Abstract
Patients with colour vision deficiency (CVD) may not see blood in urine or stool, often the first sign of bladder or colorectal cancer, respectively. Here we sought to identify whether patients with bladder or colorectal cancer and CVD have worse outcomes when compared to matched patients without CVD, using an electronic health records research network (TriNetX). A total of 135 patients with CVD and bladder cancer showed shorter overall survival (χ2 = 4.85, P = 0.028) as compared to 135 matched patients without CVD. There was no significant difference among 187 patients with colorectal cancer and CVD, and controls. This suggests that patients with bladder cancer and CVD may be at risk of reduced survival. This is a hypothesis-generating paper that should raise clinicians’ diagnostic suspicion for bladder cancer in patients with CVD and prompt further investigation into whether screening for bladder cancer should be introduced for high-risk individuals with CVD.
Similar content being viewed by others
Main
Colorectal cancer and urinary bladder cancer are among the most common malignancies in the United States. Colorectal cancer is the third most common cancer in the United States among men and women, and bladder cancer is the fourth most common among men1. Colorectal cancer has the third-highest and fourth-highest mortality among malignancies observed in men and women, respectively, while bladder cancer has the eighth-highest among men.
Blood in the stool or urine is often the first sign of colorectal2,3,4 or bladder cancer5, respectively. Recognizing this sign is an essential indicator for patients to seek medical evaluation. However, patients with visual impairments that prevent them from identifying the red colour of blood in their faeces or urine may be at greater risk of delayed detection of disease. This is especially true in the case of painless haematuria, which is often the sentinel sign of bladder cancer, where blood in the urine is not accompanied by pain, which may otherwise be an alternative symptom prompting patients to seek medical attention. Without pain as an additional symptom, patients can rely solely on recognizing blood in their urine to detect the disease.
One visual condition that may limit a patient’s ability to detect blood in the stool or urine is colour vision deficiency (CVD), one of the most common inherited disorders of vision, affecting 1 in 12 (8%) males and 1 in 200 (0.5%) females6. The majority of CVDs impair the ability to distinguish the colour red7, leading to the possibility of delayed recognition of malignancy and an increased risk of severe disease among patients with CVD and colorectal cancer or bladder cancer.
Indeed, two case reports show that this has been observed among patients with CVD. One report8 discussed three patients with CVD who were experiencing blood in their stool, but misinterpreted the blood as diarrhoea due to an inability to discriminate the colour red. It was not until their respective spouses noticed blood in the toilet that they sought care. They each delayed seeking care by a few weeks to 3 months from the onset of supposed ‘diarrhoea’. Another report9 likewise described a patient with CVD who was in shock due to gastrointestinal haemorrhage, and still did not present for 10 days following the first observation of presumed ‘diarrhoea’, at which point he was hypotensive, tachycardic and diaphoretic, and admitted to the intensive care unit.
Prior work10 showed this phenomenon in an experimental setting by conducting a study in which 10 participants with CVD and 20 age-matched controls were shown photographs of saliva, urine and stool, and asked to identify which of them contained blood. The colourblind group was substantially less successful at selecting the photos depicting bloody human excreta (a median of 77% correctly identified images versus 99% in the control group).
In a subsequent study, 200 male patients with bladder cancer were evaluated for CVD using the Ishihara plate test, and the authors found that bladder cancer patients with CVD presented with more invasive disease (rated T1 or above) as compared to peers without CVD, who mostly presented with superficial cancer (Ta or Tis)11.
Thus, there is evidence to suggest that patients with CVD and cancers that initially present with blood in urine or stool may delay care-seeking due to lack of recognition of the blood. This delay is thought to allow the cancer to invade more tissue, leading to more advanced cancer histology at the time of presentation. However, it remains an open question whether this translates to differential mortality among patients with CVD as compared to patients without CVD. We are not familiar with any studies to date that have evaluated the survival or mortality outcomes associated with colorectal or bladder cancer in patients with CVD, as compared to patients without CVD.
One study10 showed that only 10% of surveyed physicians had considered the possibility that colourblindness may preclude patients from screening for blood in their own urine and faeces, suggesting that bladder or colorectal cancer diagnoses might be made later in visually impaired patients than in patients without visual impairment.
Identifying the risks this may pose to survival and mortality further clarifies the importance of more attentively screening these populations for certain malignancies, and may serve to increase clinicians’ suspicion of cancer among patients with CVD and signs suggesting illness.
Results
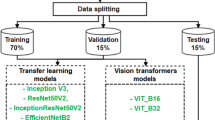
The TriNetX network provides real-world electronic health records data from health organizations in the United States and around the world. TriNetX was used to form cohorts of patients based on their diagnoses of bladder cancer, colorectal cancer and CVD (or the absence thereof), which were then used in retrospective cohort analyses to evaluate survival differences between the cohorts with CVD and those without CVD.
Bladder cancer
A total of 149 patients in the bladder cancer with CVD cohort and 371,154 patients in the bladder cancer without CVD control cohort were initially identified before propensity score matching (PSM). After PSM methods and inclusion–exclusion criteria were applied, 135 patients were subsequently analysed in each cohort.
The average age of patients after PSM at the time of initial diagnosis of bladder cancer with and without CVD was 71.9 ± 10.8 years and 70.6 ± 13.7 years, respectively. Females comprised 7.4% of the CVD cohort and 7.4% of the non-CVD cohort. Before PSM, there were significant differences between the groups in the 0–45 age at cancer diagnosis bracket (P = 0.0047), sex (P < 0.0001) and race (P < 0.0001 for white, unknown race and unknown ethnicity populations; P = 0.0002 for Hispanic or Latino populations). The mean follow-up time of patients in the bladder cancer with CVD cohort and bladder cancer without CVD cohort, respectively, was 1,848 (s.d. = 1,517) days and 1,631 (s.d. = 1,504) days.
Furthermore, there were significant differences between the groups in systemic comorbidities, including nicotine dependence (P < 0.0001), hypertension (P < 0.0001), diabetes mellitus (P < 0.0003) and hyperlipidaemia (P < 0.0001). After PSM methods were applied for the above features, baseline characteristics were balanced between the groups and there were no significant differences in age, age at cancer diagnosis, sex, race or ethnicity, nor in systemic comorbidities including nicotine dependence, hypertension, diabetes mellitus and hyperlipidaemia (Table 1).
Figure 1 shows the results of a Kaplan–Meier survival analysis of mortality in the two groups. A log-rank analysis revealed that the cohort with both bladder cancer and CVD had a lower survival probability than the cohort with bladder cancer and no CVD (χ2 = 4.85, P = 0.028).
After observing a difference in overall survival, a 20-year mortality analysis was conducted separately to quantify the differential mortality risk. Given that the TriNetX platform is live, the data are newly pulled with each analysis, leading to slight variability in the numbers. As such, in this subsequent analysis, a total of 149 patients in the bladder cancer with CVD cohort and 365,420 patients in the bladder cancer without CVD control cohort were initially identified before PSM. After PSM methods and inclusion–exclusion criteria were applied, 136 patients were subsequently analysed in each cohort.
The demographic trends in the secondary mortality analysis were similar to those in the original cohorts; more details are provided in Table 2. Some key differences included mean age at cancer diagnosis (CVD cohort, 71.6 ± 11.2 years; without CVD, 71.3 ± 11.8 years) and mean follow-up time (CVD cohort, 1,847 (s.d. = 1,512) days; without CVD, 1,556 (s.d. = 1,413) days).
The cohort with CVD experienced a 52% higher 20-year mortality rate than the non-CVD cohort (risk ratio = 1.52, 95% confidence intervals (CI) = 1.05–2.19, P = 0.025).
Colorectal cancer
A total of 216 patients in the colorectal cancer with CVD cohort and 757,629 patients in the colorectal cancer without CVD control cohort were initially identified before PSM. After PSM methods and inclusion–exclusion criteria were applied, 187 patients were subsequently analysed in each cohort.
The average age of patients after PSM at the time of initial diagnosis of colorectal cancer with and without CVD was 65.2 ± 15 years and 66.7 ± 14.9 years, respectively. Females comprised 29.9% in both cohorts. Before PSM, there were significant differences between the groups in the 45–60 age at index bracket (P = 0.02), sex (P < 0.0001), race (P < 0.0001 for white, unknown race and unknown ethnicity populations). Likewise, before PSM balancing of the constituent diagnoses of colorectal cancer (that is, C18, C19 and C20), there was a significant difference between the cohorts in the diagnosis of International Classification of Diseases, Tenth Revision (ICD-10) colon cancer (C18; P = 0.0035), International Classification of Diseases for Oncology (ICD-O) colon cancer (C18; P = 0.0022), ICD-O rectosigmoid junction cancer (C19; P < 0.0001) and ICD-O rectal cancer (P = 0.0353). The mean follow-up time of patients in the colorectal cancer with CVD cohort and colorectal cancer without CVD cohort, respectively, was 1,862 (s.d. = 1,605) days and 1,352 (s.d. = 1450) days.
Furthermore, there were significant differences between the groups in systemic comorbidities, including nicotine dependence (P < 0.0001), hypertension (P < 0.0001), diabetes mellitus (P < 0.0001) and hyperlipidaemia (P < 0.0001). After PSM methods were applied for the above features, baseline characteristics were balanced between the groups and there were no significant differences in age, age at index, sex, race, ethnicity or diagnoses of ICD-10 and ICD-O colon cancer, rectosigmoid junction cancer and rectal cancer, nor in systemic comorbidities including nicotine dependence, hypertension, diabetes mellitus and hyperlipidaemia (Table 3).
Figure 2 shows the results of a Kaplan–Meier survival analysis of mortality in the two groups. A log-rank analysis revealed that the cohorts did not significantly differ in survival probability (χ2 = 0.285, P = 0.593). As such, a 20-year mortality analysis was not conducted.
Discussion
This retrospective study compared outcomes of patients with colorectal or bladder cancer and CVD to matched patients with colorectal or bladder cancer without CVD. The analysis revealed that the bladder cancer and CVD group had a reduced survival probability and higher 20-year mortality risk than the non-CVD group with bladder cancer. There was no significant difference in mortality due to colorectal cancer between the two cohorts.
There is limited literature on the outcomes in patients with colorectal or bladder cancer and CVD. Case reports8,9 show that patients with CVD may delay seeking care by weeks to months because they are unable to discriminate blood in their waste, and only do so when their spouses notice blood in the toilet bowl. Furthermore, prior work11 has shown that patients with CVD and bladder cancer present with more advanced findings on histology as compared to patients without CVD. The existing literature is thus beginning to coalesce around the hypothesis of this study, namely that patients with CVD are more likely to delay seeking care for cancers with blood in urine or stool as a presenting symptom, leading to more invasive disease on initial presentation. The extension of this phenomenon is an expectation that patients with CVD experience increased mortality as a result of their more invasive disease on presentation; however, no evidence has been presented in the literature so far to support this. The findings presented herein lend credence to this hypothesis.
This analysis identified a significant difference in mortality between patients with bladder cancer and CVD and those without CVD. Interestingly, there was no significant mortality difference between patients with colorectal cancer and CVD and those without CVD. This may be due to a variety of factors. For one, whereas bladder cancer tends to present with painless haematuria (meaning, the only sign of disease is blood in the urine), colorectal cancer can often present with a multitude of other symptoms that may indicate disease even in a patient who cannot see blood in the stool. A study of early-onset colorectal cancer found that 63% of patients under the age of 45 years presented with abdominal pain, 54% with a change in stool habits, 53% with rectal bleeding and 32% with weight loss, and found similar findings among patients over the age of 45 years12. In contrast, 80–90% of patients with bladder cancer present with painless gross haematuria13, while only approximately 20% present with irritative voiding symptoms, including dysuria, urgency, frequency or urge incontinence14.
Screening is another factor that may explain why a difference was observed in mortality among the patients with bladder cancer, while there was no significant difference among the patients with colorectal cancer. Whereas the United States Preventive Services Task Force recommends screening for colorectal cancer in all adults aged 45 years and older15, there is no such recommendation for asymptomatic bladder cancer screening16. As such, it stands to reason that, even if a patient with CVD and colorectal cancer does not visually detect blood in the stool, many will still be captured by standard screening.
These two factors lend further support to the hypothesis that patients with CVD do not notice blood in their waste and therefore present later and with more advanced disease. Specifically, because bladder cancer tends to present only with painless haematuria, the onus of disease detection is placed almost entirely on the patient observing blood in the urine, whereas colorectal cancer might be observed through other symptoms, or might be caught by routine screening, thereby interrupting the chain of events leading from CVD to impaired recognition of blood, and thereby to more advanced disease.
It is also possible that there is, in fact, a mortality difference between colorectal cancer patients with and without CVD, but that it is smaller in effect size than what is seen in bladder cancer, for the aforementioned reasons. It may be the case that this analysis was underpowered to detect a smaller difference in mortality between patients with both colorectal cancer and CVD, and those without CVD.
Limitations within this study are inherent in the analysis of large sets of de-identified aggregated medical health records data. This study relies on accurate ICD-10 and ICD-O diagnoses and coding, and, as such, may contain inaccuracies in the true coding of the diagnoses evaluated in the analysis. It is also possible that many patients with colourblindness may not have their condition officially diagnosed and coded in their medical records, as it can often present mildly and may not cause significant enough impairment to be noticeable. Indeed, research from around the world indicates that a significant percentage of individuals with colourblindness are undiagnosed. In the United Kingdom, 80% of colourblind students remain undiagnosed by the time they enter year seven of school17. A study of 283 individuals with CVD in Latvia found that 55% of participants had learned of their colourblindness in adulthood, mostly in an occupational context18.
In the United States, colour vision screening is not typical. Only 11 states require it for school-aged children19 and only 1 state (Massachusetts) requires colour vision testing for all drivers obtaining a licence (13 require it for a commercial driver’s licence to operate large or heavy vehicles)20. As such, given how prevalent CVD is (1 in 12 males and 1 in 200 females), there is a high likelihood that the number of patients officially diagnosed with CVD is smaller than the number of patients who have CVD, whether or not they may be diagnosed. This may have led to misclassification bias, in which the effect size would be diluted because patients with undiagnosed CVD may have been included in the cohort without CVD. So, the effect size may be larger in reality than the analysis calculated.
If, as was suggested earlier, there was in fact a mortality difference among colorectal cancer patients that this study was underpowered to detect, perhaps this fact may have also contributed to suppressing the effect size and concealing that difference. This is both because of possible misclassification bias and because fewer patients officially diagnosed with CVD led to a smaller cohort size and reduced statistical power.
A possible further limitation was the 1:1 ratio used for PSM. While including a larger cohort of matched controls (for example, 2:1, 5:1 or 10:1) would have strengthened the control arm, the TriNetX system does not currently allow for these alternative matching ratios. At the same time, there is also evidence to suggest that a 1:1 or 2:1 ratio is optimal in PSM21.
A limitation also arose in implementing our fixed-sequence analysis because each subsequent analysis run in TriNetX is performed separately. This is an intrinsic element of the system, designed to protect patient privacy by summoning patient data only when the analysis is run. Because we do not have access to the raw patient records, we can only interface with the data through the TriNetX system. And, because it summons data from participating healthcare organizations in real time, there is a slight variability in the number of records drawn in each instance, which is why our survival analysis among the bladder cancer patients included 135 participants in each cohort, whereas our 20-year mortality analysis included 136 patients.
Another limitation was the low level of staging data associated with patients in the cohort. While incorporating staging data into our analysis would have offered a clearer window into the biological underpinnings of our findings (for instance, that patients with CVD also presented with more advanced stages of cancer, in addition to being at higher risk of mortality), we were unable to include this additional element of analysis because not all healthcare organizations contribute staging data to the TriNetX system, resulting in low levels of staging data within our cohorts. The staging data that were available were small in quantity and, therefore, suppressed by the system to protect privacy. However, as mentioned previously, the existing literature8,9,11 offers support for the mechanism we propose, namely that patients with CVD seek care later and thus present with more advanced cancer, placing them at higher risk of mortality.
Although we acknowledge these limitations, without the use of this system, it would have been challenging to access such a large dataset of real-world patient records and identify patients with overlapping diagnoses of CVD and bladder or colorectal cancer. Future work can use dedicated datasets and include larger cohorts to assess survival differences more systematically.
Overall, this study uses secondary data to demonstrate an increased risk of mortality among patients with bladder cancer who also have CVD, compared to patients with bladder cancer and no CVD, in a large real-world live patient dataset. While these hypothesis-generating findings should increase clinicians’ suspicion of bladder cancer among patients with CVD and nonspecific signs of malignancy (for example, weight loss and fatigue), the results should be further validated in future work to assess whether formal changes to clinical practice would be merited, such as screening patients with CVD who are at high risk for bladder cancer. Future studies may use a prospective design to test for CVD among patients with colorectal or bladder cancer as a means of increasing the sample size and factor staging into the analysis. This will help to corroborate the results of this study and also verify whether there is, in fact, no difference in mortality between patients with colorectal cancer and CVD and those without CVD. Future studies may also evaluate whether screening populations with CVD for bladder cancer can lead to improved survival. Moreover, future work should risk-stratify the various subtypes of CVD to identify whether some pose a greater mortality risk than others.
Methods
Portions of the Methods are adapted from our prior publications that also used the TriNetX network22,23.
The TriNetX platform (Cambridge) was used to conduct a retrospective cohort study. TriNetX is a research network that aggregates de-identified electronic health records from several major health organizations within the United States of America and countries across the globe. Over 275 million patient records are available on the platform. TriNetX is certified to the ISO 27001:2013 standard and complies with the Health Insurance Portability and Accountability Act. TriNetX data are only accessible in de-identified aggregate form. Given that the analysis described herein exclusively made use of de-identified records, the study was deemed exempt from Institutional Review Board approval.
The data used in this study were collected on 8 March 2025 and 11 March 2025 from the TriNetX Health Research Network, which provided access to electronic medical records. This study used a retrospective cohort design by reviewing electronic medical records included in the TriNetX research network database from January 2004 through March 2025.
Statistics and reproducibility
Patients with bladder cancer were identified by ICD-10 and ICD-O code C67 (malignant neoplasm of bladder). Patients with colorectal cancer were identified by ICD-10 and ICD-O codes C18 (malignant neoplasm of colon), C19 (malignant neoplasm of rectosigmoid junction) or C20 (malignant neoplasm of rectum). Both ICD-10 and ICD-O codes were included because not all healthcare organizations use the ICD-O classification. These populations were then narrowed to those with an additional diagnosis of CVD, as identified by the ICD-10 code H53.5 (CVDs). Univariate analyses were performed and odds ratios with 95% CI were calculated for systemic associations.
After this, the control population was formed, comprising patients with colorectal or bladder cancer without CVD. Patients in the bladder cancer control cohort were included based on the presence of ICD-10 and ICD-O code C67. Patients in the colorectal cancer control cohort were included based on the presence of ICD-10 and ICD-O code C18, C19 or C20. Individuals in these control groups were excluded if they had been diagnosed with CVDs, identified by ICD-10 code H53.5.
Demographics at baseline were noted, including sex, race, ethnicity and age at cancer diagnosis. Sex, race and ethnicity were recorded according to their designation within the electronic health record. Additionally, diagnoses of hypertension (I10), diabetes mellitus (E08-E13), hyperlipidaemia (E78.5) and nicotine dependence (F17) were queried and recorded for both groups.
Subsequently, PSM was performed on the bladder cancer with CVD and bladder cancer without CVD cohorts to control for age, age at cancer diagnosis, sex, race, ethnicity and systemic comorbidities including nicotine dependence, hypertension, diabetes mellitus and hyperlipidaemia. The same was done for the colorectal cancer with CVD and colorectal cancer without CVD cohorts. The PSM was performed using the TriNetX built-in analysis platform (1:1 matching by nearest-neighbour greedy matching algorithm with a caliper of 0.25 s.d.)24. Age at cancer diagnosis was matched by the number of participants in several age brackets (below 45, 45–59, 60–74, 75 years and above). The age of 45 years was selected as the initial threshold because the United States Preventive Services Task Force recommends screening colonoscopies at this age15. In the colorectal cancer cohorts, the proportion of each colorectal tract cancer ICD code diagnosis (C18, C19 and C20) was balanced between the two cohorts. The primary outcomes included survival probability, as measured by a Kaplan–Meier survival analysis, and a 20-year mortality risk. The survival analysis was conducted first, and, if a significant difference was observed, a 20-year mortality risk analysis was conducted subsequently. This is in keeping with the ‘fixed-sequence’ method of avoiding multiple comparisons. Because the bladder cancer and colorectal cancer analyses address different hypotheses, it was determined that further correction for multiple comparisons was not merited. Significance tests were two-sided and paired. A threshold of 0.05 was used to determine significant P values and 95% CIs were calculated as well.
Ethical statement
This analysis exclusively made use of de-identified, aggregate records. As such, the study was deemed exempt from institutional review board approval.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The data used in this analysis originate from the TriNetX platform, which deidentifies and aggregates data to protect patient privacy. As such, data at the individual level cannot be shared. Aggregated results produced by the TriNetX platform have been shared in the results of this paper. Data that were accessible to the authors can be made available within 1 month on reasonable request to E.R. (rahimye@stanford.edu), Byers Eye Institute, Department of Ophthalmology, Stanford University School of Medicine.
Code availability
Not applicable, as the analysis was conducted using built-in tools within the TriNetX system.
References
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 74, 12–49 (2024).
Demb, J. et al. Red flag signs and symptoms for patients with early-onset colorectal cancer: a systematic review and meta-analysis. JAMA Netw. Open 7, e2413157 (2024).
Olde Bekkink, M. et al. Diagnostic accuracy systematic review of rectal bleeding in combination with other symptoms, signs and tests in relation to colorectal cancer. Br. J. Cancer 102, 48–58 (2010).
Hamilton, W., Round, A., Sharp, D. & Peters, T. J. Clinical features of colorectal cancer before diagnosis: a population-based case-control study. Br. J. Cancer 93, 399–405 (2005).
DeGeorge, K. C., Holt, H. R. & Hodges, S. C. Bladder cancer: diagnosis and treatment. Am. Fam. Physician 96, 507–514 (2017).
Simunovic, M. P. Colour vision deficiency. Eye 24, 747–755 (2010).
Kolb, H., Fernandez, E., Jones, B. & Nelson, R. (eds) Webvision: The Organization of the Retina and Visual System (University of Utah Health Sciences Center, 1995).
Stiff, G. J., Haray, P. N. & Foster, M. E. Dyschromatopsia (number 97) and rectal bleeding. BMJ 313, 594 (1996).
Mahpour, N. & Hou, L. S2102 color vision deficiency and gastrointestinal hemorrhage: a synergistically lethal combination. Am. J. Gastroenterol. 115, S1107–S1108 (2020).
Reiss, M. J., Labowitz, D. A., Forman, S. & Wormser, G. P. Impact of color blindness on recognition of blood in body fluids. Arch. Intern. Med. 161, 461–465 (2001).
Katmawi-Sabbagh, S., Haq, A., Jain, S., Subhas, G. & Turnham, H. Impact of colour blindness on recognition of haematuria in bladder cancer patients. Urol. Int. 83, 289–290 (2009).
Skalitzky, M. K. et al. Characteristics and symptomatology of colorectal cancer in the young. Surgery 173, 1137–1143 (2023).
Willis, G. C. & Tewelde, S. Z. The approach to the patient with hematuria. Emerg. Med. Clin. North Am. 37, 755–769 (2019).
Jakus, D., Šolić, I., Jurić, I., Borovac, J. A. & Šitum, M. The impact of the initial clinical presentation of bladder cancer on histopathological and morphological tumor characteristics. J. Clin. Med. 12, 4259 (2023).
US Preventive Services Task Force, Davidson, K. W. et al. Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA 325, 1965–1977 (2021).
Moyer, V. A. & U.S. Preventive Services Task Force. Screening for bladder cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 155, 246–251 (2011).
Albany-Ward, K. & Sobande, M. What do you really know about colour blindness? Br. J. Sch. Nurs. 10, 123–125 (2015).
Jansone-Langina, Z. & Truksa, R. Evaluation of participants’ awareness of color vision deficiency: a comparative analysis of self-reported diagnosis and objective diagnostic testing. J. Opt. Soc. Am. A 42, B282–B288 (2025).
Wahl, M. D. et al. A comprehensive review of state vision screening mandates for schoolchildren in the United States. Optom. Vis. Sci. 98, 490–499 (2021).
Tan, T. F. et al. Colour vision restrictions for driving: an evidence-based perspective on regulations in ASEAN countries compared to other countries. Lancet Reg. Health Southeast Asia 14, 100171 (2023).
Austin, P. C. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am. J. Epidemiol. 172, 1092–1097 (2010).
Alsoudi, A. F. et al. Risk of intestinal complications, extraintestinal morbidity, and mortality in patients with Crohn’s disease and ocular involvement. Ocul. Immunol. Inflamm. 32, 2486–2493 (2024).
Wai, K. M. et al. Risk of stroke, myocardial infarction, deep vein thrombosis, pulmonary embolism, and death after retinal vein occlusion. Am. J. Ophthalmol. 257, 129–136 (2024).
Palchuk, M. B. et al. A global federated real-world data and analytics platform for research. JAMIA Open 6, ooad035 (2023).
Acknowledgements
P30 Vision Research Core Grant (NEI P30-EY026877 to P.M.) and Research to Prevent Blindness (to P.M.) provided the financial support. The funders had no role in study design, data collection and analysis, and the decision to publish or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
E.R. had full access to all study data and was responsible for the integrity and accuracy of the data analysis. M.F., A.F.A. and E.R. conceptualized and designed the study. M.F. was responsible for acquisition, analysis or interpretation of data, and also contributed to the drafting of the manuscript. E.R., A.F.A. and P.M. were responsible for administrative, technical or material support. E.R. and P.M. were responsible for supervision. All authors were involved in the critical review of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
P.M. is or has been a consultant at Alcon, Amgen, Aura Biosciences, Castle Biosciences, Genentech, Dutch Ophthalmic and Immunogen; is a lecturer at Alcon; and has received financial support from Genentech. E.R. is or has been a consultant at Apellis Pharmaceuticals, Iveric Bio, Genentech, Regeneron, Allergan, Zeiss and Google; and a speaker at Apellis Pharmaceuticals, Genentech, Regeneron and Allergan. The other authors declare no competing interests.
Peer review
Peer review information
Nature Health thanks Masahito Jimbo, Matthew Simunovic, Xiaotao Zhang and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Manonmani Soundararajan, in collaboration with the Nature Health team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fattah, M., Alsoudi, A.F., Mruthyunjaya, P. et al. Impact of colour vision deficiency on bladder and colorectal cancer survival. Nat. Health 1, 113–119 (2026). https://doi.org/10.1038/s44360-025-00032-7
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44360-025-00032-7