Abstract
Slow- and non-growing bacterial populations, along with intracellular pathogens, often evade standard antibacterial treatments and are linked to persistent and recurrent infections. This necessitates the development of therapies specifically targeting nonproliferating bacteria. To identify compounds active against non-growing uropathogenic Escherichia coli (UPEC) we performed a drug-repurposing screen of 6454 approved drugs and drug candidates. Using dilution-regrowth assays, we identified 39 compounds that either kill non-growing UPEC or delay its regrowth post-treatment. The hits include fluoroquinolones, macrolides, rifamycins, biguanide disinfectants, a pleuromutilin, and anti-cancer agents. Twenty-nine of the hits have not previously been recognized as active against non-growing bacteria. The hits were further tested against non-growing Pseudomonas aeruginosa and Staphylococcus aureus. Ten compounds – solithromycin, rifabutin, mitomycin C, and seven fluoroquinolones—have strong bactericidal activity against non-growing P. aeruginosa, killing >4 log10 of bacteria at 2.5 µM. Solithromycin, valnemulin, evofosfamide, and satraplatin are unique in their ability to selectively target non-growing bacteria, exhibiting poor efficacy against growing bacteria. Finally, 31 hit compounds inhibit the growth of intracellular Shigella flexneri in a human enterocyte infection model, indicating their ability to permeate the cytoplasm of host cells. The identified compounds hold potential for treating persistent infections, warranting further comparative studies with current standard-of-care antibiotics.
Similar content being viewed by others
Introduction
All currently used antibiotics were discovered based on their ability to inhibit bacterial growth1. However, only a few can effectively kill non-growing bacteria, which are prevalent in chronic and recurrent infections2. The ability of bacteria to survive treatment with bactericidal antibiotics without proliferation is referred to as antibiotic tolerance or antibiotic persistence. These terms describe bacterial survival in the presence of a killing drug, enabling evasion of conventional antibacterial therapies. Importantly, tolerance and persistence are temporary, transient phenotypic traits that manifest in the absence of growth. This contrasts with antibiotic resistance, a genetically acquired trait that allows bacteria to grow in the presence of the drug3. Notably, evasion of killing through tolerance or persistence can increase the likelihood of resistance development4,5. Non-growing bacteria in stationary-phase cultures are inherently tolerant to most antibiotics. In growing bacterial cultures, a subpopulation of non-growing cells, known as persisters, can transiently survive exposure to bactericidal antibiotics and resume growth once the drug pressure is removed6,7,8. However, the connection between these in vitro persisters and persistent infections in the clinical settings remains uncertain and is challenging to investigate9,10. Furthermore, chronic infections are often caused by intracellular bacteria as well as by biofilms, which both evade the immune defense and antibiotics11,12,13,14. To effectively treat these infections and curb the spread of resistance, there is an urgent need for drugs that selectively target non-growing and intracellular bacteria. These drugs must be devoid of severe side effects and either possess antibacterial activity on their own or enhance conventional antibiotics.
In this study, we performed a high-throughput screening to identify compounds that selectively target non-growing Gram-negative bacteria using a dilution-regrowth assay15. Specifically, drug-treated stationary phase culture samples were diluted into fresh medium, and the time to outgrowth was measured as a proxy for the number of bacteria that survived the treatment. For this purpose, we utilized drug repurposing, a method of assessing previously approved drugs or candidates for new medical applications. Using a library of approved and candidate drugs with known safety and pharmacokinetic properties excluded reactive and toxic compounds that might otherwise come up as false hits in the screen.
In our primary screen we used uropathogenic Escherichia coli (UPEC), a clinically important pathogen and a model organism for other Gram-negative pathogens. UPEC is a prevalent cause of recurrent urinary tract infections (UTIs)16, which are among the most common outpatient bacterial infections17 and exhibit high treatment failure rates18,19. UPEC can reside both extracellularly and intracellularly, forming persistent intracellular bacterial reservoirs in urinary epithelial cells and macrophages20,21. Reactivation of quiescent bacteria in the urinary tract may be one cause of recurrent UTIs, along with potential reinfection originating from the host’s intestinal tract22,23,24. To identify drug candidates targeting intracellularly persisting, intravacuolar bacteria, the screen was performed in an acidic, low-phosphate, and low-magnesium medium that is designed to mimic conditions in intravacuolar reservoirs, where quiescent UPEC resides within host cells22,25.
After characterizing the effects of the hit compounds on non-growing UPEC, we tested their activities against stationary phase cultures of Pseudomonas aeruginosa and Staphylococcus aureus to explore their potential broader use. These two pathogens were selected due to their prevalence in chronic biofilm infections26,27. Finally, to assess the capacity of the candidate compounds to permeate through the host cell cytoplasmic membrane barrier, we characterized their inhibitory activity against Shigella flexneri. Unlike UPEC, which resides in acidified vacuoles, S. flexneri replicates in the cytosol of intestinal epithelial cells, where the pH is neutral rather than acidic28. In the absence of a licensed Shigella vaccine, antibiotics remain essential for controlling mortality in vulnerable populations, including children under five and the elderly in low- and middle-income countries. Unfortunately, over the past two decades, multidrug-resistant and extensively drug-resistant S. flexneri and Shigella sonnei strains have emerged globally, including recently in sexually transmitted infections in the global North29. As a consequence, in 2024 the WHO included Shigella on its list of high-priority antibiotic-resistant pathogens30.
Using stationary phase culture as a model for non-growing condition, we identified 29 candidate compounds that were not previously recognized for their ability to affect non-growing bacteria. These compounds either killed stationary-phase UPEC or delayed its outgrowth without causing bacterial death. Notably, many of these compounds were even more bactericidal against non-growing P. aeruginosa, while some were active also against S. aureus.
Results
A dilution-regrowth screen identifies compounds that delay the regrowth of non-growing UPEC
We conducted a screen of 6454 registered drugs and drug candidates, aiming to identify compounds effective against non-growing UPEC strain CFT07331. This collection comprised 1200 compounds from the Prestwick Library and 5254 from the Specs Repurposing Library. The Prestwick Library primarily consists of off-patent, regulator-approved drugs from diverse therapeutic classes, including 144 antibiotics and 12 antiseptics, while the Specs Library contains commercially available drugs, drug candidates in clinical development phases 1 through 3, and compounds in preclinical development. All compounds were tested at a final concentration of 20 μM.
Bacteria were cultured in either 1:4 diluted cation-adjusted Mueller-Hinton broth (CA-MHB) at pH 7.4 or in an acidic, low-phosphate, low-magnesium medium (LPM) at pH 5.5. CA-MHB was diluted to reduce bacterial density in the stationary phase culture, which, based on our observations, we anticipated to minimize bacterial clumping and thereby reduce the pipetting error. Acidic LPM was chosen to simulate conditions in UPEC-inhabited vacuoles22,25. Given that variation in antibiotic tolerance decreases when cultures remain in the stationary phase for extended periods or are inoculated from such cultures32,33, we used a 24-h cultivation and treatment time in both the screening and validation experiments to minimize stochasticity and variability.
The screening assay involved treating a stationary-phase culture with each compound for 24 h, followed by monitoring the delay in bacterial outgrowth after a 2500-fold dilution into drug-free growth medium (Fig. 1A)15. This dilution reduced the compound concentration to 8 nM, which was expected to be below their minimum inhibitory concentration (MIC), thus allowing the regrowth of surviving bacteria. This assumption was confirmed, as the lowest measured MIC for all hit compounds was 12.5 nM (clinafloxacin, see Dataset 1). However, we cannot rule out the possibility that the remaining 8 nM drug residue might partially inhibit growth in certain cases.
A Schematic of the screening assay. A 24-h culture of UPEC strain CFT073 was dispensed into a microtiter plate and treated with 20 μM compounds from the collection for 24 h. The samples were then diluted 2500-fold into drug-free CA-MHB (pH 7.4), and OD600 was measured after 6 h. B Regrowth delay following bactericidal treatment. For assay validation, UPEC CFT073 was cultivated for 24 h in 1:4 diluted CA-MHB (pH 7.4) and treated for 24 h with 20 μM gatifloxacin (GAT) or finafloxacin (FIN), which kill non-growing bacteria and served as positive controls for screening. After a 2500-fold dilution into drug-free CA-MHB, the regrowth of the drug-treated samples was delayed compared to that of the drug-free control (DMSO). C, D Screening of the combined Prestwick and SPECS collections identified drugs that delayed bacterial regrowth in 1:4 diluted CA-MHB (pH 7.4) (C) and LPM (pH 5.5) (D). A cutoff of OD600 < 0.1 (dashed line) was used to identify hits (red). Most of the tested compounds (black) showed no effect compared to the drug-free control (purple). GAT (green) and FIN (blue) were included as positive controls in each plate. E Pie chart illustrating the distribution of validated hits across different drug groups. F Venn diagram depicting the overlap of validated hits identified in 1:4 CA-MHB (pH 7.4) and LPM (pH 5.5).
To validate the assay, we used gatifloxacin (GAT) and finafloxacin (FIN) as positive controls, while mock-treated samples (1% DMSO without antibiotics) served as negative controls (Fig. 1B, Fig. S1). GAT has previously been shown to kill UPEC persisters34, while FIN has bactericidal activity at acidic pH and kills effectively intracellular UPEC in a cell culture model35,36. Preliminary experiments confirm that both GAT and FIN have bactericidal effects against stationary-phase UPEC cultures at a concentration of 20 µM. The Z'-factor, indicating assay robustness and discrimination between positive controls and mock treatments, was above 0.5 between 5 and 8 h after dilution (Fig. S1), demonstrating excellent assay reliability within this timespan.
In the course of the screening, we measured the optical density of regrowing samples 6 h post-dilution, defining wells with an OD600 < 0.1 as hits. GAT, FIN, and DMSO controls were included on every screening plate to ensure consistency (Fig. 1C, D). After eliminating duplicates—compounds present in both libraries or those appearing in different chemical forms (e.g., the hydrochloride salt and free base of the same fluoroquinolone)—we identified 54 hits in 1:4 CA-MHB (pH 7.4) and 38 hits in LPM (pH 5.5), with 23 overlapping hits active in both media.
Hit validation and dose–response analysis
Hits from the primary screen were validated through a dilution-regrowth assay at 20, 10, and 5 μM concentrations in both 1:4 CA-MHB pH 7.4 and LPM pH 5.5 (Fig. S2). Compounds that delayed regrowth, resulting in an OD600 at least 50% lower than the drug-free control at one or more of these concentrations after 6 h of incubation in regrowth medium, were selected for further testing at concentrations ranging from 30 to 0.25 μM. We identified 39 compounds of six different classes that significantly delayed regrowth at one or more of these concentrations (Fig. 1E). Of these compounds, 37 were active in 1:4 CA-MHB, 17 in acidic LPM and 15 in both media (Figs. 1F, 2, and 3).
Heatmap showing the regrowth delay and killing of non-growing UPEC CFT073 by validated hit compounds. Gray areas indicate compounds not tested for killing due to weak activity in regrowth-delay experiments. Bacteria were grown in 1:4 CA-MHB (pH 7.4) or LPM (pH 5.5) for 24 h and then treated with the compounds at the indicated concentrations for 24 h. Regrowth data were obtained by measuring OD600 6 h after a 2500-fold dilution of the samples into CA-MHB. Killing data were determined by spot-plating serial dilutions of the treated samples on LB agar plates followed by colony counting. The differences in CFU/mL between the drug-treated samples and the drug-free control are shown. Data represent the mean of three biological replicates. The significance of the regrowth delay was assessed using one-way ANOVA followed by Dunnett’s test, comparing each treatment to the drug-free control. Asterisks denote p-values from the Dunnett’s test.
Heatmap showing the regrowth delay of non-growing UPEC CFT073 by validated hit compounds that did not kill the stationary phase bacteria. Cultures were grown in 1:4 CA-MHB (pH 7.4) or LPM (pH 5.5) for 24 h and then treated with the compounds at the indicated concentrations for another 24 h. OD600 was measured 6 h after a 2500-fold dilution in CA-MHB. PML refers to pleuromutilin. Data represent the average of three biological replicates. Regrowth delay significance was assessed using one-way ANOVA and Dunnett’s test, with comparisons made against the drug-free control. Asterisks indicate p-values from Dunnett’s test.
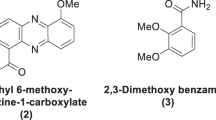
Of the 39 compounds, 29 are well-known antibiotics. While ofloxacin, ciprofloxacin37,38, tosufloxacin, sparfloxacin, moxifloxacin, gatifloxacin, enrofloxacin, sarafloxacin34,39 as well as rifampicin40,41 have been previously identified as active against non-growing bacteria, to the best of our knowledge, this has not been demonstrated for the remaining 20 antibiotics that were hits from the screen. The largest group consists of 19 fluoroquinolones, including 18 hits from the screen, as well as finafloxacin which was used as a positive control. Other antibiotic classes include protein synthesis inhibitors: five macrolides and one pleuromutilin (valnemulin), as well as four RNA synthesis-inhibiting rifamycins. The list also includes three antiseptics and disinfectants: the biguanide octenidine, and the bisbiguanides alexidine and chlorhexidine.
Hit compounds that are neither antibiotics nor cationic surfactants, are anti-cancer agents with varying mechanisms of action and at different stages of development. Mitomycin C (MMC)42, bleomycin (BLE)43, satraplatin (SAT)44, and evofosfamide (EVO)45 are known genotoxic compounds targeting DNA integrity and synthesis. Echinomycin and plicamycin (also known as mithramycin) are DNA-intercalating antitumor drugs that block transcription46. A deubiquitinase inhibitor Degrasyn (DGS, WP1130) is a thiol-reactive compound that modifies cysteine residues47,48.
In summary, our screen identified numerous compounds that were previously unknown to be active against non-growing UPEC.
Both killing and the post-antibiotic effect contribute to delaying UPEC regrowth
While setting up the screen, we anticipated that the killing of non-growing bacteria would be the primary cause of delayed regrowth. However, an alternative explanation could be the post-antibiotic effect (PAE), in which the regrowth of individual bacteria is temporarily delayed after the antibiotic is removed from the extracellular environment49. It is also possible that both bacterial killing and PAE occur simultaneously.
To differentiate between these scenarios, we used CFU counting by agar plating to assess the bactericidal effect on non-growing bacteria. A reduction in CFU indicates bacterial killing and suggests that the delay in regrowth is due to the loss of viable cells. Conversely, if no significant reduction in CFU is observed, the regrowth delay is due to PAE without killing. This analysis was performed for all compounds that demonstrated activity in the dilution-regrowth assay at a concentration of 10 μM (Fig. S2). Fluoroquinolones, anti-cancer agents, and disinfectants do kill a fraction of stationary phase UPEC (Fig. 2), whereas macrolides, rifamycins, and valnemulin are not bactericidal against E. coli but rather cause PAE (Fig. 3, Dataset 2). The occurrence of PAE indicates that these drugs penetrate the non-growing bacteria and remain there for hours, inhibiting targets and postponing regrowth. Fluoroquinolones are known to cause PAE after treatment of growing bacterial cultures50. We compared the bactericidal activity of each compound based on the log killing at a 2.5 μM concentration and regrowth-inhibiting activity by determining the EC50 values, which were calculated using the OD600 readings from treated and diluted stationary phase samples after a 6 h incubation period. Here, EC50 represents the concentration of a compound that causes a regrowth delay, halfway between the baseline (no regrowth inhibition, with OD600 of the drug-free control) and the maximum effect (complete inhibition of regrowth, with OD600 of the sterile medium) (Dataset 1). We found that fluoroquinolones with similar EC50 exhibit different bactericidal activity, although these two factors are correlated (r = −0.67; 95% CI = −0.86 to −0.29; p = 0.0025) (Fig. S3A). This indicates that both reduction of the inoculum by killing and the PAE of the surviving bacteria contributed to the observed regrowth delay by fluoroquinolones (Fig. 2). Finally, we found that sitafloxacin is the most potent and bactericidal compound against non-growing UPEC at pH 7.4, considerably exceeding ciprofloxacin, which is recommended for the treatment of uncomplicated pyelonephritis and complicated UTIs51,52.
Impact of pH and medium composition on activity against non-growing UPEC
The majority of the hit compounds were less effective in LPM (pH 5.5) compared to 1:4 CA-MHB (pH 7.4). Several fluoroquinolones, macrolides, valnemulin, and chlorhexidine were active at pH 7.4 and completely inactive in the acidic medium (Figs. 2 and 3). In particular, the bactericidal activity of all the fluoroquinolones, except finafloxacin, drops significantly at acidic pH (Fig. 2, Fig. S3A,B). Conversely, the rifamycins, alexidine, and octenidine, as well as the anti-cancer agents evofosfamide, mitomycin C, satraplatin, and plicamycin, are potentiated by the low pH of the medium (Figs. 2 and 3). In total, eleven compounds are more active in LPM (pH 5.5) than in 1:4 CA-MHB (pH 7.4) (Fig. S4).
Recently, the Collins lab identified semapimod, an anti-inflammatory drug with anti-membrane activity, as effective against stationary-phase E. coli and Acinetobacter baumannii using a similar screening procedure53. Although semapimod was included in our library, it was not among our hits. Zheng and colleagues treated stationary-phase E. coli cultures grown in 1% LB diluted in phosphate-buffered saline (PBS)53 while our experimental setup differed in several aspects, including the E. coli strains used, screening concentrations, and the dilution factor of the stationary-phase culture. To investigate how the screening procedure influences the results, we tested semapimod using both protocols and strains. As shown in Fig. S5, the growth and treatment medium appear to play a key role in semapimod activity. Semapimod exhibits strong bactericidal activity (Fig. S5A) and delays regrowth (Fig. S5B, C) in 1% LB diluted in PBS but not in 1:4 CA-MHB. Other factors had comparatively minor effects.
Thus, the use of different media by Zheng and colleagues, compared to our 1:4 CA-MHB, likely explains the differing screening results and aligns with their finding that semapimod’s activity is influenced by divalent cation concentration, as the addition of 21 mM Mg2+ abolished its activity53.
In summary, we observed that the activity of antimicrobials against non-growing UPEC is strongly influenced by the composition of the testing medium, particularly its pH.
Hit compounds have different activity profiles against non-growing P. aeruginosa and S. aureus
To determine the spectrum of activity of the compounds that were effective against non-growing UPEC, we further assessed their efficacy against the well-characterized Gram-negative and Gram-positive reference strains P. aeruginosa DSM1117 and S. aureus DSM2569, respectively. The cultures were grown and treated for 24 h in 1:4 CA-MHB (pH 7.4). Twenty four compounds that were identified as the most active in preliminary dilution-regrowth tests at a concentration of 10 μM were further characterized for regrowth delay and bactericidal activity at concentrations ranging from 10 to 0.1 μM (Fig. S2).
For better characterization of the compounds causing the strongest regrowth delay, we performed the regrowth step of the dilution-regrowth experiments on a plate reader, measuring the OD600 at 20-min intervals for over 20 h instead of using an endpoint measurement. This approach allowed us to capture the time when cultures reached a threshold optical density (start-growth-time, SGT15).
P. aeruginosa is notorious for causing resilient infections that do not respond well to antibiotics26. Therefore, we were surprised to find that many drugs, especially fluoroquinolones, were active against non-growing P. aeruginosa DSM1117 (Fig. 4). Strikingly, the bactericidal activity of the tested drugs against this P. aeruginosa strain is more potent compared to their activity against UPEC CFT073 (Figs. 2 and 4, Fig. S3A,C). Of the 24 compounds that are most active against P. aeruginosa based on preliminary regrowth-dilution results, all are also effective at killing nongrowing bacteria of this species, including those that induced only a post-antibiotic effect (PAE) without reducing CFU in UPEC.
Regrowth delay and killing of non-growing P. aeruginosa DSM1117 and S. aureus DSM2569 by compounds effective against non-growing UPEC. Gray areas in the heat map indicate compounds not tested due to inactivity in preliminary experiments. Cultures were grown in 1:4 CA-MHB (pH 7.4) for 24 h followed by treatment with the compounds at the indicated concentrations for an additional 24 h. To assess regrowth, OD600 was measured on a microplate reader after a 2500-fold dilution into CA-MHB. The time required for cultures to reach an OD600 threshold of 0.12 is reported as the start-growth-time (SGT). Bacterial killing was determined by spot-plating serial dilutions of the treated samples on LB agar plates followed by colony counting. The differences in CFU/mL between drug-treated samples and the drug-free control are presented. Data represent the average of three biological replicates. The significance of regrowth delay was evaluated using OD600 measurements taken 8 h after dilution into drug-free media. Statistical significance was assessed using one-way ANOVA followed by Dunnett’s test, comparing each treatment to the drug-free control. Asterisks denote p-values from Dunnett’s test.
Notably, solithromycin (a macrolide) and rifabutin (a rifamycin) were highly bactericidal against non-growing P. aeruginosa, reducing bacterial counts by more than four logs at concentrations of 10 μM and 2.5 μM, respectively. In contrast, these drugs did not kill UPEC but only induced PAE (Fig. 3). Solithromycin kills more than four logs of stationary phase P. aeruginosa at a concentration as low as 0.5 μM, similarly to the most bactericidal fluoroquinolones: clinafloxacin, ulifloxacin, sitafloxacin and prulifloxacin. Altogether, 10 compounds (including the above-listed, as well as mitomycin C, besifloxacin, gemifloxacin, and ciprofloxacin) reduce bacterial counts by more than four logs at a concentration of 2.5 µM. In several individual samples, the bacterial count is reduced to undetectable levels: no colonies were observed on agar from the smallest plated dilution, and/or the diluted bacteria did not regrow in liquid medium during the observation period (Dataset 2).
The activity profile of the hit compounds against non-growing S. aureus differed significantly from those against both UPEC and P. aeruginosa (Fig. 4, Fig. S3D). In the regrowth-dilution assay, most fluoroquinolones and macrolides are inactive, exhibit weak activity, or show activity only at the highest concentration tested, 10 µM. While macrolides do not kill non-growing S. aureus, some of the fluoroquinolones reduce bacterial counts by one to two logs, with sitafloxacin showing the most activity. Rifamycins do not kill non-growing S. aureus, but they demonstrate an increased activity in delaying regrowth compared to their effects on the Gram-negative organisms. Together with the disinfectants alexidine and octenidine, the anti-cancer agents mitomycin C and evofosfamide are the most bactericidal compounds in our set, reducing non-growing S. aureus below the limit of detection at a concentration of 10 µM (Fig. 4).
Diverse hit compounds are active against non-growing bacteria at sub-MIC concentrations
The bactericidal effect of antibiotics correlates positively with bacterial growth rate37,54,55,56, implying that slow-growing bacteria are less sensitive to these drugs. Non-growing bacteria are typically tolerant to β-lactams, other cell-wall inhibitors, and aminoglycosides, which did not emerge as hits. In contrast, rapid bacterial growth has been found to reduce macrolide accumulation and efficacy57. To characterize the activity of the hit compounds against growing bacteria, we measured their MIC values and found that some had MIC values much higher than the concentrations needed to kill non-growing bacteria or delay their regrowth (Dataset 1).
The MIC of midecamycin against UPEC in a standard assay (in CA-MHB) is over 160 µM, yet it effectively delays UPEC regrowth at 0.5 µM (Fig. 3). Similarly, solithromycin has a MIC of 80 µM against P. aeruginosa but kills almost four logs of stationary phase cells at 0.5 µM (Fig. 4). Comparing the activity of hit compounds against growing bacteria (MIC) and non-growing bacteria (EC50 for regrowth delay) shows considerable differences between organisms, groups of compounds, and testing conditions (Fig. 5). Anti-cancer agents are inactive based on MIC (EVO, Fig. 5A, B, D; SAT, Fig. 5C) or have an MIC far higher than EC50 (MMC in P. aeruginosa, Fig. 5C). In Gram-negative E. coli and P. aeruginosa, the MIC of macrolides and valnemulin considerably exceeds EC50 in 1:4 CA-MHB medium (Fig. 5A, C). There was no statistically significant correlation between MIC and EC50 for regrowth delay across the entire set of the hit compounds (see Fig. 5 legend for statistical details). For fluoroquinolones, the largest group of compounds, EC50 exceeded MIC manyfold for UPEC in 1:4 CA-MHB pH 7.4, indicating that growing E. coli is more sensitive to these compounds than non-growing cells (Fig. 5A). For P. aeruginosa, however, MIC values are higher than EC50 for all fluoroquinolones, suggesting that non-growing bacteria in this strain are more sensitive to these compounds than growing bacteria, which is unexpected (Fig. 5C).
The activity against growing bacteria was assessed by determining the minimal inhibitory concentration (MIC) using the broth dilution method. The activity against non-growing bacteria was evaluated by calculating the EC50 based on regrowth delay, measured by OD600 readings at 6 h (A, B) or 8 h (C, D) after dilution of treated bacteria into drug-free growth media. EVO evofosfamide, DEG degrasyn, MMC mitomycin C, SOL solithromycin, TYL tylosin, ROS rosamicin, VAL valnemulin. A, C, D 1:4 CA-MHB (pH 7.4) was used for cultivation and treatment of non-growing UPEC CFT073, P. aeruginosa DSM1117, and S. aureus DSM2569. 1:4 CA-MHB (pH 7.4) and CA-MHB (pH 7.4) were used for MIC measurement (Dataset 1). B LPM (pH 5.5) was used in experiments with non-growing E. coli CFT073 and MIC determination (Dataset 1).
Comparing UPEC MIC values at pH 7.4 and 5.5, we found that the anti-cancer agents, which were potentiated against non-growing UPEC in acidic LPM, also have lower MIC in this medium. All rifamycins and three fluoroquinolones (finafloxacin, trovafloxacin, and difloxacin) display lower MIC at pH 5.5 compared to pH 7.4 (Dataset 1). For trovafloxacin and difloxacin, this does not translate into superior activity against non-growing UPEC in acidic medium; however, both drugs are active against non-growing UPEC in both media (Fig. 2).
The standard medium for MIC determination is CA-MHB, which we also initially used to determine the MIC of the hit compounds; however, we cultured and treated the stationary-phase bacteria in a diluted medium with a fourfold reduction in divalent cation concentration. The composition of the testing medium significantly impacts both the MIC values and the bactericidal rates58. To determine if the disparity between high MIC and activity against non-growing cultures was due to different testing media, we measured the MIC of selected compounds in 1:4 CA-MHB pH 7.4. We found that extremely high MICs generally do not decrease in the diluted medium. Exceptions included two rifamycins: rifabutin (in UPEC and P. aeruginosa) and FCE-22250 (in P. aeruginosa), whose MICs drop in the diluted medium. Additionally, the MIC of most fluoroquinolones in P. aeruginosa remain the same in diluted CA-MHB, or even increase, as in the case of trovafloxacin and besifloxacin (four and twofold, respectively; Dataset 1).
We investigated whether the high activity of certain compounds against non-growing bacteria, combined with their lack of activity against growing cells, could be attributed to efflux pump activity. Since efflux pumps are energized and active in growing bacteria, we measured the MIC of these compounds in the presence of the broad-spectrum efflux pump inhibitor phenylalanine-arginine β-naphthylamide (PaβN). Our results showed that PaβN did not reduce the MIC of compounds with the highest MIC values, indicating that efflux pump activity does not account for their elevated MICs (Dataset 1).
Hit compounds display different kinetics of antimicrobial activity against non-growing bacteria
For screening and concentration-dependent characterization of the hit compounds, we used a 24-h incubation to capture their effects, although the actual onset of their activity may occur much sooner. To assess the speed of action, we treated stationary-phase cultures of three organisms with compounds that had previously shown a strong regrowth delay at 10 µM. We selected compounds that, in earlier tests, strongly delayed regrowth, such that diluted cultures remained below an OD600 of 0.12 (indicating no growth) after 6 h for UPEC or 8 h for P. aeruginosa and S. aureus in drug-free medium.
We collected samples at different times during the 24-h incubation, diluted them 2500-fold, and measured the OD600 after 6 or 8 h of further incubation, respectively. As seen in Fig. 6, most of the compounds cause the growth delay after just 1 h incubation in all three organisms. A few compounds act more slowly, such as garenoxacin in E. coli; difloxacin, satraplatin, trovafloxacin, and sparfloxacin in P. aeruginosa. Rifampicin acts quickly against non-growing S. aureus, while the effects of the other compounds increase gradually during incubation but are already apparent within the first hour of treatment.
Bacteria were cultivated in 1:4 CA-MHB (pH 7.4) for 24 h and the compounds were added at a concentration of 10 µM. Samples were taken at the indicated time points, diluted 2500-fold into CA-MHB, and OD600 was measured after 6 h of incubation for UPEC CFT073 and 8 h for P. aeruginosa and S. aureus. The color scale for OD600 values corresponding to each organism is shown below its respective heat map. Gray areas in the heat map indicate compounds not tested due to inactivity observed in previous experiments. Data represent the average of three biological replicates.
In summary, these results indicate that most compounds penetrate non-growing bacteria rapidly, exhibiting an antibacterial effect after one hour of incubation.
Evaluating hit compounds for growth inhibition of intracellular S. flexneri
Nonproliferating bacterial pathogens frequently inhabit intracellular environments, but establishing relevant infection models for high-throughput testing is challenging. Therefore, we firstly tested ability of the hit compounds to cross the eukaryotic cytoplasmic membrane barrier and inhibit growth of S. flexneri within the cytoplasm of the TC7 human colon adenocarcinoma cell line59. To this end, we developed a new, fluorescence-based method that enables real-time monitoring of growth of intracellular Shigella. We used S. flexneri 5a M90T strain producing the AfaE adhesin that enhances bacterial adhesion to epithelial cells and allows synchronization of invasion. The strain was further modified to constitutively express super-folder GFP (sfGFP), which enables monitoring bacterial growth by fluorescence measurement. The epithelial cells were grown to confluence and infected with bacteria at an MOI (multiplicity of infection) of 50. Gentamicin was added to inhibit extracellular bacteria with no effect on intracellular bacteria. Following bacterial adhesion and invasion, the cells were incubated with varying concentrations of the hit compounds and intracellular bacterial growth was tracked by measuring green fluorescence. At concentrations of antibacterials that permit bacterial growth, fluorescence intensity steadily increased over the 14-h incubation period, as exemplified by solithromycin in Fig. 7A. To quantify the effect of the compounds, we calculated the IC50, which represents the concentration at which intracellular bacterial growth was inhibited by 50%. This calculation was based on the endpoint fluorescence intensity values provided in Dataset 3, ranging from baseline (no inhibition, fluorescence intensity similar to the drug-free control) to maximum effect (complete inhibition, with no increase in fluorescence). An example of this analysis is illustrated by the solithromycin inhibition curve in Fig. 7B.
TC7 cells were infected with S. flexneri constitutively expressing sfGFP and treated with various concentrations of the hit compounds. Gentamicin was used to eliminate extracellular bacteria and intracellular bacterial growth was monitored by measuring GFP fluorescence. RFU relative fluorescence units. The symbols for antibiotic classes are shown next to panel (C). A Intracellular growth curves of S. flexneri in the presence of solithromycin at different concentrations as a representative example of a set of growth inhibition curves. Data are presented as means ± SD for n = 3. B Solithromycin inhibition curve. Intracellular growth inhibition was assessed by GFP fluorescence after 14 h treatment. Data are presented as mean ± SD for n = 3. A five-parameter logistic equation was used for asymmetric sigmoidal curve fitting and IC50 determination in GraphPad Prism. For comparison, the MIC obtained by treating extracellular bacteria with the drug is also indicated. C Comparison of MIC and intracellular IC50 values. Error bars represent 95% confidence intervals (CI). D MIC:IC50 ratios with horizontal dashed lines indicating twofold differences.
To evaluate the potentially toxic impact of the hit compounds on mammalian cell viability, we incubated TC7 cells with each drug in the absence of bacteria. At the MIC concentrations, satraplatin, chlorhexidine, alexidine, and valnemulin were toxic to epithelial cells (Fig. S6). Consequently, these compounds were excluded from further analysis. We observed that most compounds inhibited intracellular Shigella, with the exception of bleomycin, which was inactive (Dataset 1). A comparison of intracellular IC50 values with MICs revealed a strong correlation between intracellular and extracellular antibacterial activities (r = 0.79; 95% CI = 0.59–0.89; p < 0.0001) (Fig. 7C). Fluoroquinolones with low MIC values were also among the most effective against intracellular S. flexneri (Fig. 7C). The MIC:IC50 ratios are generally close to one, with the exception of rifamycins, which showed notably higher ratios (Fig. 7D). All rifamycins have MIC values at least 2-fold higher than their IC50 values, with rifabutin exhibiting a an MIC:IC50 > 10. Apart from rifamycins, solithromycin, josamycin, sparfloxacin, and mitomycin C also have an MIC:IC50 ratio >2, indicating enhanced activity against intracellular bacteria. In contrast, ulifloxacin, prulifloxacin, and evofosfamide display a slightly weaker intracellular activity, with MIC:IC50 ratios below 0.5 (Fig. 7D).
In summary, we found that, with a few exceptions, the compounds active against non-growing bacterial cultures also inhibit bacterial growth within the cytoplasm of enterocytes, demonstrating their ability to cross the eukaryotic cytoplasmic membrane barrier.
DNA damage is a possible anti-bacterial mechanism of the anti-cancer compounds
Most of the anti-cancer agents (MMC, BLE, SAT and EVO) that exhibit bactericidal activity against non-growing bacteria are genotoxic, which makes their development into antimicrobials unlikely. The other two drugs of this group, echinomycin (ECH) and plicamycin are DNA-intercalating transcription blockers46. We aimed to evaluate the genotoxicity of ECH and PLI by detecting the possible induction of the SOS response. Degrasyn was excluded from further testing due to its chemical instability.
The SOS response is induced by DNA damage that leads to double-strand breaks and RecA activation. The SOS regulon consists of several operons that are controlled by the LexA repressor, which is degraded in response to RecA activation60. We aimed to quantify SOS induction using the pANO1::cda’ reporter plasmid, which expresses the fluorescent GFPmut3* protein from the SOS-inducible cda promoter61. MMC and GAT, a fluoroquinolone, were used as control compounds. MMC induces DNA interstrand and intrastrand cross-links between adjacent guanine bases62. In bacteria, the induction of SOS regulon proteins is required to repair this damage63. GAT induces DNA damage and SOS as a secondary response to topoisomerase inhibition in bacteria, while it is not genotoxic to eukaryotic cells, which lack type II topoisomerases.
Green fluorescence was induced in response to GAT and MMC in growing cultures of UPEC CFT073 bearing pANO1::cda’. However, as the cultures approached the stationary phase, the drug-free control began to produce GFP as well. After 10 h, the fluorescence normalized to OD600 in the control culture surpassed that of the treated samples (Fig. S7A). Since we aimed to test SOS induction in non-growing cultures, it was essential to use a reporter with no leaky expression in the stationary phase. Therefore, we constructed the plasmid pAED2, based on the low copy-number plasmid pSC101, which contains the cda’ promoter in front of the mScarlet-I-encoding reporter gene. During a 6-h test, this reporter effectively lacked leaky expression and was induced by fluoroquinolones several thousand-fold, thus meeting our requirements (Fig. S7B).
Using pAED2 as a reporter, we tested the SOS response to anti-cancer agents in the medium where these agents exhibited higher antibacterial activity (MMC, BLE, and ECH in 1:4 CA-MHB pH 7.4, PLI, SAT, and EVO in LPM pH 5.5). MMC and SAT, as well as BLE, EVO, and ECH induced the SOS response to different extents when added to the growing UPEC cultures (Fig. 8). Induction of SOS by PLI was not detected (Fig. 8B). In accordance with their high MICs (Dataset 1), 20 μM PLI, EVO, and SAT cause only a slight growth inhibition compared to the effects of MMC, BLE and ECH (Fig. S7C,D). When added to stationary phase cultures, none of the compounds induced SOS (Fig. 8). This might indicate that the stationary phase bacteria are unable to induce a detectable SOS response because of the protein synthesis inhibition and are killed during the treatment. However, another possibility is that the bacteria are poisoned during the stationary phase treatment but are subject to DNA damage and initiate the SOS response only during regrowth after dilution into drug-free medium. This has been demonstrated for fluoroquinolone persisters that required functional SOS regulon for survival but induced a strong SOS response only during recovery, after the ofloxacin removal64,65,66. We tested this possibility and observed no SOS induction despite the characteristic compound-specific regrowth delay (Fig. 8, Fig. S7E, F). At the same time, a control experiment demonstrated SOS induction during recovery of the ofloxacin-treated non-growing UPEC (Fig. 8A), confirming the published finding66.
UPEC CFT073 harboring pAED2 was cultivated in 1:4 CA-MHB (pH 7.4) to assess SOS response induction by echinomycin (ECH), bleomycin (BLE), mitomycin C (MMC), and ofloxacin (OFL) (A), and in LPM (pH 5.5) to evaluate plicamycin (PLI), evofosfamide (EVO), and satraplatin (SAT) (B). The expression of the mScarlet-I reporter, controlled by the SOS-inducible cda’ promoter, was measured in a microplate. Growing cultures were treated with 20 μM of each compound for 6 h, while stationary-phase cultures were treated with 10 μM for 24 h. mScarlet fluorescence and OD600 were recorded at the start (start) and end of the incubation for both drug-free controls (control) and treated samples. Following treatment, stationary-phase bacteria were collected by centrifugation, washed, diluted 1:7 in CA-MHB, and incubated in a microplate. mScarlet fluorescence was recorded at the start of the incubation (start) and when OD600 reached approximately 0.5 for both the drug-free controls (control) and treated samples. Specific fluorescence units (SFU) were calculated by normalizing fluorescence (arbitrary units, AU) to cell density (OD600). Data are presented as means ± SEM for n = 3. Statistical significance was assessed using one-way ANOVA followed by Dunnett’s test, comparing each treatment to the drug-free control. Asterisks indicate p-values: ****p < 0.0001 and *p < 0.05. A single control experiment was performed using OFL.
In summary, we found that in growing bacterial cultures, DNA-intercalating agents either do not induce the SOS response (plicamycin) or induce it to a lesser extent (echinomycin) compared to other anticancer agents. None of the tested compounds induced an SOS response after the removal of the drug and the transfer of bacteria into drug-free growth medium, as observed with fluoroquinolones66.
Discussion
The development of antibiotics specifically targeting non-growing bacteria and chronic bacterial infections has been largely neglected. As a first step to address this gap, we conducted a drug-repurposing screening to identify antimicrobial agents that are primarily effective against quiescent Gram-negative pathogens. Importantly, we focused on compounds that have already undergone or are currently undergoing clinical trials, ensuring that their safety and pharmacokinetic properties are at least partially characterized. We also sought compounds active against Gram-negative pathogens residing in acidified intracellular compartments. This screen led to the identification of several antimicrobials with previously unrecognized potent activity against non-growing bacterial pathogens. While previous screening projects aimed at finding drugs against dormant bacteria have yielded somewhat different results—likely due to technical variations in screening and follow-up assays or differing criteria for prioritizing hit compounds34,38,39,53—our approach offers new candidates that warrant testing against larger panels of clinical isolates.
A previous repurposing screening aimed at identifying bacterial growth inhibitors found that 24% of drugs targeting human cells, spanning all therapeutic classes, inhibited the growth of certain gut bacterial strains67. In contrast, we found that compounds effective against non-growing bacteria in this study were limited to a few antibiotic classes, with only select drugs within these classes demonstrating activity. For instance, among the quinolones included in the library, less than half showed bactericidal activity against non-growing bacteria. Among the 11 macrolides in the SPECS collection, five were active, while six—including widely used erythromycin, clarithromycin, and azithromycin—were not. Among the 14 DNA-alkylating agents, only three—mitomycin C, satraplatin and evofosfamide—exhibited activity against non-growing UPEC, and out of the 19 annotated DNA synthesis inhibitors, only bleomycin demonstrated such activity. The number of disinfectants and antiseptics (14 annotations) in the collection is difficult to determine due to inconsistent classification based on their complementary mechanisms of action (e.g., alexidine dihydrochloride is annotated as a phosphatidylglycerophosphatase inhibitor). Among these, only three biguanides and bisbiguanides with membrane-disrupting activity were active68, while other membrane-targeting compounds, such as the last-resort antibiotic colistin, were not identified as hits. As compounds within the same class target the same biological process, the formation of these two subgroups cannot be attributed to differences in target activity or corruption. We hypothesize that the observed variation is likely attributable to differences in the permeability or uptake of these drugs into non-growing versus growing bacteria, which are influenced by their chemical properties. The hit compounds display diverse chemical and physical characteristics (Table S1, Fig. S8), despite half of them being fluoroquinolones, which are chemically similar to one another. The median hydrophobicity (partition coefficient, XLogP) of the hit compounds is slightly lower than that of the full Prestwick collection (Fig. S8A). In contrast, their median topological polar surface area (TPSA) and molecular complexity are significantly higher than those of the Prestwick collection (Fig. S8B,D), reflecting the inclusion of large molecules such as macrolides, rifamycins and bleomycin. Notably, the polar surface area of 15 hit compounds (over one-third), including the highly active solithromycin and MMC, exceeds 140 Å2—a threshold often associated with reduced membrane permeability69. In summary, the initial analysis of the chemical properties of the candidate compounds does not explain their activity against non-growing bacteria.
We identified several compounds with high MIC values, indicating poor efficacy against growing bacteria, which were nonetheless highly effective against the nongrowing cells of the same strain. For instance, 0.5 µM solithromycin, a macrolide antibiotic of the ketolide sub-class, killed about four logs of stationary phase P. aeruginosa, despite its MIC being 80 μM. The discrepancy, once again, is likely attributable to differences in drug uptake between growing and non-growing bacterial cells. In contrast, telithromycin, another ketolide included in the library, showed no activity. The enhanced uptake of solithromycin into non-growing bacteria may be related to the presence of a fluoride atom, which is absent in telithromycin. Based on its MIC alone, solithromycin would not be considered a viable drug candidate against P. aeruginosa. However, it could be effective when used in combination with another drug that targets proliferating bacteria. In such a combination, solithromycin could be administered at a dose lower than the therapeutic concentration required to exceed the MIC, focusing instead on its activity against non-growing bacterial cells. The identification of solithromycin as a candidate for such synergistic therapy highlights the critical need for specialized testing procedures to uncover antibiotics with activity against persistent infections.
The different bactericidal activity of solithromycin against P. aeruginosa and E. coli may be attributed to variations in their ribosomal structures and, potentially, the slower dissociation of the drug from the P. aeruginosa ribosome. While bacteriostatic and bactericidal macrolides bind to the ribosome with comparable affinity, bactericidal drugs exhibit significantly slower dissociation. This prolonged inhibition of translation can damage bacterial cells, ultimately leading to death70. The slow dissociation of ketolides is attributed to their extended alkyl-aryl side chain, which establishes additional interactions with the ribosome. This side chain acts as a potential pharmacophore, offering opportunities to enhance the bactericidal properties of the drug.
In conclusion, purposefully modifying drugs to improve their penetration into non-growing bacteria and enhance their bactericidal effect could be a promising approach for developing agents against persistent infections. This strategy could enable the development of drugs specifically targeting non-growing bacteria (antiNG-antibiotics) and facilitate their synergistic use with antibiotics targeting actively growing pathogens (antiG-antibiotics, such as beta-lactams) in combination therapies. Notably, antiNG-antibiotics would not aim to achieve the MIC but instead would be administered at a dose sufficient to reach the effective antiNG concentration.
A significant challenge in developing drugs for dormant pathogens is managing toxicity38,53,71. Half of the hits of our screen were fluoroquinolones, which have drawn increasing attention due to their severe adverse effects, and are no longer recommended as first-line antibiotics72. Sitafloxacin and clinafloxacin, which were among the most effective against non-growing bacteria, carry risks due to their extra halogen atoms, which enhance the penetration of lipid membranes but also increase undesirable accumulation in adipose tissue. Moreover, although sitafloxacin is observed to be more potent than ciprofloxacin, its efficacy is significantly reduced in acidic environments, where intravacuolar UPEC persisters are thought to reside. Oral sitafloxacin is currently approved in Japan and Thailand, while clinafloxacin was withdrawn from development due to phototoxicity, a common issue among fluoroquinolones with a halogen at the C-8 position73. Topical application can mitigate the systemic toxicity of fluoroquinolones, as demonstrated by gatifloxacin, which is safely used for eye infections despite its oral form being banned74. To assess an antibiotic’s suitability for the topical treatment of chronic infections, such as chronic wound infections, targeted drug development and specialized testing are necessary.
We successfully employed our new GFP-based method to monitor the intracellular growth of Shigella upon challenge with drugs. All hit compounds, except those that were toxic to TC-7 cells or that could not be tested because of their high extracellular MIC values, were evaluated for their ability to inhibit intracellular Shigella. All but one compound (bleomycin) demonstrated activity, indicating they are able to permeate the cytoplasm of epithelial cells. However, it remains unclear whether rifapentine, solithromycin, and other drugs with higher MIC-to-intracellular IC50 ratios accumulate in the cytoplasm of TC-7 cells, or if intracellularly located S. flexneri is more sensitive to these drugs compared to its sensitivity in TSB broth.
Notably, our screening did not identify any non-antibacterial human drugs with generally new mechanisms of antibacterial activity. The findings included certain anti-cancer compounds with known nonspecific DNA-modifying activity, as well as the DNA-intercalating agents echinomycin and plicamycin, which have the potential to interfere with both transcription and replication. The antibacterial properties of these compounds likely rely on these same mechanisms. MMC is already known for its anti-persister activity75,76,77,78, and, when used in combination therapy, is effective in vivo against multidrug-resistant (MDR) P. aeruginosa79. The antimicrobial activity of DGS was identified through a repurposing screen80 and it is effective against multidrug-resistant S. aureus by modifying several essential cysteines and altering multiple pathways48. Echinomycin is active against S. aureus, including methicillin-resistant strains (MRSA)81.
Testing the extent and timing of bacterial DNA damage induced by these anti-cancer compounds using an SOS reporter provided useful clues but left open questions requiring further investigation. Based on their weak or absent propensity to induce the SOS response in growing UPEC, echinomycin and plicamycin appear to be less genotoxic than other DNA-targeting agents, warranting further exploration for antibacterial use.
Surprisingly, treatment of non-growing bacteria with anti-cancer compounds, including MMC, did not trigger an SOS response during resuscitation, in contrast to the robust SOS induction observed in fluoroquinolone-treated persisters64,65,66. Despite the lack of detectable SOS induction, the bacteria remained capable of (delayed) outgrowth. Resumption of DNA replication and regrowth in these cells is impossible without repairing the inter-strand cross-links caused by MMC, and the uvrABC genes of the SOS regulon are essential for E. coli survival following MMC treatment75. Reduced DNA repair capacity accompanied by increased mutagenesis have been observed as a survival strategy both in certain tumor cells82 and in bacteria, where error-prone mutagenesis is induced in response to antibiotics83,84. These parallels underscore the importance of further investigating the mechanisms underlying damage survival in both tumor cells and recovering bacterial persisters.
In conclusion, the dilution-regrowth screen proved to be an effective tool for identifying compounds with potential activity against persistent Gram-negative infections, highlighting several candidates for further study. We identified 39 compounds active against non-growing bacteria, including 29 previously unrecognized for this activity. These compounds either killed stationary-phase bacteria or delayed their outgrowth without inducing cell death. Notably, some compounds that delayed regrowth in one pathogen exhibited lethality in another, underscoring the potential for species-specific effects. These findings encourage continued research to identify targeted agents for clinically significant chronic infections.
This study has certain limitations that should be considered when interpreting the findings. We found that the assumption that the time to outgrowth measurement correlates with the number of bacteria surviving treatment does not hold due to the post-antibiotic effect (PAE), which can delay outgrowth independently of bacterial killing. This limitation can be addressed using standard colony-forming unit (CFU) counting as an orthogonal assay, although employing colony counting as the primary screening method is labor-intensive.
Only reference strains were used in this study; therefore, the findings need to be validated using panels of clinical isolates of UPEC, P. aeruginosa, S. aureus and S. flexneri. The complexity of the in vivo environment and the uncertainty regarding how well acidic, low-phosphate, and low-magnesium media mimic these natural niches highlight the preliminary nature of the in vitro data. These findings require further validation in vivo.
This study did not aim to investigate the mechanistic basis for the activity of particular agents against non-growing bacteria. Future experiments involving transcriptomic or proteomic analyses will be necessary to identify the molecular targets affected by the compounds tested here.
Methods
Bacterial strains and plasmids
E. coli CFT073, P. aeruginosa DSM1117 (also known as Boston 41501, ATCC 27853), and S. aureus DSM2569 were obtained from DSMZ (Deutsche Sammlung von Mikroorganismen und Zellkulturen GmbH, Braunschweig, Germany). E. coli BW25113 was from Coli Genetic Stock Center (CGSC). pANO1::cda’61 was a gift from Dr. Lars Hestbjerg Hansen. pAED2, a low-copy, ampicillin-resistant (AmpR) plasmid based on the pSC101 backbone, was constructed using circular polymerase extension cloning (CPEC)85 in two steps. First, the trpT terminator region from pSC101-CAM-bioreporter86 was inserted between gfp-mut2 and mScarlet-I genes in pSC101-GFPmut2-mScarlet-I87, resulting in plasmid pAED1. Next, the cda promoter from pANO1::cda’ was inserted upstream of the mScarlet-I gene, resulting in pAED2. Due to difficulties amplifying the ampR gene, the vector was amplified in two fragments. The primers used for cloning are listed in Table S2. S. flexneri 5a M90T contained a chromosomal insertion of constitutively expressed super-folder gfp gene at the attn∷Tn7 site, downstream the glmS gene, and was constructed as detailed previously88,89. S. flexneri M90T expressed the adhesin AFA-I (also known as AfaE90,91) from a plasmid conferring spectinomycin resistance.
Media and growth conditions
Overnight cultures of UPEC, P. aeruginosa and S. aureus were grown in test tubes containing 3 ml of LB broth (~16 h), then diluted 1:100 into either 1:4 diluted CA-MHB medium buffered with 40 mM HEPES (pH 7.4) or, in case of UPEC, into LPM medium25 supplemented with 49 µM MgCl2 and buffered with 30 mM MES (pH 5.5). The cultures were incubated for 24 h in non-baffled Erlenmeyer flasks at 37 °C with shaking at 200 rpm.
Dilution-regrowth screen
The high-throughput screening (HTS) procedure was based on the protocol by Hazan and colleagues15 and conducted at the Chemical Biology Consortium Sweden (CBCS) screening facility. Compounds from the Prestwick Chemical Library (1200 compounds) and the Specs Repurposing Library (5254 compounds) were dispensed using the Echo® (Labcyte) system directly into 384-well plates; 200 nl of 10 mM solution in DMSO was added per well. Each plate included eight wells with 200 nl of 10 mM gatifloxacin, finafloxacin, and kanamycin solutions, along with 8-wells containing 200 nl of DMSO as controls. After 24 h incubation,100 μl of the culture was dispensed into each well of the 384-well plates for screening at a final concentration of 20 μM. The plates were sealed with parafilm and incubated at 37 °C for 24 h in closed humidified boxes, with wet paper towels added to prevent evaporation. After treatment, samples were first diluted 50-fold, using Beckman NXP robot to transfer 2 μl of the sample to 98 μl of phosphate-buffered saline (PBS), followed by a second 50-fold dilution into CA-MHB using the same volumes, resulting in a total 2500-fold dilution. The plates were incubated at 37 °C for 6 h in humidified boxes, then OD600 was measured using a microplate reader. Compounds were considered active if the OD600 < 0.1. Initially, six plates were normalized using the drug-free control, but since this normalization had no effect on the results, it was later omitted.
For hit validation, bacteria were cultivated, and the dilution-regrowth assay was conducted following the same protocol used in the primary screen. Hit compounds were dispensed into 384-well plates using the Echo® (Labcyte) system, with 200, 100, or 50 nl of a 10 mM solution in DMSO added per well, yielding final screening concentrations of 20, 10, and 5 μM, respectively. OD600 values of regrowing samples were normalized to the mean OD600 of the drug-free control. The testing was conducted in two replicates. Compounds were considered active if their OD600 was at least 50% lower than that of the drug-free control at one or more concentrations in both replicates.
For screening assay validation in pilot experiments, bacteria were cultivated as later in the screening assays. Aliquots of 180 μl from the stationary-phase culture were transferred to 96-well plates, and 20 μl of a 200 μM antibiotic solution (gatifloxacin or finafloxacin) in 10% DMSO or 10% DMSO alone for drug-free controls were added. After 24 h treatment, 4 μl of the sample was diluted in 196 μl of PBS, followed by a second dilution of 4 μl into 196 μl of CA-MHB. For assay validation in 384-well plates, 90 μl of the stationary-phase culture was mixed with 10 μl of the 200 μM antibiotic solution or 10% DMSO. After the treatment, 2 μl of the sample was diluted in 98 μl of PBS, followed by a second dilution of 2 μl into 98 μl of CA-MHB. To monitor regrowth, the plates were incubated in a microplate reader (BioTek Synergy Mx) at 37 °C with continuous shaking, and OD600 was recorded every 20 min. For regrowth validation in standing plates, the plates were incubated at 37 °C in humidified boxes, and OD600 was measured after 5, 6, 7, and 8 h. The assays were carried out in triplicates.
Dose–response analysis using the dilution-regrowth assay
For UPEC, dose–response analysis was conducted at the CBCS screening facility. Bacteria were cultivated, and the dilution-regrowth assay was performed according to the HTS protocol. Compounds were dispensed into 384-well plates using the Echo® (Labcyte) system, and regrowth was assessed by measuring OD600 after 6 h of incubation at 37 °C in humidified boxes. Three biological replicates were performed.
For P. aeruginosa and S. aureus, dose–response analysis was conducted in 96-well plates with a 200 μl assay volume, following the procedure used for screening assay validation experiments. Aliquots of the 39 compounds active against non-growing UPEC were obtained from SelleckChem and MedChem Express. Stock solutions were prepared and stored according to the manufacturers’ instructions, then diluted in 10% DMSO before use. Cultures were incubated for 24 h in 1:4 diluted CA-MHB medium under the same conditions used for UPEC cultivation. In preliminary experiments, each compound was tested at a concentration of 20 μM in the dilution-regrowth assay with 4 technical replicates. Regrowth was monitored using a microplate reader at 37 °C with continuous shaking, and OD600 was recorded every 20 min. The time at which OD600 exceeded the threshold of 0.12 was recorded as the Start_Growth-Time. Based on these results, 24 of the most active compounds were selected for further dose–response analysis, which was performed in three biological replicates using the same procedure.
Dose-dependent killing analysis
For survival analysis, bacteria were cultivated as described for the dose–response dilution-regrowth assay. Assays with UPEC were conducted at the CBCS screening facility using 96-well plates with a 200 μl sample volume, and compounds were dispensed using the Echo® (Labcyte) system. P. aeruginosa and S. aureus samples were treated according to the protocol used for the dilution-regrowth experiments. Treated samples were serially diluted 10-fold in PBS, and 10 μl drops were spot-plated onto rectangular LB agar plates using either a Beckman NXP robot (for UPEC) or an Integra VIAFLO96 electronic pipette (for P. aeruginosa and S. aureus). The LB agar plates were incubated overnight at 37 °C and scanned. Colonies were counted at the spots of the lowest dilution where individual colonies could be accurately distinguished. Each colony was manually marked on a separate image layer using the GNU Image Manipulation Program, and counted using NIST’s Integrated Colony Enumerator (NICE 1.4) software92. The experiments were performed in three biological replicates.
Susceptibility testing
Minimal inhibitory concentrations (MICs) were determined using a standard microdilution assay protocol92. CA-MHB medium buffered with 40 mM HEPES (pH 7.4) was used to determine the MICs for UPEC, P. aeruginosa, and S. aureus. For compounds with high MIC values, the measurements were repeated in 1:4 diluted CA-MHB (40 mM HEPES, pH 7.4) and in CA-MHB (40 mM HEPES, pH 7.4) supplemented with 10 μg/ml phenylalanine-arginine β-naphthylamide (PaβN). MICs for UPEC were also determined in LPM buffered with 30 mM MES (pH 5.5). For S. flexneri, MICs were determined in tryptic soy broth (TSB). The assay was performed in triplicates.
SOS response induction analysis
Overnight cultures of CFT073 harboring a reporter plasmid were grown in 3 ml of LB supplemented with 100 µg/ml carbenicillin (Cb), then diluted 1:100 into the medium used for testing. For validation of the pANO1::cda’ reporter, an overnight culture was diluted into CA-MHB (supplemented with 40 mM HEPES, pH 7.4, and 100 µg/ml Cb) and grown to an OD600 ≈ 0.5 at 37 °C with shaking at 200 rpm in an Erlenmeyer flask. Aliquots of 200 μl were dispensed into a 96-well plate and treated with 0.1 and 0.5 μM gatifloxacin, mitomycin C, or left drug-free. Empty wells were filled with water. The plate was incubated in a microplate reader (BioTek Synergy H1) at 37 °C with continuous shaking for 20 h. OD600 and GFPmut3* fluorescence (λex = 485 ± 9 nm, λem = 508 ± 9 nm) were recorded every 10 min.
For pAED2 validation, the overnight culture was diluted into 3 ml of LB supplemented with 100 µg/ml Cb and incubated at 37 °C with shaking at 200 rpm for 1 h. Aliquots of 200 μl were dispensed into a 96-well plate and incubated for 6 h with 0.1 and 0.3 μM gatifloxacin, ofloxacin, or left drug-free. OD600, GFPmut2 fluorescence (λex = 485 ± 9 nm, λem = 508 ± 9 nm), and mScarlet fluorescence (λex = 569 ± 9 nm, λem = 594 ± 9 nm) were measured using a BioTek Synergy H1 microplate reader. The experiment was performed in triplicate.
For analysis of the SOS induction by anti-cancer compounds, the overnight cultures were diluted either into 1:4 diluted CA-MHB (40 mM HEPES, pH 7.4) or LPM (30 mM MES, pH 5.5) that were supplemented with 100 µg/ml Cb. For analysis of the effect on growing bacteria, the cultures were incubated at 37 °C with shaking at 200 rpm in Erlenmeyer flasks for 90 min, to an OD600 ≈ 0.5. Then, 180 μl aliquots were transferred to 96-well plates, and 20 μl of the 200 μM drug solution was added to achieve a final concentration of 20 μM. The plates were incubated in a microplate reader (BioTek Synergy H1) at 37 °C with continuous shaking for 6 h. OD600 and mScarlet fluorescence were recorded throughout the incubation.
For analysis of the effect of anti-cancer compounds on stationary phase- and regrowing bacteria, the cultures were incubated for 24 h at 37 °C with shaking at 200 rpm in Erlenmeyer flasks. For the drug treatment, 475 μl of the culture was mixed with 25 μl of a 200 μM drug solution to achieve a final concentration of 10 μM, which had been demonstrated to be effective against stationary-phase bacteria. The samples were incubated for 24 h at 37 °C in standing 1.5 ml tubes. Before and after the drug treatment, 25 μl aliquots were taken and diluted by mixing with 175 μl PBS. OD600 and mScarlet fluorescence were recorded using a microplate reader (BioTek Synergy H1).
After the treatment, stationary-phase bacteria were harvested by centrifugation at 5000 × g for 5 min at 20 °C, washed twice with PBS, and resuspended in 475 μl PBS. Then, 25 μl aliquots were transferred to 96-well plates, and 175 μl CA-MHB was added. The plates were incubated in a microplate reader at 37 °C with continuous shaking for 14 h. OD600 and mScarlet fluorescence were recorded throughout the incubation. Specific fluorescence was calculated by dividing fluorescence intensity (in relative fluorescence units, RFU) by optical density. The experiments were performed in three biological replicates.
Culture of the TC7 intestinal epithelial cells
TC7 cells (a human cell line derived from Caco-2 colon adenocarcinoma cells59) were grown in Dulbecco’s Modified Eagle Medium (DMEM; Gibco, catalog number 21885-025) supplemented with 10% heat-inactivated serum, 1× amino acid solution prepared from Gibco Minimum Essential Medium Non-Essential Amino Acids (100×) (catalog number 11140-035), and 100 U/ml penicillin–streptomycin (Gibco, catalog number 15140-122). The cells were split using trypsin, seeded in 96-well plates for infection, and grown to confluence, corresponding to approximately 40,000 cells per well.
In vitro infection of cell culture and susceptibility testing of intracellular S. flexneri
A single colony of S. flexneri was inoculated into TSB supplemented with 50 μg/ml spectinomycin and incubated overnight at 37°C with agitation. The overnight culture was diluted 1:200 in fresh TSB, and the bacteria were grown at 37 °C until the OD600 reached 0.3–0.4, corresponding to approximately 2 × 107 CFU/ml. Bacteria were pelleted by centrifugation, washed twice with sterile PBS, and resuspended in infection solution (serum-free DMEM supplemented with 20 mM HEPES, pH 7.4). Just prior to infection, the medium was withdrawn, and the cells were washed twice with sterile PBS. The bacterial inoculum (MOI 50, 2 × 107 CFU/ml) was added to all wells except the no-infection control. The plates were incubated at room temperature for 15 min to allow bacterial adhesion, followed by a 1 h incubation at 37 °C with 5% CO2 to facilitate bacterial invasion.
Twofold serial dilutions of the drugs were prepared in infection solution containing 50 μg/ml gentamicin in a 96-well plate. After the invasion period, the bacterial inoculum was removed, and the serial dilutions of the drugs were added to the wells, except for the no-drug control. The plates were incubated in a Spark multi-mode plate reader (Tecan) at 37 °C with 5% CO2 for 12 h. Green fluorescence from intracellular bacteria was recorded hourly for 15 h at λex = 475 nm and λem = 510 nm, measuring 12 distinct regions of each well. The experiments were performed in triplicates on separate days.
Determination of cellular viability upon drug exposure
TC7 cells were grown to confluence in transparent 96-well cell culture plates (TPP) in the same cell culture medium used for the in vitro infection assay. Just prior to the experiment, the medium was discarded, and the cells were washed twice with sterile PBS to remove any traces of medium or dead cells. A total of 100 μl of infection solution containing MIC concentrations of individual drugs was added to duplicate wells. The plate was incubated at 37 °C in a CO2 incubator for 12 h, under the same conditions as the infection assay.
The 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) assay was performed using the CellTiter 96® AQueous One Solution Cell Proliferation Assay kit (Promega), according to the manufacturer’s instructions. Briefly, 20 μl of CellTiter 96 AQueous One Solution Reagent was added to each well, and the plate was incubated for 2 h at 37 °C in a CO2 incubator. The OD490 of the samples was measured using a Spark multimode plate reader (Tecan). The raw values were normalized to the control wells incubated with infection buffer only. The experiment was performed in duplicate.
For compounds that strongly absorb light at 490 nm (FCE-22250, rifampicin, mitomycin C, rifabutin, rifapentine), a lactate dehydrogenase (LDH) release assay was performed instead of the MTS assay to assess cytotoxicity. The LDH assay was conducted using the CytoTox-ONE Homogeneous Membrane Integrity Assay kit (Promega), according to the manufacturer’s instructions. Briefly, cells in positive control wells were lysed with 10 μl of 10× lysis solution. Then, 50 μl of supernatant from each well was transferred to a black 96-well microplate (Greiner), and 50 μl of CytoTox 96 Reagent was added to each sample. The plate was incubated in the dark for 10 min at room temperature, followed by the addition of 50 μl of Stop Solution. Fluorescence was measured at λex = 560 nm and λem = 590 nm using a Spark multimode plate reader (Tecan). The raw values of the samples were normalized to the average of the total lysis controls, which was set to 100% cell death.
Time-dependent effects of drug treatment
Bacteria were cultivated in 1:4 diluted CA-MHB (40 mM HEPES, pH 7.4) for 24 h. Aliquots were dispensed into a 96-well plate, and compounds were added at a 10 µM concentration. Samples were collected at designated time points, diluted 2500-fold as described for the dilution-regrowth assay, and incubated in standing plates within a humid box at 37 °C. The OD600 of the samples was measured to assess regrowth using a microplate reader (BioTek Synergy H1) after 6 h for UPEC and 8 h for P. aeruginosa and S. aureus. The experiment was performed in triplicates.
Semapimod assay
E. coli CFT073 and BW25113 were grown in 3 ml of LB at 37 °C, shaking at 200 rpm for 16 h. The overnight cultures were then diluted either 1:100 into 40 ml of 1:4 diluted CA-MHB (40 mM HEPES, pH 7.4) or 1:10,000 into 40 ml of 1% LB in PBS and grown in 125 mL Erlenmeyer flasks for 24 h at 37 °C, shaking at 200 rpm. Following this, 1 ml aliquots of each culture were transferred to 1.5 ml test tubes, and semapimod was added at final concentrations of 20 μM and 50 μM. DMSO was added to drug-free controls. To quantify live bacteria before treatment, a sample of each culture was serially 10-fold diluted into PBS, and 10 μL drops were spot-plated onto LB agar. The closed test tubes were incubated for 24 h at 37 °C without shaking.
After treatment, the samples were diluted 2500-fold in two steps: a 50-fold dilution into PBS, followed by a 50-fold dilution into CA-MHB in a 96-well plate with a total volume of 200 μl per well. The 96-well plate was then incubated in a BioTek Synergy H1 plate reader at 37 °C with continuous shaking at medium speed for 22 h with a lid. OD600 was recorded every 20 min. Additionally, the treated samples were diluted 1:200 into LB in another 96-well plate and incubated in a BioTek Synergy Mx plate reader at 37 °C without shaking for 22 h, with OD600 recorded every hour.
To determine the number of live bacteria after the treatment, the bacteria were pelleted, washed twice with PBS, serially diluted, and spot-plated. Plates were incubated and colonies counted as described previously. The experiment was performed in triplicates.
Data analysis
The statistical analysis of all data, as well as EC50 and IC50 determination, was conducted using GraphPad Prism 10.2.3. Statistical significance of the drug effects was assessed using a one-way ANOVA followed by Dunnett’s test, comparing each treatment to the drug-free control. Statistical significance of the differences in chemical characteristics between the hit compounds and the Prestwick library was assessed using a Mann–Whitney test. Statistical significance was set at P ≤ 0.05. A five-parameter logistic equation was used for asymmetric sigmoidal curve fitting and for EC50 and IC50 determination. The number of biological replicates and the meaning of the error bars are provided in the figure legends. The Venn diagram in Fig. 1F was prepared using BioVenn web application62. Characteristics of the chemical and physical properties of Prestwick library compounds were obtained from Supplementary Table S1 from reference67. Characteristics of the hit compounds not included in the Prestwick library were retrieved from the PubChem database93.
Data availability
The dataset supporting the conclusions of this article are included within the article and supplementary information. The plasmid pAED2 generated for this project is available through Addgene (accession number 234599).
References
Lewis, K. The science of antibiotic discovery. Cell 181, 29–45 (2020).
Bumann, D., Fanous, J., Li, J. & Goormaghtigh, F. Antibiotic chemotherapy against heterogeneous pathogen populations in complex host tissues. F1000Research 8, 1–7 (2019).
Balaban, N. Q. et al. Definitions and guidelines for research on antibiotic persistence. Nat. Rev. Microbiol. 17, 441–448 (2019).
Levin-Reisman, I. et al. Antibiotic tolerance facilitates the evolution of resistance. Science 355, 826–830 (2017).
Levin-Reisman, I., Brauner, A., Ronin, I. & Balaban, N. Q. Epistasis between antibiotic tolerance, persistence, and resistance mutations. Proc. Natl Acad. Sci. USA. 116, 14734–14739 (2019).
Lewis, K. Persister cells. Annu. Rev. Microbiol. 64, 357–372 (2010).
van den Bergh, B., Fauvart, M. & Michiels, J. Formation, physiology, ecology, evolution and clinical importance of bacterial persisters. FEMS Microbiol. Rev. 41, 219–251 (2017).
Kaldalu, N. et al. In vitro studies of persister cells. Microbiol. Mol. Biol. Rev. 84, e00070–20 (2020).
Gollan, B., Grabe, G., Michaux, C. & Helaine, S. Bacterial persisters and infection: past, present, and progressing. Annu. Rev. Microbiol. 73, 359–385 (2019).
Fisher, R. A., Gollan, B. & Helaine, S. Persistent bacterial infections and persister cells. Nat. Rev. Microbiol. 15, 453–464 (2017).
Carryn, S. et al. Intracellular pharmacodynamics of antibiotics. Infect. Dis. Clin. North Am. 17, 615–634 (2003).
Monack, D. M., Mueller, A. & Falkow, S. Persistent bacterial infections: the interface of the pathogen and the host immune system. Nat. Rev. Microbiol. 2, 747–765 (2004).
Personnic, N., Doublet, P. & Jarraud, S. Intracellular persister: a stealth agent recalcitrant to antibiotics. Front. Cell. Infect. Microbiol. 13, 1141868 (2023).
Hall, C. W. & Mah, T. F. Molecular mechanisms of biofilm-based antibiotic resistance and tolerance in pathogenic bacteria. FEMS Microbiol. Rev. 41, 276–301 (2017).
Hazan, R., Que, Y. A., Maura, D. & Rahme, L. G. A method for high throughput determination of viable bacteria cell counts in 96-well plates. BMC Microbiol. 12, 1–7 (2012).
Foxman, B., Barlow, R., D’Arcy, H., Gillespie, B. & Sobel, J. D. Urinary tract infection: self-reported incidence and associated costs. Ann. Epidemiol. 10, 509–515 (2000).
Terlizzi, M. E., Gribaudo, G. & Maffei, M. E. UroPathogenic Escherichia coli (UPEC) infections: virulence factors, bladder responses, antibiotic, and non-antibiotic antimicrobial strategies. Front. Microbiol. 8, 1566 (2017).
Karve, S. et al. The impact of initial antibiotic treatment failure: real-world insights in patients with complicated urinary tract infection. J. Infect. 76, 121–131 (2018).
Lawrenson, R. A. & Logie, J. W. Antibiotic failure in the treatment of urinary tract infections in young women. J. Antimicrob. Chemother. 48, 895–901 (2001).
Bokil, N. J. et al. Intramacrophage survival of uropathogenic Escherichia coli: differences between diverse clinical isolates and between mouse and human macrophages. Immunobiology 216, 1164–1171 (2011).
Hannan, T. J. et al. Host-pathogen checkpoints and population bottlenecks in persistent and intracellular uropathogenic Escherichia coli bladder infection. FEMS Microbiol. Rev. 36, 616–648 (2012).
Eto, D. S., Sundsbak, J. L. & Mulvey, M. A. Actin-gated intracellular growth and resurgence of uropathogenic Escherichia coli. Cell. Microbiol. 8, 704–717 (2006).
Gilbert, N. M., O’Brien, V. P. & Lewis, A. L. Transient microbiota exposures activate dormant Escherichia coli infection in the bladder and drive severe outcomes of recurrent disease. PLOS Pathog. 13, e1006238 (2017).
Schreiber, H. L., Spaulding, C. N., Dodson, K. W., Livny, J. & Hultgren, S. J. One size doesn’t fit all:unraveling the diversity of factors and interactions that drive E. coli urovirulence. Ann. Transl. Med. 5, 28 (2017).
Coombes, B. K., Brown, N. F., Valdez, Y., Brumell, J. H. & Finlay, B. B. Expression and secretion of Salmonella pathogenicity island-2 virulence genes in response to acidification exhibit differential requirements of a functional type III secretion apparatus and SsaL. J. Biol. Chem. 279, 49804–49815 (2004).
Høiby, N., Ciofu, O. & Bjarnsholt, T. Pseudomonas aeruginosa biofilms in cystic fibrosis. Future Microbiol. 5, 1663–1674 (2010).
Høiby, N., Bjarnsholt, T., Givskov, M., Molin, S. & Ciofu, O. Antibiotic resistance of bacterial biofilms. Int. J. Antimicrob. Agents 35, 322–332 (2010).
Schnupf, P. & Sansonetti, P. J. Shigella pathogenesis: new insights through advanced methodologies. Microbiol. Spectr. 7, https://doi.org/10.1128/microbiolspec.bai-0023-2019 (2019).
Baker, S. & Scott, T. A. Antimicrobial-resistant Shigella: where do we go next? Nat. Rev. Microbiol. 21, 409–410 (2023).
WHO. WHO Bacterial Priority Pathogens List, 2024: Bacterial pathogens of public health importance to guide research, development and strategies to prevent and control antimicrobial resistance. Bacterial pathogens of public health importance to guide research, development and strategies to prevent and control antimicrobial resistance. 72 (2024).
Welch, R. A. et al. Extensive mosaic structure revealed by the complete genome sequence of uropathogenic Escherichia coli. Proc. Natl. Acad. Sci. USA 99, 17020–17024 (2002).
Luidalepp, H., Jõers, A., Kaldalu, N. & Tenson, T. Age of inoculum strongly influences persister frequency and can mask effects of mutations implicated in altered persistence. J. Bacteriol. 193, 3598–3605 (2011).
Keren, I., Kaldalu, N., Spoering, A., Wang, Y. & Lewis, K. Persister cells and tolerance to antimicrobials. FEMS Microbiol. Lett. 230, 13–18 (2004).
Niu, H. et al. Identification of anti-persister activity against uropathogenic Escherichia coli from a Clinical Drug Library. Antibiotics (Basel, Switzerland) 4, 179–187 (2015).
Dalhoff, A., Stubbings, W. & Schubert, S. Comparative in vitro activities of the novel antibacterial finafloxacin against selected Gram-positive and Gram-negative bacteria tested in Mueller-Hinton broth and synthetic urine. Antimicrob. Agents Chemother. 55, 1814–1818 (2011).
Kerkez, I., Tulkens, P. M., Tenson, T., van Bambeke, F. & Putrinš, M. Uropathogenic Escherichia coli shows antibiotic tolerance and growth heterogeneity in an in vitro model of intracellularinfection. Antimicrob. Agents Chemother. 65, e0146821 (2021).
Eng, R. H. K., Padberg, F. T., Smith, S. M., Tan, E. N. & Cherubin, C. E. Bactericidal effects of antibiotics on slowly growing and nongrowing bacteria. Antimicrob. Agents Chemother. 35, 1824–1828 (1991).
Petersen, M. E. et al. A high-throughput assay identifies molecules with antimicrobial activity against persister cells. J. Med. Microbiol. 73, 001856 (2024).
Niu, H. et al. A clinical drug library screen identifies tosufloxacin as being highly active against Staphylococcus aureus persisters. Antibiotics 4, 329 (2015).
Zimmerli, W. & Sendi, P. Role of rifampin against staphylococcal biofilm infections in vitro, in animal models, and in orthopedic-device-related infections. Antimicrob. Agents Chemother. 63, e01746-18 (2019).
Widmer, A. F., Frei, R., Rajacic, Z. & Zimmerli, W. Correlation between in vivo and in vitro efficacy of antimicrobial agents against foreign body infections. J. Infect. Dis. 162, 96–102 (1990).
Verweij, J. & Pinedo, H. M. Mitomycin C: mechanism of action, usefulness and limitations. Anticancer Drugs 1, 5–13 (1990).
Froudarakis, M. et al. Revisiting bleomycin from pathophysiology to safe clinical use. Crit. Rev. Oncol. Hematol. 87, 90–100 (2013).
Doshi, G., Sonpavde, G. & Sternberg, C. N. Clinical and pharmacokinetic evaluation of satraplatin. Expert Opin. Drug Metab. Toxicol. 8, 103–111 (2012).
Brenner, A. J. et al. Phase 2 trial of hypoxia activated evofosfamide (TH302) for treatment of recurrent bevacizumab-refractory glioblastoma. Sci. Rep. 11, 1–6 (2021).
Portugal, J. Challenging transcription by DNA-binding antitumor drugs. Biochem. Pharmacol. 155, 336–345 (2018).
Kapuria, V. et al. Deubiquitinase inhibition by small-molecule WP1130 triggers aggresome formation and tumor cell apoptosis. Cancer Res. 70, 9265–9276 (2010).
Lee, K. M., Le, P., Sieber, S. A. & Hacker, S. M. Degrasyn exhibits antibiotic activity against multi-resistant Staphylococcus aureus by modifying several essential cysteines. Chem. Commun. (Camb). 56, 2929–2932 (2020).
Srimani, J. K., Huang, S., Lopatkin, A. J. & You, L. Drug detoxification dynamics explain the postantibiotic effect. Mol. Syst. Biol. 13, 948–948 (2017).
Athamna, A., Athamna, M., Medlej, B., Bast, D. J. & Rubinstein, E. In vitro post-antibiotic effect of fluoroquinolones, macrolides, beta-lactams, tetracyclines, vancomycin, clindamycin, linezolid, chloramphenicol, quinupristin/dalfopristin and rifampicin on Bacillus anthracis. J. Antimicrob. Chemother. 53, 609–615 (2004).
Babjuk, M. et al. EAU Guidelines. Edn. presented at the EAU Annual Congress Paris 2024. European Urology vol. 31 https://uroweb.org/guidelines/urological-infections (2022).
Chao, Y.-S. & Farrah, K. Fluoroquinolones for the Treatment of Urinary Tract Infection: A Review of Clinical Effectiveness, Cost-Effectiveness, and Guidelines. (2019).
Zheng, E. J. et al. Discovery of antibiotics that selectively kill metabolically dormant bacteria. Cell Chem. Biol. https://doi.org/10.1016/J.CHEMBIOL.2023.10.026 (2023).
Levin, B. R. & Rozen, D. E. Non-inherited antibiotic resistance. Nat. Rev. Microbiol. 4, 556–562 (2006).
Smirnova, G. V. & Oktyabrsky, O. N. Relationship between Escherichia coli growth rate and bacterial susceptibility to ciprofloxacin. FEMS Microbiol. Lett. 365, fnx254 (2018).
Tuomanen, E., Durack, D. T. & Tomasz, A. Antibiotic tolerance among clinical isolates of bacteria. Antimicrob. Agents Chemother. 30, 521–527 (1986).
Łapińska, U. et al. Fast bacterial growth reduces antibiotic accumulation and efficacy. Elife 11, e74062 (2022).
Mouton, J. W. Soup with or without meatballs: impact of nutritional factors on the MIC, kill-rates and growth-rates. Eur. J. Pharm. Sci. 125, 23–27 (2018).
Chantret, I. et al. Differential expression of sucrase-isomaltase in clones isolated from early and late passages of the cell line caco-2: evidence for glucose-dependent negative regulation. J. Cell Sci. 107, 213–225 (1994).
Maslowska, K. H., Makiela-Dzbenska, K. & Fijalkowska, I. J. The SOS system: a complex and tightly regulated response to DNA damage. Environ. Mol. Mutagen. 60, 368 (2019).
Norman, A., Hansen, L. H. & Sørensen, S. J. Construction of a ColD cda promoter-based SOS-green fluorescent protein whole-cell biosensor with higher sensitivity toward genotoxic compounds than constructs based on recA, umuDC, or sulA promoters. Appl. Environ. Microbiol. 71, 2338–2346 (2005).
Hulsen, T., de Vlieg, J. & Alkema, W. BioVenn—A web application for the comparison and visualization of biological lists using area-proportional Venn diagrams. BMC Genomics 9, 1–6 (2008).
Weng, M. W. et al. Repair of mitomycin C mono- and interstrand cross-linked DNA adducts by UvrABC: a new model. Nucleic Acids Res 38, 6976–6984 (2010).
Goormaghtigh, F. & Van Melderen, L. Single-cell imaging and characterization of Escherichia coli persister cells to ofloxacin in exponential cultures. Sci. Adv. 5, eaav9462 (2019).
Wilmaerts, D., Focant, C., Matthay, P. & Michiels, J. Transcription-coupled DNA repair underlies variation in persister awakening and the emergence of resistance. Cell Rep. 38, 110427 (2022).
Völzing, K. G. & Brynildsen, M. P. Stationary-phase persisters to ofloxacin sustain DNA damage and require repair systems only during recovery. https://doi.org/10.1128/mBio.00731-15 (2015).
Maier, L. et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 555, 623–628 (2018).
Mcdonnell, G. & Russell, A. D. Antiseptics and disinfectants: activity, action, and resistance. Clin. Microbiol. Rev. 12, 147–179 (1999).
Pajouhesh, H. & Lenz, G. R. Medicinal chemical properties of successful central nervous system drugs. NeuroRx 2, 541 (2005).
Svetlov, M. S., Vázquez-Laslop, N. & Mankin, A. S. Kinetics of drug-ribosome interactions defines the cidality of macrolide antibiotics. Proc. Natl Acad. Sci. USA 114, 13673–13678 (2017).
Hurdle, J. G., O’Neill, A. J., Chopra, I. & Lee, R. E. Targeting bacterial membrane function: an underexploited mechanism for treating persistent infections. Nat. Rev. Microbiol. 9, 62–75 (2011).
Rusu, A., Munteanu, A. C., Arbănași, E. M. & Uivarosi, V. Overview of side-effects of antibacterial fluoroquinolones: new drugs versus old drugs, a step forward in the safety profile? Pharmaceutics 15, 804 (2023).
Ball, P. Adverse drug reactions: implications for the development of fluoroquinolones. J. Antimicrob. Chemother. 51(Suppl 1), 21–27 (2003).
Schultz, C. Gatifloxacin ophthalmic solution for treatment of bacterial conjunctivitis: safety, efficacy and patient perspective. Ophthalmol. Eye Dis. 4, OED.S7383 (2012).
Kwan, B. W., Chowdhury, N. & Wood, T. K. Combatting bacterial infections by killing persister cells with mitomycin C. Environ. Microbiol. 17, 4406–4414 (2015).
Cruz-Muñiz, M. Y. et al. Repurposing the anticancer drug mitomycin C for the treatment of persistent Acinetobacter baumannii infections. Int. J. Antimicrob. Agents 49, 88–92 (2017).
Carocci, A. et al. Mitomycin C as an anti-persister strategy against Klebsiella pneumoniae: toxicity and synergy studies. Antibiotics 13, 815 (2024).
Pacios, O. et al. Enhanced antibacterial activity of repurposed mitomycin C and imipenem incombination with the lytic phage vB_KpnMVAC13 against clinical isolates of Klebsiella pneumoniae. Antimicrob. Agents Chemother. 65, e0090021 (2021).
Svedholm, E., Bruce, B., Parcell, B. J. & Coote, P. J. Repurposing mitomycin C in combination with pentamidine or gentamicin to treat infections with multi-drug-resistant (MDR) Pseudomonas aeruginosa. Antibiotics (Basel, Switzerland) 13, 177 (2024).
Le, P. et al. Repurposing human kinase inhibitors to create an antibiotic active against drug-resistant Staphylococcus aureus, persisters and biofilms. Nat. Chem. 12, 145–158 (2020).
Park, Y. S., Shin, W. S. & Kim, S. K. In vitro and in vivo activities of echinomycin against clinical isolates of Staphylococcus aureus. J. Antimicrob. Chemother. 61, 163–168 (2008).
Russo, M. et al. Adaptive mutability of colorectal cancers in response to targeted therapies. Science 366, 1473–1480 (2019).
Galhardo, R. S., Hastings, P. J. & Rosenberg, S. M. Mutation as a stress response and the regulation of evolvability. Crit. Rev. Biochem. Mol. Biol. 42, 399–435 (2007).
Gutierrez, A. et al. β-lactam antibiotics promote bacterial mutagenesis via an RpoS-mediated reduction in replication fidelity. Nat. Commun. 4, 1–9 (2013).
Quan, J. & Tian, J. Circular polymerase extension cloning. Methods Mol. Biol. 1116, 103–117 (2014).
Preem, L. et al. Monitoring of antimicrobial drug chloramphenicol release from electrospun nano- and microfiber mats using UV imaging and bacterial bioreporters. Pharmaceutics 11, 487 (2019).
Hinnu, M., Putrinš, M., Kogermann, K., Kaldalu, N. & Tenson, T. Fluorescent reporters give new insights into antibiotics-induced nonsense and frameshift mistranslation. Sci. Rep. 14, 6883 (2024).
Tadala, L. et al. Infection-induced membrane ruffling initiates danger and immune signaling via the mechanosensor PIEZO1. Cell Rep 40, 111173 (2022).
Sharma, A., Omer Aden, R., Puhar, A. & Cisneros, D. A. CRISPR-Cas-guided mutagenesis of chromosome and virulence plasmid in Shigella flexneri by cytosine base editing. mSystems 8, e0104522 (2023).
Clerc, P. & Sansonetti, P. J. Entry of Shigella flexneri into HeLa cells: evidence for directed phagocytosis involving actin polymerization and myosin accumulation. Infect. Immun. 55, 2681 (1987).
Labigne-Roussel, A. F., Lark, D., Schoolnik, G. & Falkow, S. Cloning and expression of an afimbrial adhesin (AFA-I) responsible for P blood group-independent, mannose-resistant hemagglutination from a pyelonephritic Escherichia coli strain. Infect. Immun. 46, 251–259 (1984).
Clarke, M. L. et al. Low-cost, high-throughput, automated counting of bacterial colonies. Cytometry Part A 77, 790–797 (2010).
Kim, S. et al. PubChem 2023 update. Nucleic Acids Res. 51, D1373–D1380 (2023).
Acknowledgements
We thank Jelena Kiprovskaja for excellent technical assistance.
Funding
Open access funding provided by Lund University.
Author information
Authors and Affiliations
Contributions
N.K., T.T., V.H. and A.P. conceived the project. N.K. and S.B.F. performed the screening and analyzed the data. N.B., S.B.F., and N.K. performed the follow-up characterization of antimicrobials. A.S. and A.P. conceived and performed the Shigella and mammalian cell toxicity testing. N. Ch. A. performed the SOS response testing. J.A. and M.H. constructed the SOS reporter plasmid. N.K. wrote the main manuscript, N.K., N.B. and N. Ch.A. prepared the figures. All authors reviewed the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaldalu, N., Bērziņš, N., Berglund Fick, S. et al. Antibacterial compounds against non-growing and intracellular bacteria. npj Antimicrob Resist 3, 25 (2025). https://doi.org/10.1038/s44259-025-00097-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44259-025-00097-0