Abstract
Congenital factor (F) VII deficiency is caused by mutations in the F7 gene. The p.Q160R variant manifests with bleeding episodes due to reduced FVII activity and antigen in patient plasma, most likely caused by protein misfolding and intracellular retention. As current replacement therapy is expensive and requires frequent intravenous injections, there is an unmet need for new and less invasive therapeutic strategies. Drug repurposing allows for rapid, more cost-effective discovery and implementation of new treatments, and identification of pharmacological enhancers of FVII variant activity would be of clinical importance. High-throughput screening of > 1800 FDA-approved drugs identified the orally available histone deacetylase inhibitor abexinostat and the inhaled surfactant tyloxapol as enhancers of FVII p.Q160R variant activity. The positive hits were verified in an in vitro cell model transiently expressing wild type or variant FVII and ex vivo in patients’ plasma. Both drugs showed a dose-response effect on FVII antigen and activity levels in conditioned cell medium and on FVII activity in patients’ plasma. In conclusion, the efficacy of the FDA-approved drugs abexinostat and tyloxapol in enhancing FVII variant activity constitute a proof of principle for high-throughput identification of drugs that may be feasible for novel treatment of FVII deficiency.
Similar content being viewed by others
Introduction
Coagulation factor (F) VII is a vitamin K-dependent plasma glycoprotein synthesized by the liver that circulates as a single-chain zymogen at a low concentration1. Upon vascular damage, it is activated by binding to tissue factor (TF) and the resulting TF/FVII(a) catalytic complex activates downstream clotting factors, thereby leading to initiation of blood coagulation2. Impaired FVII(a) activity reduces the clotting ability and causes bleeding.
Congenital FVII deficiency is a rare bleeding disorder that follows an autosomal recessive pattern of inheritance, and the disease is characterized by mutations in the F7 gene and concomitant reduced levels of both FVII antigen (FVII: Ag) and activity (FVII:C) (type I deficiency) or only FVII activity (type II deficiency)3. With a prevalence of symptomatic individuals of around 1:300.000-500.000, it is the most common of the rare congenital bleeding disorders, although in Norway and some other countries higher prevalences have been reported4,5,6,7. The clinical phenotypes are highly heterogenous and vary from mild to severe bleeding8.
Most of the F7 gene variants are missense mutations that generate amino acid substitutions in the protein sequence. The FVII protein consists of an amino-terminal γ-carboxy-glutamatic acid domain followed by two epidermal growth (EGF) domains and a carboxyl (C)-terminal protease domain9, and genetic variants affecting all protein domains have been found. In Norway, the most prevalent variant in FVII deficient patients is the missense mutation p.Q160R (legacy name Q100R). This mutation is in the second EGF domain of F7 (NM_000131.4) and have an A to G transition at position 479 (c.479A > G) that alters a glutamine to an arginine at codon 16010. The p.Q160R (160R) variant is associated with severe to moderate type I deficiency and manifest with bleeding episodes due to reduced FVII antigen and activity levels in plasma. Overexpression studies with recombinant (r) FVII-160R have shown that the amino acid substitution causes misfolding of the protein and reduced secretion due to retention in the endoplasmatic reticulum11,12 and impaired binding to TF13 in vitro.
So far, the only available treatment for congenital FVII deficiency is replacement therapy with factor concentrates, using either rFVIIa or plasma derived FVII14. This treatment requires frequent intravenous injections, needs careful monitoring, and is very expensive and is therefore a significant burden both to the quality of life for the patients and economically to the society. Thus, there is a need for new therapeutic strategies for FVII deficient patients that are less invasive, easier to deliver and more cost efficient. Drug repurposing is one strategy that allows for discovery and implementation of new treatments of already approved drugs in a shorter time frame15,16.
In the present study, we aimed to investigate whether it was possible to identify and verify drugs approved for other indications that could increase FVII variant activity. We screened nearly 1900 US Food and Drugs Administration (FDA)-approved drugs and identified the orally available histone deacetylase inhibitor abexinostat and the inhaled surfactant tyloxapol as enhancers of FVII-160R variant activity both in vitro and ex vivo. We further evaluated the dose-response and cellular effect of the two drugs using an in vitro cell culture model. Identification of pharmacological enhancers of FVII activity would be of clinical importance since a modest increase of FVII activity can ameliorate the bleeding phenotype in patients.
Results
High-throughput screening of drug libraries
To identify drugs that could enhance FVII-p.Q160R variant activity, conditioned medium from CHO-K1 cells transiently expressing either rFVII-wild type (wt) or rFVII-160R mutant was treated with 1875 different drugs in the high-throughput screening (HTS) of two different libraries. Prior to the HTS, the FVII activity assay was tested on the HTS platform using untreated conditioned cell medium. The activity in the conditioned medium from CHO-K1 cells overexpressing the rFVII-160R variant was significantly lower than that of the rFVII-wt overexpressing cells, and just slightly above the negative control medium (Fig. 1).
The activity of rFVII-160R in conditioned medium was severely reduced compared to rFVII-wt. Equal amounts of FVII-wt antigen from transiently transfected CHO-K1 cells expressing rFVII-wt (blue curve) or rFVII-160R (red curve) were analyzed. Empty vector (pcDNA3, grey curve) was used as negative control.
For the HTS, the cell culture medium was incubated with the different library drugs before FVII activity was measured. The initial screen resulted in 13 hits for drugs that induced the FVII activity and 168 hits that inhibited the FVII activity. The five most potent inducers and inhibitors are summarized in table S1. The orally available histone deacetylase inhibitor abexinostat and the inhaled surfactant tyloxapol were identified as the most potent inducers of rFVII-160R mutant activity based on the absorbance after two hours (A405) (table S1, Fig. 2A, B).
High-throughput screening (HTS) of drug libraries identified abexinostat (A) and tyloxapol (B) as enhancers of rFVII-160R activity. FVII activity was measured in conditioned medium from CHO-K1 cells transiently expressing wild type protein (rFVII-wt, green lines), mutant FVII protein (rFVII-160R, red lines) or mutant protein (rFVII-160R) + abexinostat (A) or tyloxapol (B) (blue line).
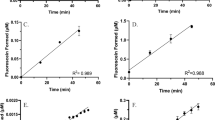
Abexinostat and tyloxapol were then further tested in a dose-response experiment. We incubated cell culture medium containing rFVII-160R with increasing doses of the drugs, ranging from 0.1 to 100 µM. Both abexinostat and tyloxapol showed a dose-response effect on FVII activity (Fig. 3A, B), and the EC50 values were calculated to be 0.98 µM and 3.4 µM, respectively.
Dose-response analysis of abexinostat and tyloxapol on FVII activity in cell culture medium from CHO-K1 cells transiently expressing rFVII-160R. The cells were treated with indicated concentrations of abexinostat (A) or tyloxapol (B) for 1.5 h before FVII activity was measured. EC50 value is indicated (dotted line).
Effect of abexinostat and tyloxapol on FVII activity in patient plasma
Next, we wanted to see if we could validate the findings in clinical samples. Plasma samples from seven patients with the FVII-p.Q160R mutation were collected and analysis of the FVII antigen (FVII:Ag) showed an average level of 194 mIU/mL (range 108–351 mIU/mL) in the samples. In comparison, normal pooled plasma measured 1076 mIU/mL. We then incubated the samples with different doses of abexinostat or tyloxapol. The initial velocity (V0) and absorbance (A405) at two hours for each patient sample were calculated and both treatments showed a dose-response effect on FVII activity in the patients’ plasmas (Fig. 4A, B). Abexinostat showed an average EC50 value of 2.8 µM (range 1.9–4.6) and tyloxapol demonstrated an average EC50 of 2.4 µM (range 1.9–4.3) (Fig. 4C). The change of magnitude in FVII activity was approximately 19% for abexinostat whereas the change of magnitude in FVII activity for tyloxapol was 21% (Fig. 4D).
Dose-response effect of abexinostat and tyloxapol on FVII-p.Q160R activity in plasma from FVII deficient patients. Citrated plasma was collected from 7 different FVII deficient patients harboring the p.Q160R variant. Dose-response analysis (range 0.1–10 µM) of abexinostat (A) and tyloxapol (B) on FVII activity was performed. Pooled normal plasma was used as a positive control. One representative patient is shown. EC50 (C) and Change of magnitude (D) of FVII activity in plasma samples from patients carrying the FVII-p.Q160R mutation stimulated with 10 µM abexinostat (n = 6) or tyloxapol (n = 7). Mean levels (+ SEM) are shown.
Treatment of overexpressing CHO-K1 cells with abexinostat or tyloxapol
As the p.Q160R mutation leads to reduction in both antigen and activity levels, we investigated whether abexinostat and tyloxapol could also affect expression and secretion of the FVII-160R mutant, using a cell model without endogenous FVII expression.
To assess whether the drugs could affect the expression of FVII, the overexpressing cells were stimulated with increasing concentrations (10–100 µM) of either abexinostat or tyloxapol for 24 h. A significant 50–80% increase in F7 mRNA levels was observed for all concentrations of abexinostat (Fig. 5A).
Effect of abexinostat on expression, secretion, and activity on mutant rFVII. CHO-K1 cells were transiently transfected with pcDNA3-FVII p.Q160R. 24 h post transfection the cells were stimulated with indicated levels of abexinostat for 24 h before harvest. F7 mRNA levels were measured with qRT-PCR using 18 S as the endogenous control gene (A). FVII:Ag levels were measured with ELISA in conditioned medium (B) and cell lysates (C). FVII activity was measured in conditioned medium (D). All values were normalized against the corresponding total protein or 18 S content in the respective samples. The bars represent mean + SD from at least three independent experiments performed in duplicate or triplicate (n ≥ 6).
There was a significant increase in the rFVII-160R antigen levels after abexinostat treatment of about 1.5-fold in the conditioned medium (Fig. 5B) and around 2-fold in the cell lysates (Fig. 5C), for all the concentrations, compared to untreated cells. Furthermore, FVII activity in the conditioned medium from cells expressing rFVII-160R was significantly increased 1.5- to 2-fold after stimulation with different concentrations of abexinostat (Fig. 5D).
In cells treated with tyloxapol, no difference in F7 mRNA expression was observed (Fig. 6A). However, both FVII antigen in the conditioned medium and cell lysates (Fig. 6B, C) and FVII activity levels (Fig. 6D) were significantly increased up to 50% and 25%, respectively, from cells expressing rFVII-160R after stimulation with 50 µM of tyloxapol. Stimulation with higher doses than 50 µM abolished FVII activity (Fig. 6D).
Effect of tyloxapol on expression, secretion, and activity on mutant rFVII. CHO-K1 cells were transiently transfected pcDNA3-p.Q160R. 24 h post transfection the cells were stimulated with increasing levels of tyloxapol for 24 h. F7 mRNA levels were measured with qRT-PCR using 18 S as the endogenous control gene (A). FVII:Ag were measured in conditioned medium (B) and cell lysates (C) by ELISA and FVII activity was measured in conditioned medium (D). Data were normalized against the corresponding total protein content in the respective samples. Bars represent mean + SD from at least three independent experiments performed in duplicate (n ≥ 6).
We then tested whether abexinostat and tyloxapol could have a cytotoxic effect on the cells. Treatment with abexinostat for 24 h significantly reduced cell viability by 60% at all three doses (Fig. 7A). Tyloxapol treatment, however, had no effect on cell viability at either dose (Fig. 7B).
Effect of abexinostat or tyloxapol on cell viability. CHO-K1 cells were treated with different doses of abexinostat (A) or tyloxapol (B) for 24 h before cell viability was assessed using Cell Counting Kit – 8. Absorbance was measured at 450 nm. The bars represent the mean +- SD from three independent experiments with 4 biological parallels (n = 12).
Treatment with tyloxapol affects intracellular trafficking of FVII
Since treatment with tyloxapol increased the secretion of rFVII-160R without affecting F7 mRNA levels or cell viability, we assessed whether tyloxapol could aid in restoring the intracellular trafficking of this FVII mutant. Therefore, we investigated the intracellular localization of rFVII-wt and rFVII-160R in cells treated with 10 µM and 50 µM tyloxapol by confocal microscopy using double staining for FVII and different organelle structures. In control cells and cells treated with tyloxapol, both rFVII-wt and rFVII-160R co-localized with the ER marker PDI (Fig. 8A). We then investigated the possible pathways that might be involved in the secretion of FVII using double staining of FVII with different ER and Golgi markers (Fig. 8A, B). In cells treated with either 10 µM or 50 µM tyloxapol, a significant increase in co-localization between rFVII-160R and the Golgi marker GRASP65 was observed (Fig. 8C) while no difference was seen in cells expressing rFVII-wt.
Intracellular localization of rFVII-160R after treatment with tyloxapol. Cells transiently transfected with rFVII-wt or rFVII-160R were treated with tyloxapol for 24 h. (A) Confocal images of cells treated with 0 µM, 10 µM or 50 µM tyloxapol and stained with FVII (green a, d, g, j, m, p) and PDI (red b, e, h, k, n, q)-stained. Co-localized green and red pixels are shown in yellow color (c, f, i, l, o, r). (B) Confocal images of cells treated with 0 µM, 10 µM or 50 µM tyloxapol and stained with FVII (green a, d, g, j, m, p) and GRASP65 (red b, e, h, k, n, q)-stained. Co-localized green and red pixels appear as yellow (c, f, i, l, o, r). (C) The co-localization of FVII with GRASP65 was calculated by the Pearson’s correlation coefficient. The bars represent mean + SD of 5 randomly selected image areas from at least three independent experiments (n ≥ 15).
Discussion
In the present study, we have examined drug repurposing as a method for identifying medications that may be used as an alternative treatment for FVII deficiency. Drug repurposing is a development process for identifying new uses for approved drugs that are outside the scope of the original medical identification17. To test drugs that could enhance FVII p.Q160R variant activity in vitro in conditioned cell medium we used high throughput screening (HTS) of commercially available drug libraries designed especially to include small molecule drugs with high chemical and pharmacological diversity and safety in humans. The advantage of using this strategy is that a repurposed drug has already been considered sufficiently safe in preclinical testing. For the drug screening and the in vitro cell model, we used CHO-K1 cells for mammalian overexpression of rFVII since these cells are known to produce biologically active FVII with similar post-translational modifications as in human plasma18,19,20 and have no interfering endogenous expression of FVII. The HTS identified several hits that affected FVII mutant activity in the conditioned medium. Interestingly, some of the hits were strong inhibitors of rFVII activity in general. For the drugs that enhanced rFVII activity, the two most potent, abexinostat and tyloxapol, were chosen for further testing both in conditioned cell media and in patients’ plasma ex vivo.
We have previously shown that protein misfolding causes impaired secretion of the p.Q160R variant in vitro12 and Kemball-Cook et al.13 have shown that impaired binding of the variant to TF and subsequent reduced ability to activate FX causes reduced activity of the p.Q160R variant in vitro. The low FVII activity observed in the conditioned medium from cells expressing the mutant FVII molecule is therefore most likely a result of both less FVII being secreted and of reduced biological activity of the secreted protein compared to wild type FVII. The assay used for measuring FVII activity in this study is based on the ability of FVII, in complex with TF, to activate FX and subsequent cleavage of a FXa specific chromogenic substrate. To better evaluate the effect of the drugs on the biological activity of FVII in the screening, we therefore adjusted the volume of the conditioned media according to the FVII antigen level in the mutated sample. It is therefore possible that the drugs identified as enhancers of the p.Q160R variant indeed improves the interaction between the variant and TF, most likely through a direct interaction between the drug tested and the variant FVII molecule, resulting in a correction of the altered conformation of the mutant FVII molecule. Due to the nature of the assay used, it is also possible that some of the identified drugs could also target FX activity, however, control experiments showed that abexinostat or tyloxapol were not able to activate FX without the presence of FVII/FVIIa or influence FXa activity directly (data not shown). Notably, the efficacy of the mechanism may be dependent on the concentration of the drug tested since the increase in FVII activity after drug treatment was dose dependent. The same explanation may be the case for the interaction of either drug with the variant FVII in patients’ plasma ex vivo.
Abexinostat is an orally available experimental drug candidate used for treatment of various cancers21,22,23. It inhibits histone deacetylase (HDAC) activity, which is upregulated in many tumor types and therefore leads to accumulation of highly acetylated histones and thus increased gene transcription of tumor suppressor genes. This results in inhibition of proliferation of cancer cells and induction of apoptosis24. Interestingly, another HDAC inhibitor, nicotinamide25, was also identified as a positive hit in the screen. Tyloxapol, also known as triton WR1339, is a non-ionic detergent that is used as an inhaled surfactant that aids in liquefaction and removal of bronchopulmonary secretions and has proven to be well tolerated for this use26. It has also been shown to inhibit lipoprotein lipase, thus preventing triglyceride uptake27. Additionally, it also blocks plasma lipolytic activity, and thus the breakdown of triglyceride-rich lipoproteins28. Tyloxapol is also used to induce hyperlipidemia in animals, and in a tyloxapol induced, murine nonalcoholic fatty liver disease model, tyloxapol increased the expression of ER stress proteins like GRP78, pPERK and CHOP29.
Our next step was to treat the CHO-K1 cells overexpressing rFVII with these drugs to explore their cellular effect on FVII expression. We found that treating the overexpressing cells with abexinostat increased both the expression and activity of the rFVII-160R variant. Although, we cannot differentiate whether the increase in activity is solely due to the elevated protein levels or also enhanced biological activity of the variant protein, the increase in mRNA and intracellular protein levels does indicate an increase in F7 gene transcription, which is in line with the function of the drug. In a previous study, we found that another FDA-approved HDAC inhibitor, 4-phenylbutyrate (4-PBA), also induced mRNA expression of rFVII-160R30. In order to test how well the cells tolerate abexinostat we measured the viability of the cells following treatment. We observed decreased cell viability at all the doses tested, which is not surprisingly considering the grade 3 cytotoxic effects of abexinostat that have been reported in clinical trials for the treatment of lymphoproliferative disorders23. Thus, the potential for drug repurposing of abexinostat appears questionable, at least in the context of FVII deficiency as the current replacement therapy is well tolerated.
In contrast to abexinostat, tyloxapol did not affect F7 mRNA expression. Nor did it decrease the viability of the cells. Since our previous studies have shown that rFVII-160R is retained in the ER we wanted to explore if tyloxapol could restore the intracellular trafficking for this FVII variant. After treatment with tyloxapol we observed a clear co-localization of the rFVII-160R variant with the Golgi marker GRASP65 suggesting a normalized transport of the mutant FVII via GRASP proteins in response to treatment. GRASPs have been identified for their specific roles in Golgi stack formation31,32. They are also involved in regulation of protein trafficking through the Golgi and has been shown to function as chaperones required for efficient trafficking of transmembrane proteins such as TGFα, CD83, CD8α, and Frizzled4 to the cell surface33,34,35. Soluble signal peptide-free cargo proteins and transmembrane proteins have been found to be secreted out of the cell in an unconventional manner that bypass the Golgi apparatus but where the secretion is dependent on GRASPs. Overexpression of GRASP65 alone increased surface expression of ΔF508-CFTR in HEK293 cells36. Thus, tyloxapol may act as a chemical chaperone that aid in GRASP-dependent secretion of the FVII variant but this needs to be further investigated. The lack of consistency between the FVII antigen and activity levels following higher doses of tyloxapol treatment might also be explained by a chaperone function of the compound that leads to increased secretion of incorrectly folded FVII in an already stressed overexpression system. We have also previously reported that a chemical chaperone was able to increase secretion of FVII-Q160R30. The cellular effect of 4-PBA was even stronger than what we observed for abexinostat and tyloxapol at mRNA and protein level, most likely due to its dual function as an HDAC inhibitor and a chemical chaperon, however, it did not affect the activity of FVII-Q160 directly (data not shown).
In conclusion, we used HTS to identify the drugs abexinostat and tyloxapol as enhancers of the p.Q160R variant FVII activity both in vitro in a cell-based model and ex vivo in patients’ plasma, although the cytotoxicity associated with abexinostat renders it a less viable option for further studies. This proof-of-concept study underscores the potential for drug repurposing as a novel treatment approach for FVII deficiency, and future research involving a broader library of FDA-approved compounds may uncover additional suitable candidates.
Methods
Cell culture
The Chinese hamster ovary (CHO-K1) cell line (American Type Culture Collection, Rockville, MD, USA) were cultured in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with L-Proline, 10% fetal bovine serum (FBS), 10 µg/mL vitamin K1, 100 U/mL penicillin, and 100 µg/mL streptomycin in a humidified atmosphere containing 5% CO2 at 37 °C.
Expression vectors and transient transfections
The plasmid vector containing F7 cDNA for p.Q160R was generated using the Quick Change Site-Directed Mutagenesis II Kit (Agilent, Santa Clara, California, United States) according to the manufacturer’s instructions using pcDNA3-FVII-wt as template as previously described12. The empty vector pcDNA™3.1(+) (pcDNA3) was used as control (Thermo Fischer Scientific, Rockford, IL, MD, USA). CHO-K1 cells were seeded in 12 well plates and grown for 24 h before transient transfection of the plasmids with Lipofectamine LTX with Plus reagent diluted in Opti-MEM according to the manufacturer’s protocol.
FVII expression studies
Cell culture medium from CHO-K1 cells (conditioned medium) with transient expression of rFVII-wt or rFVII-160R was harvested and the cells were washed briefly with ice-cold phosphate-buffered saline (PBS) before lysis in RIPA buffer supplemented with 1:100 Halt Protease and Phosphatase Inhibitor Cocktail. Cell lysates and cell culture medium were pre-cleared by centrifugation and total protein content in the lysates was measured using the BCA protein assay kit (Thermo Fisher Scientific). ELISA was performed on conditioned medium and lysates using the VisuLize FVII Antigen ELISA Kit according to the manufacturer’s protocol or with FVII-EIA together with VisuLize Buffer Pak (all Affinity Biologicals, Ancaster, Ontario, Canada). Colorimetric output was measured on the SpectraMax Plus spectrophotometer.
High-throughput screening of drug library
High-throughput screening (HTS) for rFVII-160R mutant activity enhancement in conditioned medium from CHO-K1 cells transiently expressing the FVII-p.Q160R variant or the FVII-wild type (wt) was performed at the High-Throughput Chemical Biology Screening Platform at the Centre for Molecular Medicine Norway (NCMM), Faculty of Medicine, University of Oslo, using the Prestwick Chemical Library and SelleckChem Bioactives I Library (10 µM final concentration). The Prestwick Chemical Library consists of 1520 FDA-approved small molecule drugs whereas the SelleckChem Bioactives I Library contains 355 FDA or Phase I approved drugs that do not overlap with the Prestwick Chemical Library. Serum free conditioned medium from cells transiently expressing rFVII-wt or variant rFVII-160R were assayed in 384-well plates using a Beckman Coulter BioMek i7 pipetting robot. FVII activity was analyzed after 1.5 h incubation of the conditioned medium with library drugs at 37 °C using Biophen™ FVII chromogenic assay (Hyphen BioMed, Neuville-sur-Oise, France) according to the manufacturers protocol. The absorbance was measured at 405 nm for two hours at 37 °C on a Synergy Neo2 plate reader (Agilent, BioTek, Santa Clara, United States). Equal amounts of FVII antigen were loaded onto the assay plates. Conditioned medium from cells transiently transfected with pcDNA3-empty vector or FVII-wt were used as negative or positive controls, respectively. Treatment medium (not used with cells) was used as blank.
In vitro treatment with selected compounds
For cellular experiments, CHO-K1 cells were seeded in 12-well plates at a density of 13 × 104 cells/well, transfected and allowed to grow for 24 h before changing to phenol red-free DMEM without FBS, supplemented with L-glutamine, L-proline and 10 µg/mL vitamin K1 prior to cell treatment. The cells were stimulated with abexinostat (PCI-24781, TargetMol Chemicals Inc., Boston, USA), a deacetylase inhibitor, or tyloxapol (Prestw-954), a surfactant for mucus removal, for 24 h at 37 °C with indicated concentrations (0-100 µM). Treatment medium incubated with indicated concentrations of abexinostat or tyloxapol were included as a control.
qRT-PCR
Total RNA was isolated using the MagMAX-96 Total RNA Isolation Kit on a MagMAX Express-96 Deep Well Magnetic Particle Processor (both from Thermo Fisher Scientific). Equal amounts of mRNA were reverse transcribed using the qScript cDNA SuperMix (Quantabio, Massachusetts, United States). Analysis of mRNA levels were performed using quantitative RT-PCR (qRT-PCR) with the TaqMan Gene Expression Master Mix on a 7900HT Fast Real-Time PCR system with F7 (Hs01551992_m1) and 18 S rRNA endogenous Control (all from Thermo Fisher Scientific) TaqMan assays.
FVII deficient plasma samples
Seven patients homozygous for the FVII-p.Q160R mutation and with FVII coagulant (FVII: C) activity of < 1% who attended the outpatient annual consultation were recruited during a follow-up at the Haemophilia Comprehensive Care Centre at Oslo University Hospital, Rikshospitalet, in 2019. The blood samples were collected in tubes containing trisodium citrate (0.109 M/3.2%) and centrifuged at 2500 x g for 15 min at room temperature within 1 h. Plasma was collected and frozen at -80 °C until analysis. The research was approved by the Regional Committee for Medical and Health Research Ethics in Norway and performed in accordance with the Declaration of Helsinki, with written informed consent obtained from all the patients.
Treatment of patients’ plasma with selected compounds
FVII activity was analyzed in plasma samples from patients and controls at the Centre for Molecular Medicine Norway (NCMM) using the same protocol as described above. Prior to analysis, the samples were incubated with increasing concentrations of abexinostat or tyloxapol (0.1 µM-100 µM) for 1.5 h at 37 °C. Equal amounts of FVII antigen of each sample were loaded onto the assay plates. Pooled normal plasma with FVII-wt was used as a positive control.
Cell viability
For determination of cell viability, 6 × 103 CHO-K1 cells/well were seeded in a 96-well plate in 100 µL complete DMEM with L-Proline and subsequently shifted into phenol red-free DMEM with L-Proline prior to stimulation with different concentrations of abexinostat or tyloxapol for 24 h. 10 µL of Cell Counting Kit – 8 (Sigma Aldrich, Darmstadt, Germany) were added into the media before incubation at 37 °C in an incubator with humidified atmosphere and 5% CO2 for one hour. The absorbance was measured at 450 nm using a Spectra Max Plus microplate reader.
Confocal Immunofluorescence microscopy
Cells were seeded in 2-well Ibidi chamber slides (Ibidi, Gräfeling; Germany) and transiently transfected with pcDNA-FVII-wt or pcDNA3-p.Q160R cDNA constructs and grown for 24 h post transfection. The cells were then stimulated with tyloxapol (10 and 50 µM) for 24 h at 37 °C before immunostaining was performed. Cells were fixed with paraformaldehyde and blocked for 1 h with PBS containing 10% donkey serum before incubation with primary antibodies against FVII (R&D Systems, Minneapolis, MN, USA) and either the ER marker protein disulfide isomerase (PDI) (Enzo Life Sciences, Farmingdale, NY, USA), the Golgi marker (GM) protein 130 (BD Biosciences, New Jersey, USA), trans Golgi network (TGN) 46 (Novus Biologicals, Minneapolis, USA), coat protein (COP) II (Invitrogen), Ras related protein (Rab)-8 (LSBio, Washington, USA), Rab-11 (BD Biosciences), endoplasmic-reticulum–Golgi intermediate compartment (ERGIC)-53 (Santa Cruz, Dallas, USA), or the Golgi markers Golgi reassembly stacking proteins (GRASP)55 (Santa Cruz) and GRASP65 (Invitrogen). After washing with PBS, cells were incubated with the secondary antibodies Alexa Fluor® 488 donkey anti-goat and Alexa Fluor® 568 donkey anti mouse or 568 donkey anti-rabbit (Invitrogen, Thermo Fisher Scientific). Negative controls with only secondary antibodies and double negative controls with one of the primary antibodies and both secondary antibodies were included. All incubations were done for 1 h at RT in the dark. Cells were mounted in the ProLong Glass Antifade Mountant with NuncBlue™ (Thermo Fisher Scientific) and examined with a Zeiss LSM 980 Airyscan 2 confocal microscope (Carl Zeiss MicroImaging GmbH, Jena, Germany) equipped with Diode lasers (405/445/488/514/639nm), and a DPSS laser (561 nm). The objective used was a Zeiss plan-Apochromat 63xNA/1.4 oil. Image acquisition and analysis were performed with basic software ZEN 3.8 (Carl Zeiss MicroImaging GmbH, Jena, Germany). The Pearsons colocalization measurements were performed with ZEN 3.8.
Statistical analysis
HTS data and screening of plasma samples were analyzed using custom workflow developed in KNIME software. All data were analyzed according to initial velocity (V0) and absorbance at two h (A405). Hits were identified by analyzing samples based on their deviations from statistics on the entire sample population using standard deviation (SD) and interquartile range (IQR). Samples were considered hits if they fall outside 3 SD from the sample means for either V0% or A405% or if the samples fall outside 1.5*IQR for either V0% or A405. Additional criteria included were: (1) having the correct slope (increasing curve for enhancers, decreasing curve for inhibitors), (2) showing a change in the upper and lower limit of the curves of at least 2%, (3) having an EC50 (half maximal effective concentration) less than the maximum dose tested (100 µM).
For other data the statistical analyses were performed using GraphPad Prism 10.0 (GraphPad Software, La Jolla, California, United State). Comparisons between unstimulated and stimulated cells were performed using one-way ANOVA with Bonferroni-corrected tests for multiple comparisons. A p-value of < 0.05 was considered as statistically significant (*p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001).
Gene variant nomenclature
The official HGVS recommendation for the FVII p.Q160R gene variant is NM_000131.4:c.479 A > G (cDNA) and NP_000122.1:p.Gln160Arg (protein)37.
Data availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
References
S Hagen, F. et al. Characterization of a cDNA coding for human factor VII. Proc. Natl. Acad. Sci. U S A. 83, 2412–2416. https://doi.org/10.1073/pnas.83.8.2412 (1986).
Rao, L. V. & Rapaport, S. I. Activation of factor VII bound to tissue factor: a key early step in the tissue factor pathway of blood coagulation. Proc. Natl. Acad. Sci. U. S. A. 85, 6687–6691, (1988). https://doi.org/10.1073/pnas.85.18.6687
Girolami, A., Bertozzi, I., de Marinis, G. B., Bonamigo, E. & Fabris, F. Activated FVII levels in factor VII Padua (Arg304Gln) coagulation disorder and in true factor VII deficiency: a study in homozygotes and heterozygotes. Hematology 16, 308–312. https://doi.org/10.1179/102453311x13085644680069 (2011).
Palla, R., Peyvandi, F. & Shapiro, A. D. Rare bleeding disorders: diagnosis and treatment. Blood 125, 2052–2061. https://doi.org/10.1182/blood-2014-08-532820 (2015).
Mariani, G., Bernardi, F., Factor, V. I. I. & Deficiency Semin Thromb. Hemost. 35, 400–406, doi:https://doi.org/10.1055/s-0029-1225762 (2009).
Perry, D. J., Factor, V. I. I. & Deficiency Br. J. Haematol. 118, 689–700, doi:https://doi.org/10.1046/j.1365-2141.2002.03545.x (2002).
Borhany, M. et al. Bleeding disorders in the tribe: result of consanguineous in breeding. Orphanet J. Rare Dis. 5 https://doi.org/10.1186/1750-1172-5-23 (2010).
Bernardi, F., Mariani, G. & Clinical Laboratory, and molecular aspects of factor VII deficiency. Semin Thromb. Hemost. https://doi.org/10.1055/s-0044-1788792 (2024).
McVey, J. H., Boswell, E., Mumford, A. D., Kemball-Cook, G. & Tuddenham, E. G. Factor VII deficiency and the FVII mutation database. Hum. Mutat. 17, 3–17. https://doi.org/10.1002/1098-1004(2001)17:1<3::AID-HUMU2>3.0.CO;2-V (2001).
Kavlie, A., Orning, L., Grindflek, A., Stormorken, H. & Prydz, H. Characterization of a factor VII molecule carrying a mutation in the second epidermal growth factor-like domain. Thromb. Haemost. 79, 1136–1143 (1998).
Hunault, M., Arbini, A. A., Carew, J. A., Peyvandi, F. & Bauer, K. A. Characterization of two naturally occurring mutations in the second epidermal growth factor-like domain of factor VII. Blood 93, 1237–1244 (1999).
Andersen, E. et al. Activation of Endoplasmic reticulum stress and unfolded protein response in congenital factor VII deficiency. Thromb. Haemost. 118, 664–675. https://doi.org/10.1055/s-0038-1637690 (2018).
Kemball-Cook, G. et al. Coagulation factor VII Gln100 --> Arg. Amino acid substitution at the epidermal growth factor 2-protease domain interface results in severely reduced tissue factor binding and procoagulant function. J. Biol. Chem. 273, 8516–8521. https://doi.org/10.1074/jbc.273.14.8516 (1998).
Bernardi, F. & Mariani, G. Biochemical, molecular and clinical aspects of coagulation factor VII and its role in hemostasis and thrombosis. Haematologica 106, 351–362. https://doi.org/10.3324/haematol.2020.248542 (2021).
Krishnamurthy, N., Grimshaw, A. A., Axson, S. A., Choe, S. H. & Miller, J. E. Drug repurposing: a systematic review on root causes, barriers and facilitators. BMC Health Serv. Res. 22, 970. https://doi.org/10.1186/s12913-022-08272-z (2022).
Pushpakom, S. et al. Drug repurposing: progress, challenges and recommendations. Nat. Rev. Drug Discov. 18, 41–58. https://doi.org/10.1038/nrd.2018.168 (2019).
Ashburn, T. T. & Thor, K. B. Drug repositioning: identifying and developing new uses for existing drugs. Nat. Rev. Drug Discov. 3, 673–683. https://doi.org/10.1038/nrd1468 (2004).
Xiao, W., Li, C. Q., Xiao, X. P. & Lin, F. Z. Expression and fast Preparation of biologically active Recombinant human coagulation factor VII in CHO-K1 cells. Genet. Mol. Res. 12, 6813–6824. https://doi.org/10.4238/2013.December.16.7 (2013).
Peng, L. et al. Enhanced Recombinant factor VII expression in Chinese hamster ovary cells by optimizing signal peptides and fed-batch medium. Bioengineered 7, 189–197. https://doi.org/10.1080/21655979.2016.1176656 (2016).
Böhm, E. et al. Differences in N-glycosylation of Recombinant human coagulation factor VII derived from BHK, CHO, and HEK293 cells. BMC Biotechnol. 15, 87. https://doi.org/10.1186/s12896-015-0205-1 (2015).
Aggarwal, R. et al. Inhibiting histone deacetylase as a means to reverse resistance to angiogenesis inhibitors: phase I study of abexinostat plus pazopanib in advanced solid tumor malignancies. J. Clin. Oncol. 35, 1231–1239. https://doi.org/10.1200/jco.2016.70.5350 (2017).
Lian, B., Chen, X. & Shen, K. Inhibition of histone deacetylases attenuates tumor progression and improves immunotherapy in breast cancer. Front. Immunol. 14, 1164514. https://doi.org/10.3389/fimmu.2023.1164514 (2023).
Ribrag, V. et al. Safety and efficacy of abexinostat, a pan-histone deacetylase inhibitor, in non-Hodgkin lymphoma and chronic lymphocytic leukemia: results of a phase II study. Haematologica 102, 903–909. https://doi.org/10.3324/haematol.2016.154377 (2017).
Manal, M., Chandrasekar, M. J., Gomathi Priya, J. & Nanjan, M. J. Inhibitors of histone deacetylase as antitumor agents: A critical review. Bioorg. Chem. 67, 18–42. https://doi.org/10.1016/j.bioorg.2016.05.005 (2016).
Lawson, M. et al. Inhibitors to understand molecular mechanisms of NAD(+)-dependent deacetylases (sirtuins). Biochim. Biophys. Acta. 1799, 726–739. https://doi.org/10.1016/j.bbagrm.2010.06.003 (2010).
Koppitz, M. et al. Mucolytic effectiveness of tyloxapol in chronic obstructive pulmonary Disease - A Double-Blind, randomized controlled trial. PLoS One. 11, e0156999. https://doi.org/10.1371/journal.pone.0156999 (2016).
Loginova, V. M., Tuzikov, F. V., Tuzikova, N. A. & Korolenko, T. A. Comparative characteristics of lipemia models induced by injections of Triton WR-1339 and poloxamer 407 in mice. Bull. Exp. Biol. Med. 155, 284–287. https://doi.org/10.1007/s10517-013-2133-1 (2013).
Korolenko, T. A., Tuzikov, F. V., Vasil’eva, E. D., Cherkanova, M. S. & Tuzikova, N. A. Fractional composition of blood serum lipoproteins in mice and rats with Triton WR 1339-induced lipemia. Bull. Exp. Biol. Med. 149, 567–570. https://doi.org/10.1007/s10517-010-0994-0 (2010).
Jin, M. et al. Erythritol improves nonalcoholic fatty liver disease by activating Nrf2 antioxidant capacity. J. Agric. Food Chem. 69, 13080–13092. https://doi.org/10.1021/acs.jafc.1c05213 (2021).
Andersen, E. et al. The effect of the chemical chaperone 4-phenylbutyrate on secretion and activity of the p.Q160R missense variant of coagulation factor FVII. Cell. Biosci. 9, 69. https://doi.org/10.1186/s13578-019-0333-8 (2019).
Ahat, E., Li, J. & Wang, Y. New insights into the golgi stacking proteins. Front. Cell. Dev. Biology. 7, 131. https://doi.org/10.3389/fcell.2019.00131 (2019).
Zhang, X. & Wang, Y. Nonredundant roles of GRASP55 and GRASP65 in the golgi apparatus and beyond. Trends Biochem. Sci. 45, 1065–1079. https://doi.org/10.1016/j.tibs.2020.08.001 (2020).
Kuo, A., Zhong, C., Lane, W. S. & Derynck, R. Transmembrane transforming growth factor-alpha tethers to the PDZ domain-containing, golgi membrane-associated protein p59/GRASP55. EMBO J. 19, 6427–6439. https://doi.org/10.1093/emboj/19.23.6427 (2000).
D’Angelo, G. et al. GRASP65 and GRASP55 sequentially promote the transport of C-terminal valine-bearing cargos to and through the golgi complex. J. Biol. Chem. 284, 34849–34860. https://doi.org/10.1074/jbc.M109.068403 (2009).
Stein, M. F. et al. CD83 and GRASP55 interact in human dendritic cells. Biochem. Biophys. Res. Commun. 459, 42–48. https://doi.org/10.1016/j.bbrc.2015.02.057 (2015).
Gee, H. Y., Noh, S. H., Tang, B. L., Kim, K. H. & Lee, M. G. Rescue of ∆F508-CFTR trafficking via a GRASP-dependent unconventional secretion pathway. Cell 146, 746–760. https://doi.org/10.1016/j.cell.2011.07.021 (2011).
den Dunnen, J. T. et al. HGVS recommendations for the description of sequence variants: 2016 update. Hum. Mutat. 37, 564–569. https://doi.org/10.1002/humu.22981 (2016).
Funding
The research was funded by Oslo University Hospital – Fondsstiftelsen (2018-57) and the South-Eastern Norway Regional Health Authorities (2019071).
Author information
Authors and Affiliations
Contributions
M.S.A. performed experiments, analysed the data and wrote the manuscript. M.C.M. and E.A. participated in performing the experiments. E.S. performed confocal microscopy imaging and analyses. P.M.S. provided funding for the study, interpreted results and edited the manuscript. B.S. and M.E.C. conceived and designed the study, interpreted results and edited the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Andresen, M.S., Mowinckel, M.C., Skarpen, E. et al. Identification and evaluation of Pharmacological enhancers of the factor VII p.Q160R variant. Sci Rep 15, 14315 (2025). https://doi.org/10.1038/s41598-025-98689-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98689-3