Abstract
Oral vancomycin has a long history as the first-line treatment for Clostridioides difficile infection (CDI), but its use is associated with high relapse rates. Antibiotics that more selectively target C. difficile while sparing protective commensal gut bacteria, have the potential to prevent recurrent CDI (rCDI). Here, we investigate the experimental glycopeptide antibiotic, EVG7, in the context of rCDI. In vitro susceptibility assays reveal that clinical C. difficile isolates are up to 16-times more sensitive to EVG7 (MIC = 0.063–0.25 mg/L) compared to vancomycin (MIC = 0.5–2 mg/L). In a validated mouse model of rCDI in male mice, low dose oral EVG7 (0.04 mg/mL in drinking water) more effectively treats primary CDI and prevents recurrence, outperforming a 10-fold higher dose of vancomycin. Subsequent microbiome analysis and in vitro susceptibility testing reveal that EVG7 preserves Lachnospiraceae, a family of commensal bacteria associated with protection against C. difficile colonization.
Similar content being viewed by others
Introduction
Clostridioides difficile is a Gram-positive anaerobic pathogen that is the leading cause of healthcare- and antibiotic-associated diarrhea in the United States and Europe1,2,3. Clinical symptoms of C. difficile infection (CDI) range from mild diarrhea to life-threatening colitis and death4. Each year an estimated 0.5 million patients are affected by CDI in the U.S., of which 30,000 infections are lethal1. CDI also contributes to a significant demand on healthcare resources with associated costs between $71,980 (no recurrence) and $207,733 (≥3 recurrences) per patient, amounting to an annual economic burden of around $5.4 billion5. Aside from recent antibiotic exposure, patient-specific risk factors for severe CDI are hospitalization and advanced age. Infection with C. difficile typically happens by transmission of heat-, acid-, oxygen- and antibiotic-resistant spores4. These spores are not killed by routine cleaning with alcohol-based sanitizers and can survive on surfaces for several months4, which is of particular concern in hospitals and care facilities where such spores are ubiquitously present6. Intestinal colonization can be asymptomatic, but active CDI will develop when the dormant spores germinate into anaerobic, toxin-producing vegetative cells in the presence of host-derived bile salt germinants and amino acids7. Antibiotics remain a major risk factor for CDI as they disrupt the composition and function of the gut microbiome, thus generating a favorable environment for C. difficile germination, outgrowth, and toxin production8.
Despite contributing to the onset of CDI, antibiotics remain the standard of care treatment for CDI, typically as a 10-day course of oral vancomycin or fidaxomicin9,10,11. Oral vancomycin – and fidaxomicin to a lesser extent – is associated with CDI recurrence, with up to 25% of patients relapsing within 2–8 weeks after antibiotic treatment for the initial episode12. Probability of recurrence increases with each episode12 and can be attributed to disruption of the indigenous gut microbiota by these antibiotics, resulting in an altered environment that allows persistent C. difficile spores to regerminate7,13. While historically metronidazole was also used for treating CDI, increasingly poor cure rates attributed to reduced susceptibility have led to it being deprioritized in the clinical guidelines10,14,15. For fidaxomicin, reports have revealed emerging resistance in C. difficile16,17. Given that fidaxomicin only recently made it into the clinical guidelines10,15, such reports of resistance may be a cause for concern18. With regard to vancomycin, cases of reduced susceptibility leading to poorer clinical outcomes have also been reported19, however resistance to vancomycin is still uncommon in C. difficile despite a long history of use. There are also concerns that oral vancomycin can select for resistance in other gut bacteria, for example leading to further colonization with pathogenic vancomycin-resistant enterococci (VRE) or S. aureus (VRSA)20. As an alternative to traditional antibiotics for treatment of recurrent CDI (rCDI), fecal microbiota transplantation (FMT) and more recently microbiota-focused therapies and live biotherapeutic products (LBPs) have been developed21,22,23,24. However, such treatments are adjuvant at best and do not replace antibiotic therapy25,26. Furthermore, reliable access to FMT products can be challenging27,28 and the two FDA-approved microbiota-focused therapies, VOWST29 and REBYOTA30, are not approved for treatment of pediatric patients31 or patients with fulminant CDI32.
These issues underscore the need for new antibiotics that target C. difficile while sparing other members of the gut microbiota, thus preventing recurrence. Recently, we reported the discovery and development of the new glycopeptide antibiotic EVG7 that holds promise as a treatment for challenging Gram-positive infections33. Currently in preclinical development, EVG7 is a semisynthetic vancomycin derivative with an improved safety profile that outperformed vancomycin against various (drug-resistant) Gram-positive pathogens, including vancomycin-resistant strains (e.g., VRE, VRSA), with low propensity for resistance selection. EVG7 was also found to be safe and well-tolerated in murine models.
In this work, we show that EVG7 also outperforms vancomycin against a panel of different human C. difficile clinical isolates. We further show that in a validated mouse model of rCDI a lower dose of oral EVG7 effectively treats primary CDI while preventing recurrence, demonstrating superiority to standard of care vancomycin. Notably, the reduced recurrence of CDI in EVG7-treated mice is paralleled by the preservation of Lachnospiraceae, a family of commensal bacteria associated with protection against C. difficile colonization in the gut.
Results
EVG7 outperforms vancomycin against C. difficile clinical isolates
To evaluate whether EVG7 is more potent than vancomycin (VAN) against C. difficile, in vitro susceptibility was tested against a panel of clinically relevant C. difficile isolates belonging to common phylogenic clades (Fig. 1, Supplementary Table 1). Agar dilution susceptibility testing of this collection revealed MIC50-values of 1 µg/mL for vancomycin and 0.125 µg/mL for EVG7, corresponding to an 8-fold higher sensitivity to EVG7. Across all phylogenic clades tested, the C. difficile MICs for EVG7 were consistently 8-fold to 16-fold lower than for vancomycin. Notably, susceptibility was similar in clades associated with epidemics and outbreaks18, such as clade 2 – which includes PCR ribotypes (RT) 027 and 176/multilocus sequence type (ST)1 – and clade 5 which includes RT078/ST11.
Minimal Inhibitory Concentration (MIC) of vancomycin (VAN) and EVG7 against C. difficile clinical isolates, determined by agar dilution method in Brucella Blood Agar (BBA) supplemented with sheep blood, hemin, and vitamin K. The isolates tested belong to a well-established reference collection88,89 supplemented with clinical isolates collected by the National Expertise Center for C. difficile infections (hosted at the Leiden University Medical Center (LUMC), the Netherlands)106. Each dot represents the MIC value for an independent single isolate, the lines represent the geometric mean MIC value in this clade for each compound (independent biological replicates). Graphs were generated in GraphPad Prism 10 and further compiled in Adobe Illustrator 2024. Source data are provided in Supplementary Table 1 and as a Source Data file.
Oral EVG7 prevents recurrence of CDI in vivo while vancomycin does not
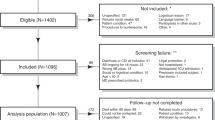
Having established its in vitro activity against C. difficile, EVG7 was further evaluated in a mouse model of rCDI (Fig. 2a). In this established model34,35,36, male mice were pretreated with the broad-spectrum antibiotic cefoperazone for five days, followed by two days on regular water, to render them susceptible to colonization. Mice were challenged with C. difficile spores on day 0 leading to established primary CDI by day 4. Next, drinking water supplemented with antibiotic (vancomycin or EVG7) was made available ad libitum for 5 days, after which antibiotic treatment was ceased and animals were monitored for clinical signs of rCDI. Clinical signs of disease were measured by monitoring weight loss (Fig. 2b) and utilizing a clinical scoring system to categorize severity of CDI (Supplementary Table 2, Fig. 2c). In this study, mice were divided into three groups: one ‘no CDI’ group (n = 4) that was not challenged with C. difficile and two antibiotic groups that were challenged with C. difficile: the comparator 0.4 mg/mL vancomycin group (VAN, n = 8), that typically relapses after 13–15 days, and the 0.04 mg/mL EVG7 group (n = 12). The 10-fold lower dose of oral EVG7 was selected in accordance with the higher in vitro sensitivity of C. difficile isolates to EVG7.
a Timeline for in vivo model of recurrent C. difficile infection (rCDI) in male C57BL/6 J mice. Following cefoperazone pretreatment, the vancomycin (VAN, n = 8 mice) and EVG7 (n = 12 mice) groups were challenged with C. difficile via oral gavage; the ‘no CDI’ group (n = 4 mice) was not challenged with C. difficile. Treatment with 0.4 mg/mL vancomycin or 0.04 mg/mL EVG7 was administered in the drinking water ad libitum from days 4–9. Mice were monitored for rCDI, which occurred on days 14 and 15 in the VAN group. b Baseline weight loss of mice in ‘no CDI’ (n = 4), VAN (n = 8), and EVG7 (n = 12) groups. Data are mean ± standard deviation. Significance comparing VAN to EVG7 was determined by two-sided mixed-effects model analysis followed by a Tukey’s posttest. c Clinical scoring of mice to monitor severity of CDI in the ‘no CDI’ (n = 4), VAN (n = 8), and EVG7 (n = 12) groups. Clinical score chart provided in Supplementary Table 2. Visual presentation and statistics as described for (b). d Total spores and vegetative cells of C. difficile in colony-forming units (CFUs) per gram of fecal content in the VAN (n = 8) and EVG7 (n = 12) groups. Each dot represents an individual fecal sample, bars represent the mean with error bars showing the standard deviation. Stool was not collected from deceased or very sick animals. Values below LOD were set to 1000. Significance and statistics as described for (b). e Total spores and vegetative cells of C. difficile in CFUs per gram of cecal content on day 14/15 (VAN, n = 6) or day 18 (EVG7, n = 12) (P < 0.0001). Each dot represents an individual cecal sample, bars represent the mean with error bars showing the standard deviation. Values below LOD were set to 1000. Significance was determined by a two-sided Mann-Whitney test. f Toxin activity in cecal content as determined by Vero cell cytotoxicity assay (P < 0.0001). Visual presentation and statistics as described for (e). The dashed line represents the limit of detection for the toxin activity (reciprocal log titer). For all statistical tests: *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. Graphs were generated in GraphPad Prism 10 and further compiled in Adobe Illustrator 2024. Source data are provided as a Source Data file.
As expected, both antibiotic-treated groups exhibited weight loss (Fig. 2b) and clinical signs of disease (Fig. 2c) in the first four days following C. difficile spore challenge, signifying primary CDI. However, mice receiving 0.4 mg/mL vancomycin in their drinking water slowly started to show clinical signs of relapse after antibiotic treatment was halted on day 9, including significant weight loss compared to both the ‘no CDI’ and EVG7 groups (P ≤ 0.0001), and had to be euthanized on day 14/15. While the total C. difficile load (vegetative cells and spores) in the feces was lowered almost to the limit of detection of 103 colony forming units (CFUs) (Fig. 2d) during treatment, by day 13 C. difficile levels exceeded pretreatment levels in the VAN group as the animals started relapsing. The high C. difficile bacterial load (Fig. 2e) and toxin activity (Fig. 2f) in cecal content confirmed recurrence of CDI in the VAN group. By comparison, none of the animals in the EVG7 group showed clinical signs of disease post-treatment. Interestingly, the total C. difficile load (vegetative cells and spores) in feces during EVG7 treatment was below the limit of detection and only became detectable again at day 11 (after treatment was stopped) (Fig. 2d). Furthermore, up to the end of the study, C. difficile levels stayed below pretreatment levels, and were significantly lower than in the relapsing VAN group (P ≤ 0.0001). On the day of necropsy (day 14/15 for VAN, day 18 for EVG7), the cecal contents of EVG7-treated mice contained a significantly lower C. difficile load (P ≤ 0.0001) (Fig. 2e) and toxin activity (P ≤ 0.0001) (Fig. 2f) compared to the vancomycin-treated mice. Altogether, this study indicates that 0.04 mg/mL EVG7 effectively treated the primary CDI while preventing recurrence.
To assess the impact of EVG7 dose level, we also ran the rCDI mouse model using high (0.4 mg/mL) and low (0.04 mg/mL) doses of EVG7 and vancomycin (Supplementary Fig. 1). Mice were divided into five groups of four animals (Supplementary Fig. 1a): a control group (‘no CDI’) that was not challenged with C. difficile; and four groups that received antibiotic in their drinking water from day 4–9: 0.04 mg/mL vancomycin (VAN low); 0.4 mg/mL vancomycin (VAN high); 0.04 mg/mL EVG7 (EVG7 low); and 0.4 mg/mL EVG7 (EVG7 high). All animals were euthanized on day 14, when the first group (VAN low) relapsed (Supplementary Fig. 1b), to allow for direct comparison of C. difficile burden and toxin activity in cecal content across all groups. During antibiotic treatment, both groups treated with 0.04 mg/mL antibiotic saw a reduction in fecal C. difficile levels. C. difficile burden remained low for 0.04 mg/mL EVG7-treated mice (EVG7 low) after discontinuation of treatment, whereas the mice treated with the same dose of vancomycin (VAN low) showed clear clinical signs of disease and recurrence upon treatment cessation (Supplementary Fig. 1b, c). This was further confirmed by high cecal C. difficile burden (Supplementary Fig. 1d) and toxin activity (Supplementary Fig. 1e) detected for the VAN low group. Compared to low dose VAN and EVG7 groups, treatment with 0.4 mg/mL vancomycin (VAN high) or EVG7 (EVG7 high) resulted in further lowering of fecal C. difficile levels (below detection limit) while drinking water was supplemented with either antibiotic. However, by day 14 C. difficile was detectable in feces for both high dose groups (Supplementary Fig. 1c). Interestingly, evaluation of cecal C. difficile burden (Supplementary Fig. 1d) and cecal toxin activity (Supplementary Fig. 1e) indicates that high dose EVG7 is less effective than low dose EVG7, while the opposite is true for the vancomycin groups. The finding that low dose EVG7 is superior to high dose EVG7 speaks to the possibility that above a certain threshold concentration EVG7 may begin to also eliminate commensal bacteria associated with protection against C. difficile colonization and relapse (vide infra).
Low dose oral EVG7 targets C. difficile while sparing gut microbes from the Lachnospiraceae family
To define changes in the gut microbiome composition between 0.4 mg/mL vancomycin (VAN) and 0.04 mg/mL EVG7 treatment groups (Fig. 2), DNA isolated from the mouse cecal content was characterized by 16S rRNA Illumina sequencing (Fig. 3). Principal Coordinates Analysis (PCoA) revealed that the gut microbiota profiles of each antibiotic treatment formed a distinct cluster with significant dissimilarity (P = 0.001) to the other treatment group (Fig. 3a). One of the hallmarks of a healthy gut microbiome is a high microbial diversity and richness37. Compared to the relapsing vancomycin-treated mice, the cecal content in the EVG7-treated mice had a significantly higher Shannon diversity (Fig. 3b; P = 0.0001) and Chao1 richness (Fig. 3c; P = 0.0009). Furthermore, the lower relative abundance of the Clostridioides amplicon sequence variant (ASV) in EVG7-treated mice compared to vancomycin-treated mice (Fig. 3d; P = 0.0001) is in agreement with the lower C. difficile CFUs and toxin activity in cecal content (Fig. 2e, f). Specifically, an increased abundance of ASVs belonging to Lachnospiraceae and Bifidobacteriaceae family members was found in the core microbial cecal content of EVG7-treated mice compared to the vancomycin group, whereas ASVs of Lactobacillaceae and Enterococcaceae were overrepresented in the vancomycin-treated mice (Fig. 3e). Members of the Lachnospiraceae family are associated with resistance against C. difficile colonization and are among the gut microbiota that are considered protective against CDI38,39,40 whereas Lactobacillaceae and Enterococcaceae are among the taxa positively correlated with C. difficile colonization38. Mouse fecal samples also reveal obvious changes in microbial community structures during and after treatment with vancomycin or EVG7 (Fig. 3f, g). Principal response curve analysis (Fig. 3f) showed time-dependent antibiotic treatment effects and revealed that the EVG7-treated mice start to deviate from the vancomycin-treated mice during treatment. Specifically, the negative taxon weights of Enterococcaceae and Akkermansiaceae suggest a decreased absolute abundance in the EVG7-treated mice compared to the vancomycin-treated mice. Conversely, the absolute abundance of Oscillospiraceae, Clostridia UCG-014, and the protective taxa Lachnospiraceae and Ruminococcaceae increased in response to EVG7 treatment, with Lachnospiraceae mainly driving microbiota changes due to antibiotic treatment. The longitudinal analysis (Fig. 3g) revealed a similar increase in relative abundance of Lachnospiraceae in feces during and after EVG7 treatment, whereas a strong decrease was observed during vancomycin treatment. Taken together, these data in EVG7-treated mice indicate preservation of Lachnospiraceae family members who are associated with protection against C. difficile colonization in the gut.
Microbiome analysis of DNA extracted from cecal content samples (a–e)) of 0.4 mg/mL vancomycin-treated (VAN) mice (on day 14/15, n = 6 mice) and 0.04 mg/mL EVG7-treated mice (on day 18, n = 12 mice) or from fecal samples collected on various days (f, g)). Data accompanying Fig. 2. a Principal Coordinates Analysis (PCoA) plot based on Aitchison’s distances between cecal content samples. The variance contribution of the first and second principal coordinates is shown on the x- and y-axis, respectively. Each point represents the microbial community of an individual sample. Ellipses correspond to 95% confidence regions. The significance of the clustering (P = 0.001) was calculated with permutational multivariate analysis of variance (PERMANOVA). b Shannon diversity in cecal content (P = 0.0001). Significance was determined by a two-sided Mann-Whitney test. Box plots show the median (center line), the first and third quartiles (bounds of the box). Whiskers to show the 1.5 of the IQR. Asterisks indicate statistical significance: ***P ≤ 0.001; ****P ≤ 0.0001. Each dot represents an individual cecum sample. c Chao1 richness in cecal content (P = 0.0009). Visual presentation and statistics as described for (b). d Relative abundance of the C. difficile ASV in cecal content (P = 0.0001). Visual presentation and statistics as described for (b). e Heatmap representing the core ASVs detected in the cecal content. The core is defined by a 0.01 detection and a 0.3 prevalence threshold. The heatmap color represents centered log-ratio (CLR) transformed ASV relative abundances. The bar plot insert depicts the prevalence of the ASV. Treatments are clustered based on hierarchical clustering using Euclidean distance. f Principal response curve showing time-dependent antibiotic treatment effects in feces of VAN (reference line) and EVG7 groups. Absolute abundances were log10 transformed. Taxa with bk values above 0.3 or below −0.3 are displayed. g Longitudinal relative abundance of Lachnospiraceae family members in feces. Each point represents an individual stool sample. The measure of center of the regression line is fitted with a smooth local regression (LOESS), error bands indicate a 95% confidence interval. Graphs were generated in R99 v4.1.2 and further compiled in Adobe Illustrator 2024. Source data are provided as a Source Data file.
EVG7 exhibits an activity spectrum supportive of C. difficile eradication while preserving commensal gut bacteria
To further characterize the different impact of EVG7 versus vancomycin on the gut microbiome, their in vitro antimicrobial activities were evaluated against a panel of clinical commensal anaerobes comprised of representative Gram-positive and Gram-negative species (Fig. 4). Notably, the Lachnospiraceae family members that were identified in the mouse microbiome (Fig. 3) do not have cultured isolates in public repositories and we therefore included a number of unclassified Lachnospiraceae in the panel. Among the Gram-positive clinical isolates screened, the MIC values for EVG7 were typically four- to eight-fold lower than for vancomycin (Fig. 4, Supplementary Table 3). All Clostridiaceae species (C. hylemonae, C. ramosum, and C. scindens) demonstrated a four- to eight-fold higher sensitivity to EVG7, mirroring the susceptibility of Clostridioides. Inhibition of commensal Clostridial bacteria may negatively affect clinical outcome as specific strains have been associated with (bile acid-dependent and -independent) resistance to CDI41,42,43,44,45. However, in our studies C. difficile (MIC = 0.125–0.25 µg/mL) is more sensitive to EVG7 than C. scindens (MIC = 0.5 µg/mL) and C. ramosum (MIC = 1 µg/mL). Whether inhibition of commensal could affect clinical outcomes warrants further investigation. In contrast, the EVG7 MICs measured for the Lachnospiraceae isolates were only two- to four-fold lower than the vancomycin MICs. Interestingly, in case of vancomycin, the Lachnospiraceae (MIC = 0.25–0.5 µg/mL) were found to be consistently more sensitive than the C. difficile isolates (MIC = 1 µg/mL), an effect not observed for EVG7. These findings indicate that upon treatment with vancomycin, Lachnospiraceae species will likely be lost before C. difficile is impacted.
Minimal Inhibitory Concentration (MIC) of vancomycin (VAN) and EVG7 against commensal clinical isolates determined by agar dilution method on Fastidious Anaerobe Agar with Horse Blood (FAA-HB)16. All isolates in this panel have been obtained from public repositories (as indicated by their catalog number) or isolated from human donors at the Leiden University Medical Center (LUMC) in the Netherlands. Source data are provided in Supplementary Table 3.
Among the Gram-negative commensal isolates tested, all were resistant to vancomycin (MIC ≥ 32 µg/mL) (Fig. 4, Supplementary Table 3). Gram-negative bacteria are intrinsically resistant to vancomycin, because it is unable to penetrate the outer membrane, preventing access to its target lipid II, located on the inner membrane in the periplasm46. Approaches to potentiate vancomycin (derivatives) against Gram-negative bacteria include disruption of the outer membrane47,48 or conjugation of cationic residues49,50,51 to facilitate translocation across the outer membrane. In the case of EVG7, most Gram-negative commensals were also resistant to EVG7 (MIC > 16 µg/mL) with some notable exceptions. Specifically, three commensal anaerobic Gram-negative isolates were found to be susceptible to EVG7; ranging from the moderately sensitive A. onderdonkii (MIC = 8 µg/mL) to the more highly sensitive P. clara (MIC = 0.25 µg/mL) and A. muciniphila (MIC = 0.25 µg/mL).
Discussion
Oral vancomycin effectively treats active C. difficile infection (CDI) yet is often associated with recurrence of CDI that is attributed to continued disruption of the indigenous gut microbiota13. Recurrence is generally lower in fidaxomicin-treated patients, an effect that may stem from inhibition of spore formation52 and sparing protective commensal members of the anaerobic gut microbiota53,54. However, similar recurrence rates have been reported in patients treated with fidaxomicin or vancomycin for infections caused by the hypervirulent BI/NAP1/027 strain55. Unlike fidaxomicin, sub-MIC concentrations of vancomycin do not significantly affect C. difficile sporulation52. Similarly, EVG7 (at 0.125× MIC) does not significantly reduce spore formation in C. difficile strain 630Δerm56,57 (data not shown). These findings indicate that EVG7 does not prevent recurrence of CDI by inhibition of sporulation, but by sparing of members of the protective gut microbiota (vide infra). As a last resort treatment after multiple recurrences, fecal microbiota transplantation (FMT) – the introduction of fecal matter from healthy donors into the patients’ gastrointestinal tract to restore a healthy gut microbiome – is used for CDI management with reported recurrence prevention of 80–90%58,59. Given that FMT products are manufactured from human stool, they have a variable donor-dependent composition60 and carry a risk of inadvertent transplantation of pathogenic bacteria61,62. Despite these risks, FMT is the only non-antibiotic treatment option for pediatric rCDI patients31 and patients with fulminant CDI32,63. However, with the leading US stool bank OpenBiome suspending distribution of FMT products late 202427,28, availability of screened donor stool for FMT has become limited. The advent of alternative microbiota-focused therapies might overcome these difficulties21,22,24. Nevertheless, these treatments do not replace antibiotic therapy as they require a neoadjuvant antibiotic course23. Also, while the FDA-approved VOWST29 and REBYOTA30 are indicated for adult rCDI, neither have been approved for treatment of fulminant CDI or pediatric patients, leaving an urgent gap in treatment.
There is a clear need for antibiotics that support microbiome conservation and stewardship – i.e. that spare the indigenous gut microbiome64. Disruption of the gut microbiome renders the patient susceptible to subsequent microbial infections65 and may also affect host physiology and immune function66 with altered gut microbiome composition found in various diseases37,67. Despite the clear clinical need, the pipeline for novel antibiotics that treat and prevent rCDI while sparing the gut microbiome is relatively dry18,68,69. The WHO reported only five traditional antibiotics in clinical development for CDI in their 2023 report70 and development of ridinilazole (SMT19969)71,72 and oxaquin (DNV3837)73 has since been discontinued. The remaining three drug candidates in active development all prevented CDI recurrence in Phase 2 trials, but only CRS3123 (REP 3123)74,75 and ibezapolstat (ACX-362E)76 showed preservation of intestinal microbiota compared to vancomycin, while recurrence prevention by MGB-BP-377 was attributed to its fast bactericidal effect rather than sparing the gut microbiome. Based on reports describing the in vitro activity of these clinical candidates78,79, EVG7 appears to possess superior activity against C. difficile. The reported in vitro potency against C. difficile clinical isolates for CRS3123 (MIC 0.5–1 µg/mL)78 and ibezapolstat (MIC 1–8 µg/mL)79 is similar to vancomycin (MIC 0.5–2 µg/mL), while EVG7 (MIC 0.063–0.25 µg/mL) is more potent (Fig. 1). Similar to CRS312374,80 and ibezapolstat81,82, EVG7 spares beneficial gut commensal bacteria, most notably members of the Lachnospiraceae and Oscillospiraceae families. In all cases, new antibiotic therapies for CDI will be compared to the standard of care vancomycin. In our current work, we demonstrate that oral administration of the new experimental glycopeptide EVG7 effectively treats primary CDI in a murine model (Fig. 2). When dosed orally at 0.04 mg/mL, EVG7 was more effective than a 10-fold higher dose of oral vancomycin in the prevention of CDI relapse, thus demonstrating superiority over the standard of care.
Protection against recurrent CDI requires sufficient preservation of the gut microbiome during antibiotic treatment. The Lachnospiraceae are a family of obligate anaerobic Gram-positive bacteria belonging to the Clostridia cluster XIVa83 and are among the microbial taxa associated with protection against C. difficile in both mice and humans38,39,40. Our data (Fig. 3) indicate that treatment with a low dose of oral EVG7 (0.04 mg/mL) prevents disease recurrence in a murine model of rCDI by the sparing of Lachnospiraceae. Mice colonized by Lachnospiraceae are less likely to develop CDI38 and administration of specific murine Lachnospiraceae isolates has also been shown to protect against C. difficile colonization in murine CDI models84,85. In humans, the presence of Lachnospiraceae was negatively correlated with C. difficile colonization in both healthy adults and fecal transplant patients38. Furthermore, the protective potential of Lachnospiraceae for treatment of rCDI is exploited in multiple microbiota-focused products currently approved or in clinical trails86 with 36% of the genera in the recently FDA-approved VOWST being Lachnospiraceae87. In this regard, the maintenance of Lachnospiraceae species in the context of CDI treatment with low dose oral EVG7 is promising. Based on the findings here reported, EVG7 warrants further investigation as an alternative to oral vancomycin therapy in the treatment of CDI and the prevention of recurrence.
Methods
Materials and resources
A list of the reagents used in this study is provided in Supplementary Table 4. Bacterial isolates used in this study are available upon reasonable request to W.K.S. Samples of the experimental antibiotic EVG7 are available upon request to N.I.M.
Minimum inhibitory concentration (MIC) assays (agar dilution)
Antibiotic preparation
Solutions of vancomycin (Applichem, A1839) and EVG7 (Leiden University, in-house synthesis33) were prepared from dry solid powder. Stock solutions of vancomycin (6.4 mg/mL) and EVG7 (3.2 mg/mL) were prepared in distilled water, filter-sterilized, and stored at −20 °C until use. The final concentrations of the antimicrobials in the agar dilution experiments were 0.25–64 mg/L for vancomycin and 0.125–32 mg/L for EVG7.
C. difficile isolates
The Clostridioides difficile isolates tested belong to a well-established reference collection88,89 supplemented with clinical isolates collected by the National Expertise Center for C. difficile infections (hosted at the Leiden University Medical Center (LUMC), Leiden, NL).
Commensal isolates
Gut microbiome commensal strains were isolated from healthy human donor feces at the Experimental Bacteriology laboratory at the LUMC (Leiden, NL). Though strains were isolated on different culture media, all demonstrated robust growth on Fastidious Anaerobe Agar supplemented with horse blood. All strains were identified by standard procedures (including Bruker Biotyper and 16S rRNA sequencing) and stored in glycerol broth at −70 °C until use.
Agar dilution MIC assay
Minimum inhibitory concentrations (MICs) for C. difficile were determined at the LUMC (Leiden, NL) using a modified Clinical and Laboratory Standard Institute (CLSI) agar dilution method as previously reported16. Briefly, C. difficile isolates were removed from −80 °C storage and subcultured anaerobically on Tryptic Soy Sheep Blood Agar plates (TSS; bioMérieux, 43009) for 48 h, prior to inoculation of pre-reduced Schaedler’s anaerobic broth (ThermoFisher Oxoid, CM0497B) for 24 h. Isolates were transferred to pre-reduced sterile saline (Supelco, 1.06404.1000) and adjusted to McFarland standard 1.0. Non-antibiotic-containing plates were incubated aerobically and anaerobically. Test medium used for C. difficile strains (Fig. 1) was Brucella Blood Agar (BBA; ThermoFisher Oxoid, CM0169) supplemented with 5% (v/v) sheep blood (Xebios Diagnostics, 10000100/10000250), 0.1 g/L hemin (SigmaAldrich, 51280), and 0.01 g/L vitamin K1 (Carl Roth, 3804.2). Minimum inhibitory concentrations (MICs) for the panel of commensal isolates (Fig. 4) were determined at the LUMC (Leiden, NL) using methods recommended by EUCAST (www.eucast.org, v15.0), using Fastidious Anaerobe Agar (FAA; Neogen, NCM0014a) supplemented with 5% (v/v) horse blood (Xebios Diagnostics, 2000100). C. difficile was included in these experiments as a control strain as well. Bacterial suspensions were inoculated onto agar plates using a multipoint inoculator and incubated anaerobically at 37 °C for 48 h. The minimum inhibitor concentration was defined as the lowest dilution at which growth is completely inhibited or where only a single colony remains16.
Murine model of recurrent C. difficile infection (rCDI)
Antibiotic preparation
Color- and odorless solutions of vancomycin (Sigma Aldrich, V2002) and EVG7 (Leiden university, in-house synthesis33) in drinking water (Gibco Laboratories, 15230) were prepared from solid dry powder and stored at 4 °C for a maximum of 7 days.
Spore preparation
C. difficile spores were prepared as previously described in ref. 90. Briefly, C. difficile was grown at 37 °C anaerobically for 1 week in Clospore media (in-house preparation91). Spores were harvested by centrifugation and washed with water, heat treated for 20 min at 65 °C, and were stored at 4 °C. Spores were plated on Brain Heart Infusion (BHI; BD Life Sciences, 241810) and Taurocholate BHI (TBHI; in-house preparation90) to make sure no viable cells were present.
Animals and housing
Animal experiments were conducted in the Laboratory Animal Facilities located on the North Carolina State University (NCSU) College of Veterinary Medicine (CVM) campus (Raleigh, USA). C57BL/6 J mice (male, 4–5 weeks old) purchased from Jackson Laboratories were used for the experimental infections. Mice were housed in cages of four animals with autoclaved bedding and water, and irradiated food. Cage changes were performed weekly in a laminar flow hood. All mice were subjected to a 12-hour light and 12-hour dark cycle, with an average temperature of 70 °F and 35% humidity.
C. difficile infection and sample collection
Groups of 4–5-week-old, male C57BL/6 J mice (Jackson Laboratories, 664) were given 0.5 mg/mL cefoperazone (MP Biomedicals, 02199695-CF) in drinking water ad libitum for 5 days to render them susceptible to C. difficile infection90. This was followed by a 2-day washout with regular drinking water (Gibco Laboratories, 15230). On day 0 all mice, excluding the’no CDI’ control group, were challenged via oral gavage with approximately 105 C. difficile 630 spores. All mouse stool tested culture negative for C. difficile before the challenge. From days 4–9, the mice were treated as follows based on their experimental group in study I (Fig. 2) and study II (Supplementary Fig. 1):
(1) ‘no CDI’ uninfected control (n = 4 in study I; n = 4 in study II) – not challenged with C. difficile and not given any additional antibiotic on day 4;
(2) VAN high (n = 8 in study I; n = 4 in study II) – challenged with C. difficile, given 0.4 mg/mL vancomycin in drinking water ad libitum;
(3) VAN low (n = 4 in study II) – challenged with C. difficile, given 0.04 mg/mL vancomycin in drinking water ad libitum;
(4) EVG7 high (n = 4 in study II) – challenged with C. difficile, given 0.4 mg/mL EVG7 in drinking water ad libitum;
(5) EVG7 low (n = 12 in study I; n = 4 in study II) – challenged with C. difficile, given 0.04 mg/mL EVG7 in drinking water ad libitum.
C. difficile infection and recurrence progression/status of the mice was monitored closely starting on day 0 by weighing the mice daily and observing and recording the clinical signs of disease for up to 18 days post challenge. An adjusted CDI clinical scoring chart (Supplementary Table 2) was used in the assessment of the clinical signs of disease in the mice and the information as used in determining severity of the disease92. Fecal pellets were collected on day −7, −2, 0, 1, 4, 5, 6, 7, 9, 11, 13, 14 in study I and II, and additionally on day 8, 15, 16, 17, and 18 in study I. Fecal pellets were stored at −80 °C until further analysis. Stool collection was not possible for all animals on some days, because sick animals often do not defecate: details and exceptions are provided in the ‘Source Data document’. Animals were humanely euthanized by CO2 asphyxiation followed by cervical dislocation prior to necropsy. Animals that expired before the end of the study were not necropsied: details are provided in the ‘Source Data document’. During necropsy, content and tissue snips were taken from the cecum and flash frozen in liquid nitrogen then stored at −80 °C until further analysis. Some of the cecal content that was collected was used for bacterial enumeration on the day of necropsy, and later 16S rRNA sequencing analysis.
C. difficile infection clinical signs scoring
The clinical scoring chart was developed for the detection and assessment of clinical signs of disease in mice that are known to have been infected by C. difficile. There are five areas of typical clinical signs of CDI that are assessed for this chart: weight loss, energy level/activity, posture, coat cleanliness, and presence of diarrhea. Each area is scored from 0 to 3 according to the chart (Supplementary Table 2) adjusted from Warren et al.92, with 0 showing no clinical signs and 3 showing severe clinical signs, all scores are added together for a full assessment. An overall score of ≤3 is not specifically indicative of signs of disease of CDI and any physical signs of sickness could be due to either stress or another condition (such as dehydration or malocclusion). An overall score of 4–7 is indicative that the mouse is showing signs of CDI but is not necessarily severely impacted by the disease. A score of 8–11 is indicative that the mouse has severe signs of disease associated with CDI and should be monitored closely and considered for euthanasia if signs appear to worsen. An overall score of ≥12 is indicative of very severe signs of disease of CDI, the mouse can often be considered moribund at this level, and euthanasia should be strongly considered. If the mouse reaches at least 20% weight loss from the day 0 baseline weight at any time then it has reached the humane endpoint in accordance with the protocol and should be euthanized.
Bacterial enumeration of C. difficile in stool and cecal content
Bacterial enumeration was performed at NCSU (Raleigh, USA) on both fecal pellets and cecal content as reported in Winston et al.90. Feces were diluted (1:10 based on weight) with phosphate-buffered saline (PBS; ThermoFisher, 10-010-049) to resuspend the samples. Samples were then incubated anaerobically for 30 min to allow the contents to settle. Ten-fold serial dilutions were performed for each sample in 1× PBS and was plated on the C. difficile-selective medium: Taurocholate, Cefoxitin, Cycloserine, and Fructose Agar (TCCFA; preparation as previously reported90) to determine the total number of both vegetative cells and spores present. All agar plates were incubated at 37 °C for 24 h. Bacterial load was expressed as colony-forming units CFUs/gram of feces or cecal content. Samples with burden below limit of detection (LOD) were given a value of 103 CFU/g for graphical and statistical purposes.
Vero cell cytotoxicity assay
Toxin activity was measured at NCSU (Raleigh, USA) using a Vero cell cytotoxicity assay as reported in Winston et al.90. Vero cells are grown and maintained in DMEM media (Gibco laboratories, 11965-092) with 10% heat-inactivated fetal bovine serum (FBS; Gibco Laboratories, 16140-071) and 1% penicillin-streptomycin solution (Gibco Laboratories, 15070-063). Cells were incubated with 0.25% trypsin (Gibco Laboratories, 25200-056), washed with DMEM media, and harvested by centrifugation at 250 × g for 5 min. Plates were seeded at 1 × 104 cells per well in a 96-well flat-bottom microtiter plate (Costar Corning, CL3595) and incubated overnight at 37 °C/5% CO2. The cecal content was diluted (1:10 by weight) with PBS and filtered before testing. The samples were further diluted 10-fold to a maximum of 10−6. Sample dilutions were incubated 1:1 with PBS (for all dilutions) or antitoxin (TechLabs, T5000) for 40 min at room temperature. Following the incubation, these mixtures were added to the Vero cells and plates were incubated overnight at 37 °C/5% CO2. Vero cells were viewed under 200× magnification and evaluated for rounding after overnight incubation. The cytotoxic titer was defined as the reciprocal log of the highest dilution that produced rounding in 80% of Vero cells for each sample. Values below LOD were set to 1 for graphical and statistical purposes. Vero cells treated with purified C. difficile toxin A (List Biological Labs, 152 C) were used as controls.
16S rRNA Illumina sequencing
DNA was isolated from feces and cecal snips (from study I) at the University of Michigan Microbial Systems Molecular Biology Laboratory (Ann Arbor, USA). The Mag Attract Power Microbiome kit (Mo Bio Laboratories, Inc) was used to isolate DNA from cecal snips. Dual-indexing sequencing approach was used to amplify the V4 region of the 16S rRNA gene. Each PCR mixture contained 2 µL of 10× Accuprime PCR buffer II (Life Technologies, CA, USA), 0.15 µL of Accuprime high-fidelity polymerase (Life Technologies, CA, USA), 5 µL of a 4.0 µM primer set, 1 µL DNA, and 11.85 µL sterile nuclease-free water. The template DNA concentration was 1–10 ng/µL for a high bacterial DNA/host DNA ratio. The PCR conditions were as follows: 2 min at 95 °C, followed by 30 cycles of 95 °C for 20 s, 55 °C for 15 s, and 72 °C for 5 min, followed by 72 °C for 10 min. Libraries were normalized using a Life Technologies SequalPrep normalization plate kit (Life Technologies, CA, USA) as per the manufacturer’s instructions for sequential elution. The concentration of the pooled samples was determined using the Kapa Biosystems library quantification kit for Illumina platforms (Kapa Biosystems, MA, USA). Agilent Bioanalyzer high-sensitivity DNA analysis kit (Agilent, CA, USA) was used to determine the sizes of the amplicons in the library. The final library consisted of equal molar amounts from each of the plates, normalized to the pooled plate at the lowest concentration. Sequencing was done on the Illumina MiSeq platform, using a MiSeq reagent kit V2 (Ilumina, CA, USA) with 500 cycles according to the manufacturer’s instructions, with modifications. Sequencing libraries were prepared according to Illumina’s protocol for preparing libraries for sequencing on the MiSeq (Ilumina, CA, USA) for 2 or 4 nM libraries. PhiX and genomes were added in 16S amplicon sequencing to add diversity. Sequencing reagents were prepared according to the Schloss SOP, and custom read 1, read 2 and index primers were added to the reagent cartridge. FASTQ files were generated for paired end reads.
Microbiome data analysis
Taxonomic profiling
The demultiplexed 16S rRNA gene amplicon sequences were filtered using “trimmomatic”93 v0.36. Filtered sequences were processed with QIIME 294 v2024.10 to produce amplicon sequence variants (ASVs). In brief, reads were denoised with the DADA2 plugin95 and taxonomies were assigned against the SILVA 138 database using the 99% OTUs full-length sequences Naive Bayes classifier with the classify-sklearn algorithm in the feature-classifier plugin96,97,98. Further processing was done using R99 v4.1.2.
PCoA
The base R “cmdscale” function and the R “phyloseq” package100 v1.38.0 were used to perform and visualize PCoA ordination with Aitchison’s distance of cecum samples. Euclidean distance was calculated for CLR-transformed ASV read counts with the “phyloseq” package100 v1.38.0.
Microbiota ecological characteristics
The “alpha” function of the R package “microbiome”101 v1.16.0 was used to calculate Shannon diversity and Chao1 richness based on rarified ASV abundance profiles of each sample. Samples were rarified to an even depth (minimum number of reads detected) with the R “phyloseq” package100 v1.38.0.
Heatmap
The core was determined on ASV relative abundance profiles with the “core” function in the R “microbiome” package v1.16.0 with a 0.01 detection threshold and a 0.3 prevalence threshold. Core ASV relative abundances were CLR-transformed and visualized with the “comp_heatmap” function of the R “microViz” package102 v0.9.3.
Principal response curve
Principal response curve analysis was performed on log10-transformed absolute abundances of families using the “prc” function of the R package “vegan”103 v2.6-4 using symmetric scaling. Stool samples from day 18 of the EVG7-treated mice were excluded from this analysis. The R “ggvegan” package104 v0.1.999 was used for visualization.
Longitudinal analyses
The regression line for relative abundance of Lachnospiraceae family members on various days was plotted for vancomycin-treated mice and EVG7-treated mice with the “geom_smooth” function of the “ggplot2” package105 v3.3.6 using the default smooth local regression (LOESS).
Statistical analyses
Statistical analyses of in vivo study data (Fig. 2 and Supplementary Fig. 1) were performed using GraphPad Prism 10 v.10.3.1. For burden data, CFU values (Fig. 2d, e and Supplementary Fig. 1c, d) were transformed to log10 values for statistical analysis. Significance comparing VAN to EVG7 for baseline weight, clinical score and fecal C. difficile CFU (Fig. 2b–d) was determined by a two-sided mixed-effects model analysis followed by a Tukey’s posttest. Significance for cecal C. difficile CFU and cecal toxin activity (Fig. 2e, f) was determined by a two-sided Mann-Whitney test. Significance for cecal C. difficile CFU (Supplementary Fig. 1d) was determined by a one-sided Brown-Forsythe and Welch’s ANOVA followed by a Dunnett T3 multiple posttest. Significance for toxin activity (Supplementary Fig. 1e) was determined by a one-sided Kruskal-Wallis ANOVA followed by a Dunn’s multiple comparisons posttest. For all tests: *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001. Details are also listed in each figure legend.
Statistical analyses of microbiome data (Fig. 3) were performed using R99 v4.1.2. Significance of clustering by treatment in the PCoA (Fig. 3a) was tested with the “adonis2” function using default permutations in the R “vegan” package103 v2.6-4. Means of Shannon diversity (Fig. 3b), Chao1 richness (Fig. 3c), and Clostridioides ASV relative abundance (Fig. 3d) were compared with a two-sided Mann-Whitney test after normality was rejected with a Shapiro-Wilk’s test. The “geom_smooth” function of the “ggplot2” package105 v3.3.6 was used for a default smooth local regression (LOESS) with 95% confidence interval in the longitudinal analyses of Lachnospiraceae family members (Fig. 3g).
Ethics statement
All animal experiments were conducted in the Laboratory Animal Facilities located on the North Carolina State University (NCSU) College of Veterinary Medicine (CVM) campus (Raleigh, USA). The animal facilities are equipped with a full-time animal care staff coordinated by the Laboratory Animal Resources (LAR) division at NCSU. The NCSU CVM is accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care International (AAALAC). Trained animal handlers in the facility fed and assessed the status of animals several times per day. Those assessed as moribund were humanely euthanized by CO2 asphyxiation. This protocol is approved by NC State’s Institutional Animal Care and Use Committee (IACUC).
Bacteria isolated from human stool were used in this study (not human stool itself). These bacteria were originally isolated from stool obtained from the Netherlands Donor Feces Bank (NDFB; https://www.ndfb.nl/), independent from the present study. The NDFB obtained informed consent for the use of the fecal donor samples for research purposes under approval of the Medical Ethics Committee at Leiden University Medical Center (P15.145).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The demultiplexed 16S rRNA gene amplicon sequencing data generated in this study have been deposited in the European Nucleotide Archive under accession code PRJEB86983. Source data are provided in the Supplementary Information and the Source Data file. Source data are provided with this paper.
References
Feuerstadt, P., Theriault, N. & Tillotson, G. The burden of CDI in the United States: a multifactorial challenge. BMC Infect. Dis. 23, 132 (2023).
European Centre for Disease Control and Prevention. Clostridioides difficile infections - Annual Epidemiological Report for 2018−2020; 2024. Available from: https://www.ecdc.europa.eu/en/publications-data/clostridioides-difficile-infections-annual-epidemiological-report-2018-2020.
Guh, A.Y. et al. Trends in U.S. Burden of Clostridioides difficile Infection and Outcomes. N. Engl. J. Med. 382, 1320–1330 (2020).
Czepiel, J. et al. Clostridium difficile infection: review. Eur. J. Clin. Microbiol. Infect. Dis. 38, 1211–1221 (2019).
Feuerstadt, P. et al. Healthcare resource utilization and direct medical costs associated with index and recurrent Clostridioides difficile infection: a real-world data analysis. J. Med. Econ. 23, 603–609 (2020).
Bartlett, J. G. & Gerding, D. N. Clinical Recognition and Diagnosis of Clostridium difficile Infection. Clin. Infect. Dis. 46, S12–S18 (2008).
Zhu, D., Sorg, J. A. & Sun, X. Clostridioides difficile Biology: Sporulation, Germination, and Corresponding Therapies for C. difficile Infection. Front. Cell. Infect. Microbiol. 8, 29 (2018).
Baktash, A. et al. Mechanistic Insights in the Success of Fecal Microbiota Transplants for the Treatment of Clostridium difficile Infections. Front. Microbiol. 9, 1242 (2018).
McDonald, L. C. et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin. Infect. Dis. 66, 987–994 (2018).
Johnson, S. et al. Clinical Practice Guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 Focused Update Guidelines on Management of Clostridioides difficile Infection in Adults. Clin. Infect. Dis. 73, e1029–e1044 (2021).
Al-Jashaami, L. S. & DuPont, H. L. Management of Clostridium difficile Infection. Gastroenterol. Hepatol. 12, 609–616 (2016).
Tsigrelis, C. Recurrent Clostridioides difficile infection: Recognition, management, prevention. Clevel. Clin. J. Med. 87, 347–359 (2020).
Wang, R. Clostridioides difficile infection: microbe-microbe interactions and live biotherapeutics. Front. Microbiol. 14, 1182612 (2023).
Gonzales-Luna, A. J. et al. Reduced Susceptibility to Metronidazole Is Associated With Initial Clinical Failure in Clostridioides difficile Infection. Open Forum Infect. Dis. 8, ofab365 (2021).
van Prehn, J. et al. European Society of Clinical Microbiology and Infectious Diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin. Microbiol. Infect. 27, S1–S21 (2021).
Freeman, J. et al. Antimicrobial susceptibility testing of Clostridioides difficile: a dual-site study of three different media and three therapeutic antimicrobials. Clin. Microbiol. Infect. 6, 1011–1017 (2025).
Marchandin, H. et al. In vivo emergence of a still uncommon resistance to fidaxomicin in the urgent antimicrobial resistance threat Clostridioides difficile. J. Antimicrobial Chemother. 78, 1992–1999 (2023).
Smits, W. K., Garey, K. W., Riley, T. V. & Johnson, S. Clostridioides difficile is a bacterial priority pathogen. Anaerobe 93, 102965 (2025).
Eubank, T. A. et al. Reduced Vancomycin Susceptibility in Clostridioides difficile Is Associated With Lower Rates of Initial Cure and Sustained Clinical Response. Clin. Infect. Dis. 79, 15–21 (2024).
Fishbein, S. et al. Randomized Controlled Trial of Oral Vancomycin Treatment in Clostridioides difficile-Colonized Patients. mSphere 6, e00936–00920 (2021).
Benech, N. et al. Update on microbiota-derived therapies for recurrent Clostridioides difficile infections. Clin. Microbiol. Infect. 30, 462–468 (2024).
Pribyl, A. L., Hugenholtz, P. & Cooper, M. A. A decade of advances in human gut microbiome-derived biotherapeutics. Nat. Microbiol. 10, 301–312 (2025).
Wang, Y., Hunt, A., Danziger, L. & Drwiega, E. N. A Comparison of Currently Available and Investigational Fecal Microbiota Transplant Products for Recurrent Clostridioides difficile Infection. Antibiotics 13, 436 (2024).
McMillan, A. S. & Theriot, C. M. Bile acids impact the microbiota, host, and C. difficile dynamics providing insight into mechanisms of efficacy of FMTs and microbiota-focused therapeutics. Gut Microbes 16, 2393766 (2024).
Birch, C. R. et al. Cost-effectiveness of faecal microbiota transplantation compared with vancomycin monotherapy for early Clostridioides difficile infection: economic evaluation alongside a randomized controlled trial. J. Hospital Infect. 155, 145–149 (2025).
Baunwall, S. M. D. et al. Faecal microbiota transplantation for first or second Clostridioides difficile infection (EarlyFMT): a randomised, double-blind, placebo-controlled trial. Lancet Gastroenterol. Hepatol. 7, 1083–1091 (2022).
OpenBiome. FMT Update & Future Directions. [Press Release]; 2024. Available from https://openbiome.org/feature/fmt-update-future-directions/.
Davidson, J. OpenBiome No Longer Distributing FMT For Recurrent C. difficile Infections. [Gastroenterology & Endoscopy News]; 2024. Available from https://www.gastroendonews.com/PRN/Article/12-24/OpenBiome-No-Longer-Distributing-FMT-For-Recurrent-C-difficile-Infections/75606.
Jain, N., Umar, T. P., Fahner, A.-F. & Gibietis, V. Advancing therapeutics for recurrent clostridioides difficile infections: an overview of vowst’s FDA approval and implications. Gut Microbes 15, 2232137 (2023).
Mullard, A. FDA approves second microbiome-based C. difficile therapy. Nat. Rev. Drug Discov. 22, 436 (2023).
Shirley, D.-A., Tornel, W., Warren, C. A. & Moonah, S. Clostridioides difficile Infection in Children: Recent Updates on Epidemiology, Diagnosis, Therapy. Pediatrics 152, e2023062307 (2023).
Carlson, T. J., Gonzales-Luna, A. J. & Garey, K. W. Fulminant Clostridioides difficile Infection: A Review of Treatment Options for a Life-Threatening Infection. Semin. Respiratory Crit. Care Med. 43, 028–038 (2022).
van Groesen, E. et al. Semisynthetic guanidino lipoglycopeptides with potent in vitro and in vivo antibacterial activity. Sci. Transl. Med. 16, eabo4736 (2024).
Theriot, C. M. et al. Cefoperazone-treated mice as an experimental platform to assess differential virulence of Clostridium difficile strains. Gut Microbes 2, 326–334 (2011).
Blake, S. et al. Salicylanilide Analog Minimizes Relapse of Clostridioides difficile Infection in Mice. J. Medicinal Chem. 63, 6898–6908 (2020).
Seekatz, A. M. et al. Fecal Microbiota Transplantation Eliminates Clostridium difficile in a Murine Model of Relapsing Disease. Infect. Immun. 83, 3838–3846 (2015).
Hou, K. et al. Microbiota in health and diseases. Signal Transduct. Target. Ther. 7, 135 (2022).
Seekatz, A. M. & Young, V. B. Clostridium difficile and the microbiota. J. Clin. Investig. 124, 4182–4189 (2014).
Theriot, C. M., Bowman, A. A. & Young, V. B. Antibiotic-Induced Alterations of the Gut Microbiota Alter Secondary Bile Acid Production and Allow for Clostridium difficile Spore Germination and Outgrowth in the Large Intestine. mSphere 1, e00045–00015 (2016).
McMillan, A. S. et al. Metagenomic, metabolomic, and lipidomic shifts associated with fecal microbiota transplantation for recurrent Clostridioides difficile infection. mSphere 9, e00706–e00724 (2024).
Buffie, C. G. et al. Precision microbiome reconstitution restores bile acid mediated resistance to Clostridium difficile. Nature 517, 205–208 (2015).
Girinathan, B. P. et al. In vivo commensal control of Clostridioides difficile virulence. Cell Host Microbe 29, 1693–1708.e1697 (2021).
Kang, J. D. et al. Bile Acid 7α-Dehydroxylating Gut Bacteria Secrete Antibiotics that Inhibit Clostridium difficile: Role of Secondary Bile Acids. Cell Chem. Biol. 26, 27–34.e24 (2019).
Fishbein, S. R. S. et al. Commensal-pathogen dynamics structure disease outcomes during Clostridioides difficile colonization. Cell Host Microbe 33, 30–41.e36 (2025).
Aguirre, A. M. et al. Bile acid-independent protection against Clostridioides difficile infection. PLOS Pathog. 17, e1010015 (2021).
Walsh, C. T. et al. Bacterial resistance to vancomycin: Five genes and one missing hydrogen bond tell the story. Chem. Biol. 3, 21–28 (1996).
van Groesen, E. et al. Vancomyxins: Vancomycin-Polymyxin Nonapeptide Conjugates That Retain Anti-Gram-Positive Activity with Enhanced Potency against Gram-Negative Strains. ACS Infect. Dis. 7, 2746–2754 (2021).
Li, Q. et al. Outer-membrane-acting peptides and lipid II-targeting antibiotics cooperatively kill Gram-negative pathogens. Commun. Biol. 4, 31 (2021).
Antonoplis, A. et al. Vancomycin-Arginine Conjugate Inhibits Growth of Carbapenem-Resistant E. coli and Targets Cell-Wall Synthesis. ACS Chem. Biol. 14, 2065–2070 (2019).
Sarkar, P. et al. Vancomycin Derivative Inactivates Carbapenem-resistant Acinetobacter baumannii and Induces Autophagy. ACS Chem. Biol. 15, 884–889 (2020).
Bian, X. et al. Single Amine or Guanidine Modification on Norvancomycin and Vancomycin to Overcome Multidrug-Resistance through Augmented Lipid II Binding and Increased Membrane Activity. J. Medicinal Chem. 67, 20639–20663 (2024).
Babakhani, F. et al. Fidaxomicin Inhibits Spore Production in Clostridium difficile. Clin. Infect. Dis. 55, S162–S169 (2012).
Yamaguchi, T. et al. The gut microbiome diversity of Clostridioides difficile-inoculated mice treated with vancomycin and fidaxomicin. J. Infect. Chemother. 26, 483–491 (2020).
Louie, T. J. et al. OPT-80 Eliminates Clostridium difficile and Is Sparing of Bacteroides Species during Treatment of C. difficile Infection. Antimicrobial Agents Chemother. 53, 261–263 (2009).
Louie, T. J. et al. Fidaxomicin versus Vancomycin for Clostridium difficile Infection. N. Engl. J. Med. 364, 422–431 (2011).
van Eijk, E. et al. Complete genome sequence of the Clostridium difficile laboratory strain 630Δerm reveals differences from strain 630, including translocation of the mobile element CTn5. BMC Genomics 16, 31 (2015).
Hussain, H. A., Roberts, A. P. & Mullany, P. Generation of an erythromycin-sensitive derivative of Clostridium difficile strain 630 (630Δerm) and demonstration that the conjugative transposon Tn916ΔE enters the genome of this strain at multiple sites. J. Med. Microbiol. 54, 137–141 (2005).
Kassam, Z., Lee, C. H. & Hunt, R. H. Review of the Emerging Treatment of Clostridium difficile Infection with Fecal Microbiota Transplantation and Insights into Future Challenges. Clin. Lab. Med. 34, 787–798 (2014).
Rohlke, F. & Stollman, N. Fecal microbiota transplantation in relapsing Clostridium difficile infection. Therapeutic Adv. Gastroenterol. 5, 403–420 (2012).
Blair, H. A. SER-109 (VOWST™): A Review in the Prevention of Recurrent Clostridioides difficile Infection. Drugs 84, 329–336 (2024).
DeFilipp, Z. et al. Drug-Resistant E. coli Bacteremia Transmitted by Fecal Microbiota Transplant. N. Engl. J. Med. 381, 2043–2050 (2019).
Tan, X. & Johnson, S. Fecal microbiota transplantation (FMT) for C. difficile infection, just say ‘No’. Anaerobe 60, 102092 (2019).
Peery, A. F. et al. AGA Clinical Practice Guideline on Fecal Microbiota–Based Therapies for Select Gastrointestinal Diseases. Gastroenterology 166, 409–434 (2024).
Peixoto, R. S. et al. Harnessing the microbiome to prevent global biodiversity loss. Nat. Microbiol. 7, 1726–1735 (2022).
Khosravi, A. & Mazmanian, S. K. Disruption of the gut microbiome as a risk factor for microbial infections. Curr. Opin. Microbiol. 16, 221–227 (2013).
Durack, J. & Lynch, S. V. The gut microbiome: Relationships with disease and opportunities for therapy. J. Exp. Med. 216, 20–40 (2019).
Afzaal, M. et al. Human gut microbiota in health and disease: Unveiling the relationship. Front. Microbiol. 13, 999001 (2022).
Carlson, T. J. & Gonzales-Luna, A. J. Antibiotic Treatment Pipeline for Clostridioides difficile Infection (CDI): A Wide Array of Narrow-Spectrum Agents. Curr. Infect. Dis. Rep. 22, 20 (2020).
Quan, M. et al. Fighting against Clostridioides difficile infection: Current medications. Int. J. Antimicrobial Agents 64, 107198 (2024).
World Health Organization. 2023 Antibacterial agents in clinical and preclinical development: an overview and analysis. Available from https://www.who.int/publications/i/item/9789240094000 (2024).
Okhuysen, P. C. et al. A Randomized, Double-Blind, Phase 3 Safety and Efficacy Study of Ridinilazole Versus Vancomycin for Treatment of Clostridioides difficile Infection: Clinical Outcomes With Microbiome and Metabolome Correlates of Response. Clin. Infect. Dis. 78, 1462–1472 (2024).
Taylor, N. P. Summit makes case for changes to antibiotic R&D after sharing data from failed phase 3 trial. 2022. Available from https://www.fiercebiotech.com/biotech/summit-makes-case-changes-antibiotic-rd-after-sharing-data-failed-phase-3-trial.
DEINOVE - Update on the receivership proceedings. [Press release]; 2023. Available from https://firstwordpharma.com/story/5697000.
Lomeli, B. K. et al. Multiple-Ascending-Dose Phase 1 Clinical Study of the Safety, Tolerability, and Pharmacokinetics of CRS3123, a Narrow-Spectrum Agent with Minimal Disruption of Normal Gut Microbiota. Antimicrobial Agents Chemother. 64, e01395–01319 (2019).
Crestone Inc. Crestone Announces Positive Data from Phase 2 Clinical Trial of CRS3123 for C. Difficile Infections (CDI). [Press release]; 2024. Available from https://crestonepharma.com/positive-data-phase-2-clinical-trial-crs3123/.
Eubank, T. A. et al. P-1109. A phase 2, randomized, double-blind study of ibezapolstat compared with vancomycin for the treatment of Clostridioides difficile infection: clinical and microbiome evaluation. Open Forum Infect. Dis. 12, ofae631.1297 (2025).
MGB Biopharma. MGB Biopharma Announces Successful Outcome from Phase II Clinical Study with MGB-BP-3 – a Potential New Gold Standard, First-Line Treatment for Clostridium difficile Infection (CDI). [Press release]; 2020. Available from https://www.mgb-biopharma.com/mgb-biopharma-announces-successful-outcome-from-phase-ii-clinical-study-with-mgb-bp-3-a-potential-new-gold-standard-first-line-treatment-for-clostridium-difficile-infection-cdi/.
Critchley, I. A. et al. Spectrum of activity and mode of action of REP3123, a new antibiotic to treat Clostridium difficile infections. J. Antimicrobial Chemother. 63, 954–963 (2009).
Murray, B. et al. In vitro activity of the novel antibacterial agent ibezapolstat (ACX-362E) against Clostridioides difficile. J. Antimicrobial Chemother. 75, 2149–2155 (2020).
Citron, D. M. et al. Comparative in vitro activity of REP3123 against Clostridium difficile and other anaerobic intestinal bacteria. J. Antimicrobial Chemother. 63, 972–976 (2009).
Garey, K. W. et al. Efficacy, Safety, Pharmacokinetics, and Microbiome Changes of Ibezapolstat in Adults with Clostridioides difficile Infection: A Phase 2a Multicenter Clinical Trial. Clin. Infect. Dis. 75, 1164–1170 (2022).
McPherson, J. K. et al. The microbiome-restorative potential of ibezapolstat for the treatment of Clostridioides difficile infection is predicted through variant PolC-type DNA polymerase III in Lachnospiraceae and Oscillospiraceae. Antimicrobial Agents Chemother. 69, e01679–01624 (2025).
Vacca, M. et al. The Controversial Role of Human Gut Lachnospiraceae. Microorganisms 8, 573 (2020).
Reeves, A. E., Koenigsknecht, M. J., Bergin, I. L. & Young, V. B. Suppression of Clostridium difficile in the Gastrointestinal Tracts of Germfree Mice Inoculated with a Murine Isolate from the Family Lachnospiraceae. Infect. Immun. 80, 3786–3794 (2012).
Tejada, J. N. et al. Prevention and cure of murine C. difficile infection by a Lachnospiraceae strain. Gut Microbes 16, 2392872 (2024).
Zaplana, T., Miele, S. & Tolonen, A. C. Lachnospiraceae are emerging industrial biocatalysts and biotherapeutics. Front. Bioeng. Biotechnol. 11, 1324396 (2024).
Feuerstadt, P. et al. SER-109, an Oral Microbiome Therapy for Recurrent Clostridioides difficile Infection. N. Engl. J. Med. 386, 220–229 (2022).
Knetsch, C. W. et al. Comparative analysis of an expanded Clostridium difficile reference strain collection reveals genetic diversity and evolution through six lineages. Infect., Genet. Evolution 12, 1577–1585 (2012).
Baktash, A. et al. Comparison of Whole-Genome Sequence-Based Methods and PCR Ribotyping for Subtyping of Clostridioides difficile. J. Clin. Microbiol. 60, e01737–01721 (2022).
Winston, J. A., Thanissery, R., Montgomery, S. A. & Theriot, C. M. Cefoperazone-treated Mouse Model of Clinically-relevant Clostridium difficile Strain R20291. J. Vis. Exp. 118, e54850 (2016).
Perez, J., Springthorpe, V. S. & Sattar, S. A. Clospore: A Liquid Medium for Producing High Titers of Semi-purified Spores of Clostridium difficile. J. AOAC Int. 94, 618–626 (2011).
Warren, C. A. et al. Amixicile, a Novel Inhibitor of Pyruvate:Ferredoxin Oxidoreductase, Shows Efficacy against Clostridium difficile in a Mouse Infection Model. Antimicrobial Agents Chemother. 56, 4103–4111 (2012).
Bolger, A. M., Lohse, M. & Usadel, B. Trimmomatic: a flexible trimmer for Illumina sequence data. Bioinformatics 30, 2114–2120 (2014).
Bolyen, E. et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 37, 852–857 (2019).
Callahan, B. J. et al. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods 13, 581–583 (2016).
Bokulich, N. A. et al. Optimizing taxonomic classification of marker-gene amplicon sequences with QIIME 2’s q2-feature-classifier plugin. Microbiome 6, 90 (2018).
Robeson, M. S. et al. RESCRIPt: Reproducible sequence taxonomy reference database management. PLoS Computational Biol. 17, e1009581 (2021).
Quast, C. et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 41, D590–D596 (2012).
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/ (2021).
McMurdie, P. J. & Holmes, S. phyloseq: An R Package for Reproducible Interactive Analysis and Graphics of Microbiome Census Data. PLoS ONE 8, e61217 (2013).
Lahti, L. & Shetty, S. microbiome R package. https://doi.org/10.18129/B9.bioc.microbiome
Barnett, D. J. M., Arts, I. C. W. & Penders, J. microViz: an R package for microbiome data visualization and statistics. J. Open Source Softw. 6, 3201 (2021).
Oksanen, J. et al. vegan: Community Ecology Package. R package version 2.6-4 https://CRAN.R-project.org/package=vegan (2022).
Simpson, G. L. & Oksanen, J. ggvegan: ‘ggplot2’ Plots for the ‘vegan’ Package. R package version 0.1.999 https://gavinsimpson.r-universe.dev/ggvegan/ggvegan.pdf (2023).
Wickham, H. ggplot2: Elegant Graphics for Data Analysis. https://doi.org/10.1007/978-0-387-98141-3 (Springer-Verlag, 2009).
Ducarmon, Q. R. et al. Clostridioides difficile infection with isolates of cryptic clade C-II: a genomic analysis of polymerase chain reaction ribotype 151. Clin. Microbiol. Infect. 29, 538.e531–538.e536 (2023).
Acknowledgements
This work was funded in part by the Netherlands Organization for Scientific Research (NWO NACTAR); grants number 18504 (N.I.M.) and 20813 (N.I.M.). The authors acknowledge the Netherlands Donor Feces Bank for kindly providing a stool sample from which bacterial strains were isolated. The authors wish to acknowledge Lesley Schout for banking the isolates used for this study. Marjon Wells-Bennik and Guus Kortman (NIZO) are thanked for the early testing of EVG7 against Clostridial strains.
Author information
Authors and Affiliations
Contributions
E.M., W.K.S., C.M.T., and N.I.M. designed the study. E.M., F.M.S., and E.G. synthesized EVG7. I.M.J.G.S., A.G.R., and W.K.S. isolated clinical strains and performed in vitro susceptibility assays. C.E.P. and C.M.T. performed in vivo studies. J.E.G.H. and W.K.S. performed microbiome analysis. E.M. and J.E.G.H. prepared the first draft of the manuscript with subsequent contributions from the other authors. All authors discussed results and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
E.G. and N.I.M. are inventors on a patent application filing WO2021060980A1; title: “Antibiotic compounds”; priority date: 24 September 2019, which includes compounds described in this article. W.K.S. has performed research for Cubist Pharmaceuticals and Acurx Pharmaceuticals and received speaker fees from Promega. C.M.T. has consulted for Vedanta Biosciences, Inc., Summit Therapeutics, and Ferring Pharmaceuticals, Inc. and is on the Scientific Advisory Board for Ancilia Biosciences. All other authors declare that they have no competing interests.
Peer review
Peer review information
Nature Communications thanks Jennifer Auchtung, Dena Lyras and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mons, E., Henderickx, J.G.E., Sanders, I.M.J.G. et al. Experimental glycopeptide antibiotic EVG7 prevents recurrent Clostridioides difficile infection by sparing members of the Lachnospiraceae family. Nat Commun 16, 9017 (2025). https://doi.org/10.1038/s41467-025-64067-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-64067-w