Abstract
Colorectal cancer (CRC) is one of the most prevalent malignancies worldwide, with high postoperative recurrence and metastasis rates posing significant challenges to patient survival. Identifying reliable and accessible prognostic markers is essential for optimizing treatment strategies. This study investigates the prognostic significance of two preoperative hematological indices, the [neutrophils × platelets]/[lymphocytes × hemoglobin] (NP/LHb) ratio and absolute monocyte count (Mono), in predicting overall survival in CRC patients. A retrospective analysis of 566 patients was conducted, with one cohort serving as an external validation set. Receiver operating characteristic curve analysis identified optimal cut-off values for NP/LHb and Mono, and Kaplan-Meier survival analysis revealed that higher levels of both markers were associated with significantly shorter survival. A novel prognostic model, NPM, integrating NP/LHb and Mono, demonstrated superior predictive accuracy compared to either marker alone. The NPM model was further validated through a nomogram, achieving high predictive performance for 1-, 3-, and 5-year survival. These findings highlight the potential of combining inflammatory and nutritional markers for effective risk stratification in CRC patients. The NPM model offers a simple, cost-effective prognostic tool that may facilitate personalized postoperative management, though further prospective validation is warranted.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed malignancy and the second leading cause of cancer-related deaths worldwide1. The incidence of CRC has been rising due to shifts in lifestyle, diet, and environmental factors. Despite advancements in surgical techniques and adjuvant therapies, postoperative recurrence and metastasis remain major challenges, significantly affecting patient survival and quality of life2,3. Identifying reliable prognostic markers that are simple, accessible, and cost-effective is essential for optimizing postoperative management and improving clinical outcomes.
The role of inflammation in cancer progression is well established, with chronic inflammation contributing to tumor proliferation, invasion, and immune evasion4,5. Various inflammation-based prognostic indices, such as the neutrophil-to-lymphocyte ratio (NLR)6, platelet-to-lymphocyte ratio (PLR)7,8, and systemic immune-inflammation index (SII)9, have been reported to correlate with poor survival outcomes in cancer patients. Similarly, nutritional status is a critical determinant of cancer prognosis, influencing immune function, postoperative recovery, and treatment tolerance10. Previous studies have shown that anemia, commonly reflected by low hemoglobin (Hb) levels, is associated with worse survival in CRC patients11,12.
A recently developed inflammatory-nutritional composite index, the NP/LHb ratio (calculated as [neutrophils × platelets] / [lymphocytes × hemoglobin]), has demonstrated predictive potential for CRC development13,14. However, its prognostic utility in CRC patients remains unexplored. Additionally, monocytes play a crucial role in the tumor microenvironment by promoting angiogenesis, immune suppression, and metastasis15,16,17. Given their involvement in CRC progression, the absolute monocyte count (Mono) may serve as an independent prognostic factor.
In this study, we hypothesized that combining NP/LHb and Mono could improve prognostic accuracy for CRC patients. We retrospectively analyzed preoperative NP/LHb and Mono levels in CRC patients and assessed their association with overall survival (OS). Furthermore, we developed a novel prognostic model, NPM, integrating these two markers to enhance risk stratification. This study aims to establish a practical and accessible prognostic tool for CRC patients, providing valuable insights for individualized treatment strategies.
Patients and methods
Study population
This retrospective cohort study included 566 patients diagnosed with primary CRC who underwent radical surgery between January 2016 and December 2017 at two institutions: the Affiliated Cancer Hospital of Xinjiang Medical University (training cohort, n = 435) and the People’s Hospital of Bortala Mongolian Autonomous Prefecture (validation cohort, n = 131). Patients were included if they had histopathologically confirmed primary CRC, underwent curative-intent surgery, were older than 18 years, had available preoperative hematological parameters (measured within one week before surgery), and had complete clinical and follow-up data. Exclusion criteria included the presence of non-primary CRC or other malignancies, unresectable distant metastases, hematological or autoimmune diseases, severe hepatic or renal dysfunction, malnutrition, or prior parenteral nutritional support before surgery. This study was approved by the Ethics Committee of Xinjiang Medical University Cancer Hospital (Approval No. K-2024056) and the Ethics Committee of the People’s Hospital of Bortala Mongolian Autonomous Prefecture (Approval No. LLSH20241221) in accordance with the Declaration of Helsinki, and written informed consent was obtained from all participants or their legal guardians.
Data collection
Clinical and laboratory data were extracted from the electronic medical record systems of both hospitals. The following parameters were recorded: (1) Baseline characteristics: age, sex, height, weight, smoking status, and alcohol consumption. (2) Preoperative hematological parameters: platelet count, lymphocyte count, neutrophil count, monocyte count, hemoglobin level, carcinoembryonic antigen (CEA), and carbohydrate antigen 19 − 9 (CA-199). (3) Pathological features: tumor differentiation, vascular invasion, perineural invasion, and TNM staging. (4) Follow-up data: OS and survival duration (months). The NP/LHb ratio was calculated using the formula NP/LHb = (neutrophil count × platelet count) / (lymphocyte count × hemoglobin level) to evaluate its prognostic significance in CRC patients.
Statistical analysis
All statistical analyses were performed using SPSS v29.0 and R software v4.4.1. Baseline characteristics were expressed as counts (%) for categorical variables and as means ± standard deviation (SD) or medians (interquartile range, IQR) for continuous variables. Group comparisons were conducted using the chi-square test (χ²) or Fisher’s exact test for categorical variables, the independent t-test or analysis of variance (ANOVA) for normally distributed continuous variables, and the Wilcoxon rank-sum test for non-normally distributed variables. Receiver operating characteristic (ROC) curve analysis was performed to determine the optimal cut-off values for NP/LHb and Mono, with the area under the curve (AUC) used to assess their predictive accuracy. Kaplan-Meier survival curves were constructed, and differences were compared using the log-rank test, while restricted cubic spline (RCS) plots were used to evaluate the nonlinear relationship between NP/LHb, Mono, and mortality risk. A novel prognostic model (NPM) was developed by integrating NP/LHb and Mono, with scoring criteria as follows: NPM = 0 (NP/LHb < 5.667 and Mono < 0.505), NPM = 1 (either NP/LHb ≥ 5.667 or Mono ≥ 0.505), and NPM = 2 (both NP/LHb ≥ 5.667 and Mono ≥ 0.505). Multivariate Cox proportional hazards regression analysis was conducted to evaluate independent prognostic factors. A nomogram was constructed incorporating NP/LHb, Mono, NPM, and N stage, with predictive performance assessed using ROC curves (1-, 3-, and 5-year AUC values), calibration curves, and decision curve analysis (DCA). External validation was performed using the validation cohort, and statistical significance was set at p < 0.05.
Results
Clinicopathological characteristics of the study cohort
This study included 566 CRC patients who underwent radical resection, with 435 patients in the training cohort and 131 patients in the validation cohort. Among them, 59.0% were male, with a median age of 62 years. TNM staging distribution was as follows: 18.9% in stage I, 45.6% in stage II, 33.9% in stage III, and 1.6% in stage IV. The majority of tumors were moderately differentiated (83.0%), while 15.2% were poorly differentiated and 1.8% were well-differentiated. Perineural invasion and vascular tumor emboli were observed in 14.0% and 19.3% of patients, respectively. Elevated CEA and CA-199 levels were found in 37.1% and 10.1% of patients, respectively. No significant differences were observed in baseline characteristics between the training and validation cohorts (Table 1).
Association between NP/LHb and mono with clinicopathological features
In the training cohort, high NP/LHb levels were significantly associated with older age (p = 0.0132), T stage (p < 0.001), BMI (p = 0.021), N stage (p = 0.043), TNM stage (p = 0.002), CEA (p = 0.004), and CA-199 (p = 0.004). Similarly, high Mono levels were significantly associated with age (p < 0.001), T stage (p = 0.010), and tumor stage (p = 0.001). However, no statistically significant associations were found between NP/LHb or Mono and histological grade, perineural invasion, vascular invasion, smoking status, or alcohol consumption (Table 2).
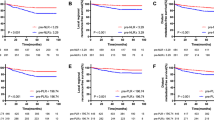
Determination of optimal Cut-off values for NP/LHb and mono
ROC curve analysis identified 5.667 as the optimal cut-off value for NP/LHb (AUC = 0.760) and 0.505 for Mono (AUC = 0.663), both demonstrating predictive capability for CRC prognosis (Fig. 1A). RCS analysis revealed a progressive increase in mortality risk with rising NP/LHb and Mono levels, confirming their continuous impact on survival outcomes (Fig. 1B, C).
Prognostic significance of NP/LHb and Mono in CRC patients. (A) ROC curve analysis for NP/LHb and Mono, demonstrating their prognostic accuracy. (B, C) RCS plots illustrating the nonlinear relationship between NP/LHb, Mono, and OS risk. (D, E) Kaplan-Meier survival curves showing significantly worse OS in patients with high NP/LHb and high Mono levels (p < 0.001 for both). (F, G) Stratified survival analysis further confirming that elevated NP/LHb and Mono are independently associated with increased mortality risk in CRC patients.
Impact of NP/LHb and mono on OS
Kaplan-Meier survival analysis demonstrated that patients with high NP/LHb or high Mono levels had significantly shorter OS compared to those with low NP/LHb or low Mono levels (p < 0.001, log-rank test) (Fig. 1D, E). In subgroup analysis, high NP/LHb and high Mono remained independently associated with increased mortality risk (Fig. 1F, G).
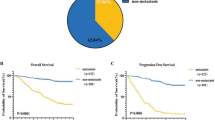
Development and prognostic value of the NPM model
To enhance predictive accuracy, we developed the NPM model, integrating NP/LHb and Mono, as shown in Table 3. Based on their cut-off values, patients were categorized as follows: NPM = 0 (low NP/LHb and low Mono), NPM = 1 (either NP/LHb or Mono high), and NPM = 2 (both NP/LHb and Mono high). The NPM model demonstrated superior prognostic performance compared to individual markers, achieving an AUC of 0.810, significantly higher than NP/LHb (0.760) or Mono (0.663) alone (Fig. 2A). Kaplan-Meier survival analysis confirmed that patients with NPM = 2 had significantly worse OS compared to those with NPM ≤ 1 (p < 0.001) (Fig. 2B, C). Multivariate Cox regression analysis further validated that higher NPM scores were independently associated with increased mortality risk, with HR = 5.09 (95% CI: 2.64–9.80, p < 0.001) for NPM = 1 and HR = 10.82 (95% CI: 5.26–22.25, p < 0.001) for NPM = 2, compared to NPM = 0 (Table 4).
Development and validation of the NPM prognostic model. (A) ROC curve demonstrating the predictive performance of the NPM model compared to NP/LHb and Mono alone. The NPM model achieves the highest AUC, indicating superior prognostic accuracy. (B, C) Kaplan-Meier survival curves stratified by NPM score, showing significantly poorer OS in patients with higher NPM values (p < 0.001). (D) Stratified survival analysis indicating that high NPM scores correlate with increased mortality risk in CRC patients.
Nomogram construction and validation
To facilitate clinical application, we constructed a nomogram model incorporating NP/LHb, Mono, NPM, and N stage to predict 1-, 3-, and 5-year survival probabilities (Fig. 3A). The nomogram exhibited high predictive accuracy, with AUC values of 0.856, 0.842, and 0.837 for 1-, 3-, and 5-year OS, respectively, in the training cohort (Fig. 3B) and 0.783, 0.730, and 0.799 in the validation cohort (Fig. 3C). Calibration curves demonstrated excellent agreement between predicted and observed survival probabilities (Fig. 3D). DCA further confirmed the clinical utility of the nomogram, showing superior net benefit in risk stratification compared to conventional models (Fig. 4A–F).
Nomogram for predicting OS in CRC patients. (A) A prognostic nomogram incorporating NP/LHb, Mono, NPM score, and N stage to predict 1-, 3-, and 5-year survival probabilities. (B, C) ROC curves for the training and validation cohorts, demonstrating high AUC values for 1-, 3-, and 5-year survival predictions, confirming the model’s predictive accuracy. (D) Calibration curves comparing predicted and observed survival probabilities, indicating excellent agreement between model predictions and actual survival outcomes.
DCA for clinical utility assessment of the nomogram model. (A–C) DCA curves for 1-, 3-, and 5-year survival in the training cohort, demonstrating the net clinical benefit of the nomogram in guiding risk stratification. (D–F) DCA curves for the validation cohort, confirming the nomogram’s robust predictive performance and potential clinical applicability for CRC prognosis.
External validation of the NPM model
To assess the generalizability of the NPM model, external validation was performed using the independent validation cohort (n = 131). The NPM model maintained robust predictive performance, with AUC values of 0.783, 0.730, and 0.799 for 1-, 3-, and 5-year OS, respectively. Kaplan-Meier analysis in the validation cohort further confirmed that patients with NPM = 2 had significantly shorter OS compared to those with NPM ≤ 1 (p < 0.001). The DCA in the validation cohort also demonstrated strong clinical applicability, supporting the potential integration of NPM into routine CRC prognostic assessment.
Discussion
CRC remains a significant global health burden, with high postoperative recurrence and metastasis rates leading to poor long-term survival1,18. Identifying reliable, accessible, and cost-effective prognostic markers is essential for improving individualized patient management. In this study, we demonstrated that both the NP/LHb index and Mono are independently associated with OS in CRC patients. Furthermore, we developed a novel prognostic model, NPM, integrating these two markers, which significantly outperformed NP/LHb or Mono alone in predicting patient survival. The NPM model, validated in an independent cohort, represents a promising, readily available prognostic tool for CRC risk stratification.
The inflammatory response plays a crucial role in tumor development, progression, and immune evasion19. Several hematological indices, including NLR, PLR, and SII, have been widely recognized as prognostic biomarkers in various malignancies20,21,22,23. Our study extends this evidence by evaluating NP/LHb, a composite inflammatory-nutritional index, which combines neutrophils, platelets, lymphocytes, and hemoglobin. This index reflects both systemic inflammation and nutritional status, which are integral components of cancer progression. We found that high NP/LHb was significantly associated with worse OS, reinforcing its prognostic value in CRC. Similarly, monocytes are key players in the tumor microenvironment, contributing to angiogenesis, immunosuppression, and metastasis15. Elevated Mono levels have been linked to worse survival outcomes in multiple cancers17,24,25,26. Our findings support this notion, as high preoperative Mono levels were independently associated with poor prognosis in CRC patients. The strong predictive value of Mono highlights its potential as a simple and effective prognostic biomarker.
While individual biomarkers provide valuable prognostic insights, combining multiple markers often enhances predictive accuracy27,28. Our study demonstrates that integrating NP/LHb and Mono into the NPM model significantly improved survival prediction, achieving an AUC of 0.810, which was notably higher than NP/LHb (0.760) or Mono (0.663) alone. The Kaplan-Meier survival analysis further confirmed that patients with NPM = 2 had significantly shorter OS compared to those with NPM ≤ 1 (p < 0.001). Moreover, Cox proportional hazards regression analysis validated that higher NPM scores were independently associated with increased mortality risk, reinforcing the robustness of this prognostic model. To facilitate clinical translation, we developed a nomogram incorporating NP/LHb, Mono, NPM, and N stage. The high AUC values for 1-, 3-, and 5-year OS in both the training and validation cohorts (0.856, 0.842, 0.837 and 0.783, 0.730, 0.799, respectively) confirmed the strong predictive performance of the nomogram. Furthermore, calibration curves demonstrated excellent agreement between predicted and observed survival probabilities, while decision curve analysis (DCA) indicated substantial net clinical benefit, suggesting that the NPM model may be a valuable tool for guiding postoperative management in CRC patients.
Numerous prognostic models for CRC have been proposed, incorporating hematological markers, tumor staging, and molecular signatures. However, many of these models require expensive molecular testing or complex computational analysis, limiting their applicability in routine clinical settings29,30,31,32. In contrast, our NPM model is based on readily available preoperative blood parameters, making it highly accessible and cost-effective. The ease of use and superior predictive performance of the NPM model provide a compelling rationale for its potential integration into clinical practice.
The findings of this study have several clinical implications. First, preoperative assessment of NP/LHb and Mono could enable better risk stratification of CRC patients, allowing for more tailored treatment strategies. High-risk patients may benefit from closer postoperative surveillance and more aggressive adjuvant therapy, while low-risk patients may be spared from overtreatment. Second, the nomogram provides an individualized survival probability estimate, which could assist in shared decision-making between clinicians and patients.
Despite the strengths of our study, several limitations should be acknowledged. First, this was a retrospective study conducted at two institutions, and although external validation was performed, further large-scale, multicenter prospective studies are needed to confirm the generalizability of our findings. Second, potential confounding factors, such as patient comorbidities and treatment regimens, were not fully accounted for, which may influence survival outcomes. Third, while our study focused on preoperative blood-based biomarkers, integrating molecular and genetic markers may further enhance prognostic precision. Future research should explore the potential synergistic value of NPM with tumor genomic profiling to refine CRC prognostication.
Conclusion
Our findings confirm that both the NP/LHb index and Mono independently predict CRC prognosis. By integrating these two markers, the NPM model enhances survival prediction accuracy beyond individual markers, providing a robust and clinically accessible prognostic tool. The nomogram incorporating NPM provides a practical, cost-effective tool for CRC risk stratification, with strong predictive accuracy and potential clinical utility. Prospective validation and further refinement of the model, potentially incorporating molecular markers, will be essential to optimize CRC prognostication and guide personalized treatment strategies.
Data availability
All data generated or analysed during this study are included in this published article.
References
Siegel, R. L., Kratzer, T. B., Giaquinto, A. N., Sung, H. & Jemal, A. Cancer statistics, 2025. CA Cancer J. Clin. 75, 10–45. https://doi.org/10.3322/caac.21871 (2025).
Han, L. et al. Nomogram of conditional survival probability of long-term survival for metastatic colorectal cancer: A Real-World data retrospective cohort study from SEER database. Int. J. Surg. 92, 106013. https://doi.org/10.1016/j.ijsu.2021.106013 (2021).
Shapaer, T. et al. Elevated BEAN1 expression correlates with poor prognosis, immune evasion, and chemotherapy resistance in rectal adenocarcinoma. Discov Oncol. 15, 446. https://doi.org/10.1007/s12672-024-01321-5 (2024).
He, W. et al. Do inflammatory markers predict prognosis in patients with synchronous colorectal cancer? Medicine 96, e6607. https://doi.org/10.1097/MD.0000000000006607 (2017).
Wan, R. et al. Decoding gastric cancer: machine learning insights into the significance of COMMDs family in immunotherapy and diagnosis. J. Cancer. 15, 3580–3595. https://doi.org/10.7150/jca.94360 (2024).
Pine, J. K. et al. Systemic neutrophil-to-lymphocyte ratio in colorectal cancer: the relationship to patient survival, tumour biology and local lymphocytic response to tumour. Br. J. Cancer. 113, 204–211. https://doi.org/10.1038/bjc.2015.87 (2015).
Xu, N. et al. The prognostic value of the neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) in colorectal cancer and colorectal anastomotic leakage patients: a retrospective study. BMC Surg. 25, 57. https://doi.org/10.1186/s12893-024-02708-5 (2025).
Shayimu, P. et al. Serum nutritional predictive biomarkers and risk assessment for anastomotic leakage after laparoscopic surgery in rectal cancer patients. World J. Gastrointest. Surg. 16, 3142–3154. https://doi.org/10.4240/wjgs.v16.i10.3142 (2024).
Zhao, W. et al. Nutritional and inflammatory status dynamics reflect preoperative treatment response and predict prognosis in locally advanced rectal cancer: A retrospective multi-institutional analysis. Surgery 178, 108965. https://doi.org/10.1016/j.surg.2024.108965 (2025).
Wang, Q. et al. IL1RN and PRRX1 as a prognostic biomarker correlated with immune infiltrates in colorectal cancer: evidence from bioinformatic analysis. Int. J. Genomics. 2723264. https://doi.org/10.1155/2022/2723264 (2022).
Zeng, X. et al. Effects of micronutrients and macronutrients on risk of allergic disease in the European population: a Mendelian randomization study. Food Agricultural Immunol. 35. https://doi.org/10.1080/09540105.2024.2442369 (2024).
Liu, C. A. et al. Muscle distribution in relation to all-cause and cause-specific mortality in young and middle-aged adults. J. Transl Med. 21, 154. https://doi.org/10.1186/s12967-023-04008-7 (2023).
Hernandez-Ainsa, M., Velamazan, R., Lanas, A., Carrera-Lasfuentes, P. & Piazuelo, E. Blood-Cell-Based inflammatory markers as a useful tool for early diagnosis in colorectal cancer. Front. Med. (Lausanne). 9, 843074. https://doi.org/10.3389/fmed.2022.843074 (2022).
Lanas, A., García-Rayado, G. & Editorial Insights in gastroenterology: 2021. Front. Med. (Lausanne). 9, 1008157. https://doi.org/10.3389/fmed.2022.1008157 (2022).
Jakubowska, K., Koda, M., Grudzińska, M., Kańczuga-Koda, L. & Famulski, W. Monocyte-to-lymphocyte ratio as a prognostic factor in peripheral whole blood samples of colorectal cancer patients. World J. Gastroenterol. 26, 4639–4655. https://doi.org/10.3748/wjg.v26.i31.4639 (2020).
Montalbán-Hernández, K. et al. Colorectal cancer stem cells fuse with monocytes to form tumour hybrid cells with the ability to migrate and evade the immune system. Cancers (Basel). 14, 3445. https://doi.org/10.3390/cancers14143445 (2022).
Larionova, I. et al. PFKFB3 overexpression in monocytes of patients with colon but not rectal cancer programs pro-tumor macrophages and is indicative for higher risk of tumor relapse. Front. Immunol. 13, 1080501. https://doi.org/10.3389/fimmu.2022.1080501 (2023).
Wu, Z., Chen, Y., Yu, G. & Ma, Y. Research trends and hotspots in surgical treatment of recurrent nasopharyngeal carcinoma: A bibliometric analysis from 2000 to 2023. Asian J. Surg. 47, 2939–2941. https://doi.org/10.1016/j.asjsur.2024.02.106 (2024).
Liu, C. et al. Temporal relationship between inflammation and metabolic disorders and their impact on cancer risk. J. Glob Health. 14, 04041. https://doi.org/10.7189/jogh.14.04041 (2024).
Bartlett, E. K. et al. High neutrophil-to-lymphocyte ratio (NLR) is associated with treatment failure and death in patients who have melanoma treated with PD-1 inhibitor monotherapy. Cancer 126, 76–85. https://doi.org/10.1002/cncr.32506 (2020).
Qi, X. et al. Prognostic significance of platelet-to-lymphocyte ratio (PLR) in patients with breast cancer treated with neoadjuvant chemotherapy: a meta-analysis. BMJ Open. 13, e074874. https://doi.org/10.1136/bmjopen-2023-074874 (2023).
Zhu, Y. et al. Using machine learning to identify patients at high risk of developing low bone density or osteoporosis after gastrectomy: a 10-year multicenter retrospective analysis. J. Cancer Res. Clin. Oncol. 149, 17479–17493. https://doi.org/10.1007/s00432-023-05472-w (2023).
Fest, J. et al. The systemic immune-inflammation index is associated with an increased risk of incident cancer-A population-based cohort study. Int. J. Cancer. 146, 692–698. https://doi.org/10.1002/ijc.32303 (2020).
Chen, X., Li, Y., Xia, H. & Chen, Y. H. Monocytes in tumorigenesis and tumor immunotherapy. Cells 12, 1673. https://doi.org/10.3390/cells12131673 (2023).
Zhang, H. et al. KIF18A inactivates hepatic stellate cells and alleviates liver fibrosis through the TTC3/Akt/mTOR pathway. Cell. Mol. Life Sci. 81, 96. https://doi.org/10.1007/s00018-024-05114-5 (2024).
Sajadieh, A. et al. Monocyte number associated with incident cancer and mortality in middle-aged and elderly community-dwelling Danes. Eur. J. Cancer. 47, 2015–2022. https://doi.org/10.1016/j.ejca.2011.02.015 (2011).
Gould, L. E. et al. A systematic review of the pathological determinants of outcome following resection by pelvic exenteration of locally advanced and locally recurrent rectal cancer. Int. J. Surg. 104, 106738. https://doi.org/10.1016/j.ijsu.2022.106738 (2022).
Wang, Q. et al. Establishment of a novel lysosomal signature for the diagnosis of gastric cancer with in-vitro and in-situ validation. Front. Immunol. 14, 1182277. https://doi.org/10.3389/fimmu.2023.1182277 (2023).
Qin, M. et al. Tumor-infiltrating lymphocyte: features and prognosis of lymphocytes infiltration on colorectal cancer. Bioengineered 13, 14872–14888. https://doi.org/10.1080/21655979.2022.2162660 (2022).
He, X. et al. Prognostic role of Lymphocyte-C-Reactive protein ratio in colorectal cancer: A systematic review and meta analysis. Front. Oncol. 12, 905144. https://doi.org/10.3389/fonc.2022.905144 (2022).
Wu, Z. et al. Mitochondrial-related drug resistance LncRNAs as prognostic biomarkers in laryngeal squamous cell carcinoma. Discov Oncol. 15, 785. https://doi.org/10.1007/s12672-024-01690-x (2024).
Lawler, T., Parlato, L. & Warren Andersen, S. Racial disparities in colorectal cancer clinicopathological and molecular tumor characteristics: a systematic review. Cancer Causes Control. 35, 223–239. https://doi.org/10.1007/s10552-023-01783-y (2024).
Funding
This study was financially supported by the Natural Science Foundation of Xinjiang Uygur Autonomous Region (Project No. 2022D01C297).
Author information
Authors and Affiliations
Contributions
Zeliang Zhao, Yi Chen and Junmin Guan contributed to study concept and design. Kuan Wang and Kejin Li collected clinical data. Ziyi Zhang, Xiangyue Zeng, Subinur Sulayman and Saibihutula Ababaike contributed to analyze the data. Junfeng Chu, Zhimin Wu and Yipeng Pan contributed to prepare the manuscript. Kuan Wang provided critical feedback on methods, supervised the study. All authors approved the final version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was approved by the Ethics Committee of Xinjiang Medical University Cancer Hospital (Approval No. K-2024056) and the Ethics Committee of the People’s Hospital of Bortala Mongolian Autonomous Prefecture (Approval No. LLSH20241221) in accordance with the Declaration of Helsinki, and written informed consent was obtained from all participants or their legal guardians.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, K., Li, K., Zhang, Z. et al. Prognostic value of combined NP and LHb index with absolute monocyte count in colorectal cancer patients. Sci Rep 15, 8902 (2025). https://doi.org/10.1038/s41598-025-94126-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-94126-7
Keywords
This article is cited by
-
G-CSF promotes H3K27ac-modified KLF5 to activate CXCR4 expression and drive colon cancer growth and metastasis
European Journal of Medical Research (2026)
-
Risk factors and predictive model of lymph node metastasis in clinical stage IA peripheral non-small cell lung cancer: a retrospective study
BMC Cancer (2025)
-
Identifying risk factors and evaluating therapeutic interventions for anastomotic recurrence in postoperative esophageal squamous cell carcinoma
BMC Cancer (2025)
-
Trends in pancreatic cancer mortality among US adults, 1999–2023
BMC Gastroenterology (2025)
-
Erythrocyte lifespan for predicting moderate and severe anemia in advanced gastric cancer patients post-anti-tumor therapeutics: a prospective study
BMC Cancer (2025)