Abstract
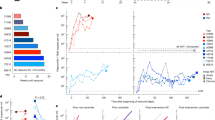
Attempts to reduce the human immunodeficiency virus type 1 (HIV-1) reservoir and induce antiretroviral therapy (ART)-free virologic control have largely been unsuccessful. In this phase 1b/2a, open-label, randomized controlled trial using a four-group factorial design, we investigated whether early intervention in newly diagnosed people with HIV-1 with a monoclonal anti-HIV-1 antibody with a CD4-binding site, 3BNC117, followed by a histone deacetylase inhibitor, romidepsin, shortly after ART initiation altered the course of HIV-1 infection (NCT03041012). The trial was undertaken in five hospitals in Denmark and two hospitals in the United Kingdom. The coprimary endpoints were analysis of initial virus decay kinetics and changes in the frequency of CD4+ T cells containing intact HIV-1 provirus from baseline to day 365. Secondary endpoints included changes in the frequency of infected CD4+ T cells and virus-specific CD8+ T cell immunity from baseline to day 365, pre-ART plasma HIV-1 3BNC117 sensitivity, safety and tolerability, and time to loss of virologic control during a 12-week analytical ART interruption that started at day 400. In 55 newly diagnosed people (5 females and 50 males) with HIV-1 who received random allocation treatment, we found that early 3BNC117 treatment with or without romidepsin enhanced plasma HIV-1 RNA decay rates compared to ART only. Furthermore, 3BNC117 treatment accelerated clearance of infected cells compared to ART only. All groups had significant reductions in the frequency of CD4+ T cells containing intact HIV-1 provirus. At day 365, early 3BNC117 + romidepsin was associated with enhanced HIV-1 Gag-specific CD8+ T cell immunity compared to ART only. The observed virological and immunological effects of 3BNC117 were most pronounced in individuals whose pre-ART plasma HIV-1 envelope sequences were antibody sensitive. The results were not disaggregated by sex. Adverse events were mild to moderate and similar between the groups. During a 12-week analytical ART interruption among 20 participants, 3BNC117-treated individuals harboring sensitive viruses were significantly more likely to maintain ART-free virologic control than other participants. We conclude that 3BNC117 at ART initiation enhanced elimination of plasma viruses and infected cells, enhanced HIV-1-specific CD8+ immunity and was associated with sustained ART-free virologic control among persons with 3BNC117-sensitive virus. These findings strongly support interventions administered at the time of ART initiation as a strategy to limit long-term HIV-1 persistence.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data are not available for download due to privacy/ethical restrictions under the EU GDPR. Specific requests for access to the trial data may be sent to olesoega@rm.dk and access may be provided to a named individual in agreement with the rules and regulations of the Danish Data Protection Agency and the National Committee on Health Research Ethics with a 2-week response timeframe to requests.
Change history
30 April 2025
In the version of the article initially published, the URL embedded in the clinical trial ID NCT03041012 was incorrect and has now been amended in the HTML and PDF versions of the article.
References
Abrahams, M. R. et al. The replication-competent HIV-1 latent reservoir is primarily established near the time of therapy initiation. Sci. Transl. Med. 11, eaaw5589 (2019).
Brodin, J. et al. Establishment and stability of the latent HIV-1 DNA reservoir. elife 5, e18889 (2016).
Martin, G. E. et al. Levels of human immunodeficiency virus DNA are determined before ART initiation and linked to CD8 T-cell activation and memory expansion. J. Infect. Dis. 221, 1135–1145 (2020).
Jones, B. R. et al. Phylogenetic approach to recover integration dates of latent HIV sequences within-host. Proc. Natl Acad. Sci. USA 115, E8958–E8967 (2018).
Brooks, K. et al. HIV-1 variants are archived throughout infection and persist in the reservoir. PLoS Pathog. 16, e1008378 (2020).
Rasmussen, T. A. et al. Panobinostat, a histone deacetylase inhibitor, for latent-virus reactivation in HIV-infected patients on suppressive antiretroviral therapy: a phase 1/2, single group, clinical trial. Lancet HIV 1, e13–e21 (2014).
Li, J. Z. et al. The size of the expressed HIV reservoir predicts timing of viral rebound after treatment interruption. AIDS 30, 343–353 (2016).
Kroon, E. D. M. B. et al. A randomized trial of vorinostat with treatment interruption after initiating antiretroviral therapy during acute HIV-1 infection. J. Virus Erad. 6, 100004 (2020).
Leth, S. et al. Combined effect of Vacc-4x, recombinant human granulocyte macrophage colony-stimulating factor vaccination, and romidepsin on the HIV-1 reservoir (REDUC): a single-arm, phase 1B/2A trial. Lancet HIV 3, e463–e472 (2016).
Gruell, H. et al. Effect of 3BNC117 and romidepsin on the HIV-1 reservoir in people taking suppressive antiretroviral therapy (ROADMAP): a randomised, open-label, phase 2A trial. Lancet Microbe 3, e203–e214 (2022).
Søgaard, O. S. et al. The depsipeptide romidepsin reverses HIV-1 latency in vivo. PLoS Pathog. 11, e1005142 (2015).
Lehrman, G. et al. Depletion of latent HIV-1 infection in vivo: a proof-of-concept study. Lancet 366, 549–555 (2005).
Archin, N. M. et al. Valproic acid without intensified antiviral therapy has limited impact on persistent HIV infection of resting CD4+ T cells. AIDS 22, 1131–1135 (2008).
Archin, N. M. et al. Antiretroviral intensification and valproic acid lack sustained effect on residual HIV-1 viremia or resting CD4+ cell infection. PLoS ONE 5, e9390 (2010).
Routy, J. P. et al. Design and implementation of a randomized crossover study of valproic acid and antiretroviral therapy to reduce the HIV reservoir. HIV Clin. Trials 13, 301–307 (2012).
Archin, N. M. et al. Administration of vorinostat disrupts HIV-1 latency in patients on antiretroviral therapy. Nature 487, 482–485 (2012).
Elliott, J. H. et al. Activation of HIV transcription with short-course vorinostat in HIV-infected patients on suppressive antiretroviral therapy. PLoS Pathog. 10, e1004473 (2014).
Archin, N. M. et al. HIV-1 expression within resting CD4+ T cells after multiple doses of vorinostat. J. Infect. Dis. 210, 728–735 (2014).
Wei, D. G. et al. Histone deacetylase inhibitor romidepsin induces HIV expression in CD4 T cells from patients on suppressive antiretroviral therapy at concentrations achieved by clinical dosing. PLoS Pathog. 10, e1004071 (2014).
Gunst, J. D., Tolstrup, M., Rasmussen, T. A. & Søgaard, O. S. The potential role for romidepsin as a component in early HIV-1 curative efforts. Expert Rev. Anti. Infect. Ther. 14, 447–450 (2016).
McMahon, D. K. et al. A phase 1/2 randomized, placebo-controlled trial of romidespin in persons with HIV-1 on suppressive antiretroviral therapy. J. Infect. Dis. 224, 648–656 (2021).
Shan, L. et al. Stimulation of HIV-1-specific cytolytic T lymphocytes facilitates elimination of latent viral reservoir after virus reactivation. Immunity 36, 491–501 (2012).
Mothe, B. et al. HIVconsv vaccines and romidepsin in early-treated HIV-1-infected individuals: safety, immunogenicity and effect on the viral reservoir (Study BCN02). Front. Immunol. 11, 823 (2020).
Fidler, S. et al. Antiretroviral therapy alone versus antiretroviral therapy with a kick and kill approach, on measures of the HIV reservoir in participants with recent HIV infection (the RIVER trial): a phase 2, randomised trial. Lancet 395, 888–898 (2020).
Caskey, M., Klein, F. & Nussenzweig, M. C. Broadly neutralizing anti-HIV-1 monoclonal antibodies in the clinic. Nat. Med. 25, 547–553 (2019).
Lu, C.-L. et al. Enhanced clearance of HIV-1–infected cells by broadly neutralizing antibodies against HIV-1 in vivo. Science 352, 1001–1004 (2016).
Dufloo, J. et al. Broadly neutralizing anti-HIV-1 antibodies tether viral particles at the surface of infected cells. Nat. Commun. 13, 630 (2022).
Schoofs, T. et al. HIV-1 therapy with monoclonal antibody 3BNC117 elicits host immune responses against HIV-1. Science 352, 997–1001 (2016).
Niessl, J. et al. Combination anti-HIV-1 antibody therapy is associated with increased virus-specific T cell immunity. Nat. Med. 26, 222–227 (2020).
Scheid, J. F. et al. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science 333, 1633–1637 (2011).
Nishimura, Y. et al. Early antibody therapy can induce long-lasting immunity to SHIV. Nature 543, 559–563 (2017).
DiLillo, D. J. & Ravetch, J. V. Differential Fc-receptor engagement drives an anti-tumor vaccinal effect. Cell 161, 1035–1045 (2015).
Gay, C. L. et al. Stable latent HIV infection and low-level viremia despite treatment with the broadly neutralizing antibody VRC07-523LS and the latency reversal agent vorinostat. J. Infect. Dis. 225, 856–861 (2022).
Gunst, J. D., Tolstrup, M. & Søgaard, O. S. Beyond antiretroviral therapy: early interventions to control HIV-1 infection. AIDS 31, 1665–1667 (2017).
Reece, J. et al. An ‘escape clock’ for estimating the turnover of SIV DNA in resting CD4+ T cells. PLoS Pathog. 8, e1002615 (2012).
Reece, J. C. et al. Measuring turnover of SIV DNA in resting CD4+ T cells using pyrosequencing: implications for the timing of HIV eradication therapies. PLoS ONE 9, e93330 (2014).
Petravic, J., Martyushev, A., Reece, J. C., Kent, S. J. & Davenport, M. P. Modeling the timing of antilatency drug administration during HIV treatment. J. Virol. 88, 14050–14056 (2014).
Baxter, A. E. et al. Multiparametric characterization of rare HIV-infected cells using an RNA-flow FISH technique. Nat. Protoc. 12, 2029–2049 (2017).
Puertas, M. C. et al. VIP-SPOT: an innovative assay to quantify the productive HIV-1 reservoir in the monitoring of cure strategies. mBio 12, e0056021 (2021).
Bruner, K. M. et al. A quantitative approach for measuring the reservoir of latent HIV-1 proviruses. Nature 566, 120–125 (2019).
Kinloch, N. N. et al. HIV-1 diversity considerations in the application of the Intact Proviral DNA Assay (IPDA). Nat. Commun. 12, 165 (2021).
Caskey, M. et al. Viraemia suppressed in HIV-1-infected humans by broadly neutralizing antibody 3BNC117. Nature 522, 487–491 (2015).
Bar-On, Y. et al. Safety and antiviral activity of combination HIV-1 broadly neutralizing antibodies in viremic individuals. Nat. Med. 24, 1701–1707 (2018).
Stephenson, K. E. et al. Safety, pharmacokinetics and antiviral activity of PGT121, a broadly neutralizing monoclonal antibody against HIV-1: a randomized, placebo-controlled, phase 1 clinical trial. Nat. Med. 27, 1718–1724 (2021).
Caskey, M. et al. Antibody 10-1074 suppresses viremia in HIV-1-infected individuals. Nat. Med. 23, 185–191 (2017).
Feng, Q. et al. Quadruple versus triple combination antiretroviral therapies for treatment naive people with HIV: systematic review and meta-analysis of randomised controlled trials. Br. Med. J. 366, 4179 (2019).
Markowitz, M. et al. A randomized open-label study of 3- versus 5-drug combination antiretroviral therapy in newly HIV-1-infected individuals. J. Acquir. Immune Defic. Syndr. 66, 140–147 (2014).
Scheid, J. F. et al. Sequence and structural convergence. Science 333, 1633–1637 (2011).
Stefic, K., Bouvin-Pley, M., Braibant, M. & Barin, F. Impact of HIV-1 diversity on its sensitivity to neutralization. Vaccines 7, 74 (2019).
Wang, P. et al. Quantifying the contribution of Fc-mediated effector functions to the antiviral activity of anti–HIV-1 IgG1 antibodies in vivo. Proc. Natl Acad. Sci. USA 117, 18002–18009 (2020).
Asokan, M. et al. Fc-mediated effector function contributes to the in vivo antiviral effect of an HIV neutralizing antibody. Proc. Natl Acad. Sci. USA 117, 18754–18763 (2020).
Veenhuis, R. T., Garliss, C. C., Bailey, J. R. & Blankson, J. N. CD8 effector T cells function synergistically with broadly neutralizing antibodies to enhance suppression of HIV infection. Front. Immunol. 12, 708355 (2021).
Spencer, D. A. et al. Phagocytosis by an HIV antibody is associated with reduced viremia irrespective of enhanced complement lysis. Nat. Commun. 13, 662 (2022).
Chomont, N. et al. HIV reservoir size and persistence are driven by T cell survival and homeostatic proliferation. Nat. Med. 15, 893–900 (2009).
Hiener, B. et al. Identification of genetically intact HIV-1 proviruses in specific CD4+ T cells from effectively treated participants. Cell Rep. 21, 813–822 (2017).
Buzon, M. J. et al. HIV-1 persistence in CD4+ T cells with stem cell-like properties. Nat. Med. 20, 139–142 (2014).
Jaafoura, S. et al. Progressive contraction of the latent HIV reservoir around a core of less-differentiated CD4+ memory T cells. Nat. Commun. 5, 5407 (2014).
Collins, D. R., Gaiha, G. D. & Walker, B. D. CD8+ T cells in HIV control, cure and prevention. Nat. Rev. Immunol. 20, 471–482 (2020).
Rosás-Umbert, M. et al. Administration of broadly neutralizing anti-HIV-1 antibodies at ART initiation maintains long-term CD8+ T cell immunity. Nat. Commun. (in the press).
Mendoza, P. et al. Combination therapy with anti-HIV-1 antibodies maintains viral suppression. Nature 561, 479–484 (2018).
Deeks, S. G. et al. Research priorities for an HIV cure: International AIDS Society global scientific strategy 2021. Nat. Med. 27, 2085–2098 (2021).
Estes, J. D. et al. Defining total-body AIDS-virus burden with implications for curative strategies. Nat. Med. 23, 1271–1276 (2017).
Gaebler, C. et al. Prolonged viral suppression with anti-HIV-1 antibody therapy. Nature 606, 368–374 (2022).
Schulz, K. F., Altman, D. G. & Moher, D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials 11, 32 (2010).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
Harris, P. A. et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inform. 95, 103208 (2019).
Baxter, A. E. et al. Single-cell characterization of viral translation-competent reservoirs in HIV-infected individuals. Cell Host Microbe 20, 368–380 (2016).
Grau-Expósito, J. et al. A novel single-cell FISH-flow assay identifies effector memory CD4+ T cells as a major niche for HIV-1 transcription in HIV-infected patients. mBio 8, e00876-17 (2017).
Gaebler, C. et al. Combination of quadruplex qPCR and next-generation sequencing for qualitative and quantitative analysis of the HIV-1 latent reservoir. J. Exp. Med. 216, 2253–2264 (2019).
Parekh, B. S. et al. Performance evaluation of Asante rapid recency assay for HIV diagnosis and detection of recent infection: potential for surveillance and prevention. In: Ninth IAS Conference on HIV Science (2017).
Julg, B. et al. Recommendations for analytical antiretroviral treatment interruptions in HIV research trials—report of a consensus meeting. Lancet HIV 6, e259–e268 (2019).
Besson, G. J. et al. HIV-1 DNA decay dynamics in blood during more than a decade of suppressive antiretroviral therapy. Clin. Infect. Dis. 59, 1312–1321 (2014).
Royston, P. Multiple imputation of missing values: further update of ice, with an emphasis on categorical variables. Stata J. 9, 466–477 (2009).
Rubin D. B. Multiple Imputation for Nonresponse in Surveys (Wiley, 2004).
Austin, P. C., White, I. R., Lee, D. S. & van Buuren, S. Missing data in clinical research: a tutorial on multiple imputation. Can. J. Cardiol. 37, 1322–1331 (2021).
Acknowledgements
We thank all study participants who devoted time to our research as well as every clinical research unit involved in the study: at Aarhus University Hospital—study nurses Yordanos Yehdego, Ane Søndergaard and Ann Bach, physicians Janne T. Martinsen and Nina B. Stærke and lab technician Lene S. Jøhnke; at Copenhagen University Hospital–Amager and Hvidovre—study nurses Dorthe K. Petersen and Louise Krohn-Dehli and lab technician Anna L. Sørensen; at Aalborg University Hospital—study nurses Maria R. Juhl and Kristine T. Pedersen; at Odense University Hospital—study nurses Susan O. Lindvig and Bente Ramskover; at Regional Hospital Herning—study nurses Kirsten Lillevang and Heidi G. Sørensen; at Imperial College Hospital—study nurses Rebecca Hall, Claire Petersen and Shelly Page, physician John Thornhill, lab technician Andrew O Lovell and study coordinator Tom Cole; at King’s College London—study nurses Anele Waters, Rebekah Roberts, Hiromi Uzu and Andrea Berlanga and study coordinator Alice Sharp; and at the Danish Good Clinical Practice Units—monitors Lene Brandsborg, Inge M. Burmeister and Stine K. Hovgaard. We acknowledge Rockefeller University for providing 3BNC117 and Bristol-Myers Squibb Company (Celgene Corporation) for providing the RMD as well as the Labcorp-Monogram Biosciences Clinical Reference Laboratory for performing the phenotypic resistance assays with project management from Y. Lie and C. Kang. Finally, we would like to acknowledge the amazing support and help from the late Amin Alamshah, a kind and brilliant clinical project manager at the Imperial College Center for Translational and Experimental Medicine, who tragically lost his life before the completion of this study. The funders were not involved in the study design/operations, data collection/analysis/interpretation or preparation of the manuscript. This study is funded by the Danish Council for Independent Research (grant numbers: 7016-00022 and 9060-00023B to O.S.S.), the Central Region Denmark Research Fund, The Danish Regions’ Medicine and Treatment Fund, Aarhus University and Next Experimental Therapy Partnership. Research reported in this publication was also supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (award number: UM1AI164565 to R.B.J.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. N.N.K. received a Vanier Award from the Canadian Institutes for Health Research. Z.L.B. received a scholar award from the Michael Smith Foundation for Health Research. Study drugs were donated free of charge by The Rockefeller University (3BNC117) and Celgene (romidepsin) for use in this trial. None of the specific sources of funding had any role in the conceptualization, design, data collection, analysis, decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
O.S.S. developed the trial design. J.D.G., M.T., M.C.N., M.C. and O.S.S. wrote the protocol. J.D.G., T.B., H.N., I.S.J., R.M., L.Ø., V.K., J.F., S.F. and O.S.S. did the clinical visits. J.D.G., M.H.P., M.R.-U., I.-N.L., M.K., M.H.S., R.O., P.W.D., N.N.K., D.C.C., A.R.W., W.D.C.A., S.D.N., M.C.P., J.D.R., C.J.P., J.M.-P., Z.L.B., R.B.J., M.T. and O.S.S. did the laboratory assays and validations. V.R. performed the bioinformatic analysis. J.D.G., M.H.P., M.R.-U. and H.S. did the statistical analysis. J.D.G., P.W.D. and O.S.S. drafted the tables and figures. J.D.G. and O.S.S. drafted the article, which all authors critically revised for important intellectual content. J.D.G. and O.S.S. had full access to all the data in the study, verified the data and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
M.C.N. is listed as an inventor on patents for the antibody 3BNC117. J.D.R. and C.J.P. are employees of Labcorp-Monogram Biosciences. All other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editor: Alison Farrell, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 A comprehensive CONSORT Flow Diagram.
AE, adverse event; Ag, antigen; ART, antiretroviral therapy; COVID-19, coronavirus disease 2019; RMD, romidepsin; SAE, serious AE.
Extended Data Fig. 2
Distribution between self-report time of infection to study enrollment and outcome of the Asanté HIV-1 Rapid Recency Assay (n = 54).
Extended Data Fig. 3 Transcriptionally (mRNA+) and transcriptionally + translationally (mRNA+p24+) active HIV-1-infected cells following ART initiation.
Changes in HIV-1-infected cells during the first 30 days of ART among the four groups shown as median (error bars represents interquartile ranges) number of CD3+CD8- T cells expressing either HIV-1 mRNA (a) or HIV-1 mRNA and Gag p24 protein (b). ART-control n = 4, ART + 3BNC117 n = 5, ART + RMD n = 4, ART + 3BNC117 + RMD n = 5. ART, antiretroviral therapy; RMD, romidepsin.
Extended Data Fig. 4 Impact of 3BNC117 on translationally (p24+) active HIV-1-infected CD4+ T cell subsets.
Data are shown as in Fig. 3b-e, where the ART alone and ART + RMD groups (who only received ART during the first 10 days) are combined into one group and compared to the two 3BNC117-treated groups. Median (error bars represent interquartile ranges) fold change in CD3+CD8- T cell subsets expressing Gag p24 among the combined ART (n = 15) and ART + 3BNC117 (n = 18) groups. The CD3+CD8- T cells subsets are central memory T cells (TCM) (a), naïve T cells (TN) (b), effector memory T cells (TEM) (c), terminally differentiated T cells (TTD) (d), and T follicular helper cells (TFH) (e). P values comparing within group was calculated using paired two-tailed Wilcoxon test. ART, antiretroviral therapy; IQR, interquartile ranges; RMD, romidepsin.
Extended Data Fig. 5 The frequency of HIV-1 antigen-producing cells.
The individual frequency of induced p24+ CD4+ T cells at ART initiation (day 0) and after 365 days of ART (lines at median) (a) and median changes in these cells between day 0 and 365 after ART initiation (b) among individuals in the four groups. P values comparing within group and between groups were calculated using paired two-tailed Wilcoxon test and two-tailed Mann-Whitney test, respectively. Pie charts showing the status of HIV-1 antigen-producing cells after 365 days of ART per group (column and upper row) and categorized according to pre-ART plasma virus sensitivity (middle row; blue shaded area) or resistance (bottom row; red shaded area) to 3BNC117 (c). A compiled group ART + 3BNC117 + /-RMD is shown is the last column. ART-control n = 12, ART + 3BNC117 n = 14, ART + RMD n = 10, ART + 3BNC117 + RMD n = 13. Ag, antigen; ART, antiretroviral therapy; RMD, romidepsin.
Extended Data Fig. 6 Effect of RMD on transcriptionally (mRNA+) and transcriptionally + translationally (mRNA+p24+) active HIV-1-infected cells.
Data are shown as in Fig. 3f, g. Individual and overall median fold change (column) from pre- to post-RMD infusions in groups ART + RMD (n = 8) and ART + 3BNC117 + RMD (n = 10) on CD3+CD8- T cells expressing HIV-1 mRNA (a) or mRNA and Gag p24 (b). P values comparing within group was calculated using paired two-tailed Wilcoxon test. Due to a faulty mRNA probe in the 2nd batch of FISH-flow cytometry analyses, mRNA data was only available for half of the study population. ART, antiretroviral therapy; RMD, romidepsin.
Extended Data Fig. 7 The frequency of defective HIV-1 proviruses.
The frequency of 3’ (a) and 5’ (b) defective HIV-1 proviruses at ART initiation and after 180 and 365 days of ART among individuals in the four groups (lines at median, error bars represent interquartile ranges). P values comparing within group were calculated using paired two-tailed Wilcoxon test. ART only n = 14, ART + 3BNC117 n = 14, ART + RMD n = 10, ART + 3BNC117 + RMD n = 14. ART, antiretroviral therapy; RMD, romidepsin.
Extended Data Fig. 8 CD4+ T cell count and CD4/CD8 ratio during the study.
Tukey plots depicts the CD4+ T cell count (a) and CD4/CD8 ratio (b) in the four groups at baseline (day 0), the interventional period (day 10–30) and during follow-up (day 90–365). Lines indicates median, boxes represent interquartile ranges and whiskers drawn within the 1.5 IQR values. ART only n = 15, ART + 3BNC117 n = 15, ART + RMD n = 13, ART + 3BNC117 + RMD n = 16. ART, antiretroviral therapy; IQR, interquartile range; RMD, romidepsin.
Supplementary information
Supplementary Information
Supplementary Figs. 1–5, Supplementary Tables 1–6, CONSORT checklist and study protocol: eCLEAR-001, version 3.1, 18 September 2018.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gunst, J.D., Pahus, M.H., Rosás-Umbert, M. et al. Early intervention with 3BNC117 and romidepsin at antiretroviral treatment initiation in people with HIV-1: a phase 1b/2a, randomized trial. Nat Med 28, 2424–2435 (2022). https://doi.org/10.1038/s41591-022-02023-7
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41591-022-02023-7
This article is cited by
-
Clinical trials of broadly neutralizing monoclonal antibodies in people living with HIV – a review
AIDS Research and Therapy (2025)
-
Inhibition of ALKBH5 demethylase of m6A pathway potentiates HIV-1 reactivation from latency
Virology Journal (2025)
-
Antibodies and T cells join forces for sustained HIV remission
Nature (2025)
-
PADI4-mediated citrullination of histone H3 stimulates HIV-1 transcription
Nature Communications (2025)
-
Immune-mediated strategies to solving the HIV reservoir problem
Nature Reviews Immunology (2025)