Abstract
Clozapine is a potent serotonin receptor antagonist and commonly used for the treatment of Schizophrenia. The study aimed to develop and optimize the transdermal matrix patch of clozapine. A 3-level, 3-factor Central Composite Design was applied to examine and validate the impact of various formulation variables, Eudragit, PEG, and oleic acid on in vitro drug release, flux, and tensile strength (TS). Different formulation characteristics were studied in terms of physico-chemical characterization, Fourier Transform Infrared Spectroscopy (FTIR), Differential Scanning Calorimetry (DSC), drug release performance, and in vitro permeability. The numerical and graphical optimization was based on the desirability function and the optimized formulation obtained from the polynomial equation was further validated and evaluated for the targeted critical attributes. The optimized patch was further evaluated for skin irritation, in vivo pharmacodynamics, in silico prediction, and simulation using the GastroPlus TCAT® model and stability. The experimental results of the optimized formulation, such as tensile strength 1.220 kg/cm2, flux 147.376 μg/cm2/h and Q24 94.874%, showed similarity with the values predicted by numerical and graphical optimization. In vivo Neuro-pharmacological studies showed that the results were comparable to the standard. The Cmax, Tmax, AUCt, and AUCinf were predicted as 38.396 ng/mL, 28.960 h, 1625.500 ng-h/mL, and 1175.700 ng-h/mL for a 50 mg patch. No skin irritation was found for the optimized transdermal patch as per the Draize score method. The shelf life of the optimized formulation was 30.41 months under accelerated conditions. The study showed that the matrix-type transdermal patch of clozapine can be used for the management of schizophrenia in terms of improved patient compliance.
Similar content being viewed by others
Introduction
Clozapine is classified as an atypical antipsychotic that has shown significant success in the treatment of treatment-resistant schizophrenia and exhibited a very low incidence of extrapyramidal side effects. Clozapine is a potent serotonin receptor antagonist, and it has been suggested that serotonin and dopamine receptor antagonism may contribute to its atypical profile. Due to its effects on both negative and positive symptoms of schizophrenia, clozapine is considered the most effective antipsychotic drug1,2. It is commercially available in oral tablet dosage form3. The oral administration of clozapine is related to poor bioavailability (approximately 27%) due to first-pass effect. Therefore, its poor oral bioavailability, low molecular weight (326.823 g/mol), and lipophilic nature (logP 3.500) make it a favorable candidate for transdermal drug delivery system4,5.
The transdermal drug delivery system delivers active therapeutic agents across human skin and offers various advantages over conventional dosage forms. These advantages include patient compliance in long-term therapy, bypassing first-pass metabolism, maintaining a prolonged and constant drug level in plasma, minimizing side effects, and reducing intra and inter-patient variability in response6. In terms of formulation and fabrication, the transdermal drug delivery system has three major types of patches, i.e., matrix type, drug in adhesive type, and reservoir type patch. Matrix-type transdermal patches are fabricated by incorporating the drug in the lipophilic or hydrophilic matrix, forming polymers that control the rate of delivery of the drug across the skin7.
The application of composite polymers like ethyl cellulose (EC), polyvinylpyrrolidone (PVP), hydroxypropyl methylcellulose (HPMC), and Eudragits has been widely reported for matrix transdermal delivery systems8,9,10. The polymers are used to control the release of drugs. Hydrophilic polymers like HPMC and PVP are easily hydrated and release the drug quickly11. Eudragits are derivatives of acrylic and methacrylic esters and are water insoluble12. They have swelling ability and sustained release properties, which are suitable for controlling the release of drugs from transdermal matrix patch formulations13. They are considered non-toxic, non-irritant, easily fabricated, and possess good film-forming characteristics. Eudragit RL100 (E-RL100) and Eudragit RS100 (E-RS100) are generally used in combination in transdermal patch formulation due to their intermediate behavior in terms of hydrophobicity and lipophilicity. The E-RL100 is more hydrophilic and swells rapidly in contact with water, releasing the drug quickly. While the E-RS100 is less permeable to water and highly retard drug release12,14.
Another basic component of this type of system is a plasticizer, which is used to enhance the flexibility and tensile strength of the film. Two major characteristics of an ideal plasticizer are compatibility with the matrix polymers15 and low skin permeability. Some commonly used plasticizers are sorbitol, glycerin, dibutyl phthalate, triethyl citrate, polyethylene glycol, and propylene glycol16. Polyethylene glycol 400 (PEG 400) has been used successfully with E-RL100 and E-RS100 as plasticizers17,18. It is a glycol derivative and a widely used plasticizer due to its non-toxic, compatible, and biodegradable properties16,19.
The human skin acts as a barrier to the permeation of transdermal drugs. Various penetration enhancers such as surfactants, pyrrolidones, essential oils, vegetable oils, and azones, have been studied to improve and enhance the transdermal delivery of drugs. These penetration enhancers improve drug molecules’ flux (permeation) through the skin layers20. Skin’s barrier function is reversibly altered by these agents, allowing the drug molecules with poor permeation characteristics to surpass the skin layers and enter the systemic circulation21. Fatty acids such as linoleic, palmitoleic, and oleic acids are considered safe and effective drug permeation enhancers in transdermal drug delivery systems22. Among these, oleic acid has been reported as the best permeation enhancer23. It interacts with lipid membranes and reduces diffusional resistance24. It is observed that oleic acid with PEG significantly increases the permeation of drugs25.
The evaluation of drugs in animals and humans has traditionally been essential. However, challenges such as rising costs and high failure rates highlighted the need for more reliable and ethical alternatives26. Physiologically based pharmacokinetic (PBPK) modeling, first used in 1973, has become a key in silico tool to predict in vivo pharmacokinetics of various drug delivery systems and provides valuable insights for drug regulation and development. The PBPK modeling is considered an influential tool for the in silico evaluation of transdermal products, as also suggested by the U. S. Food and Drug Administration (FDA)26,27. Similarly, around 30% of the Application Review Files approved by the FDA were found to use PBPK models28.
Previous work on transdermal delivery of clozapine is limited. Formerly, clozapine was formulated into a drug in adhesive patches by Aggarwal et al., 2021, for transdermal delivery of the drug by using different permeation enhancers to increase the flux of the drug across the skin29. In another study, Patel et al., 2020, has developed matrix transdermal patches of clozapine using HPMC K15M and HPMC K4M30. However, the prospect of Clozapine delivery via transdermal patches is a relatively new area of research that requires additional research with the use of matrix polymers such as Eudragit that offer more predictable and controlled delivery of the drug through skin and optimization before clinical evaluation and commercialization31. The current research focuses on developing and optimizing a matrix-type transdermal patch of clozapine using E-RL100 and E-RS100 as matrix polymers with PEG 400 as a plasticizer and oleic acid as a permeation enhancer. In vitro release and permeation behavior of patches were examined using USP apparatus 5 and Franz diffusion cell. Chemical interaction and thermal and mechanical properties were determined. In vivo pharmacodynamics was studied on rats. In vivo pharmacokinetics were predicted using an in silico model, and an accelerated stability study was performed.
Materials and methods
Materials and animals
Clozapine was gifted by Shrook Pharmaceuticals, Lahore, Pakistan. Other chemicals and reagents used were Eudragit RL 100 (Evonik, Darmstadt, Germany), Eudragit RS 100 (Evonik, Darmstadt, Germany), Isopropyl Alcohol (IPA), Acetone (BDH Limite, Poole, England), Oleic Acid, Polyethylene glycol 400 (PEG 400), Ethanol, Methanol (Sigma Aldrich, Steinheim, Germany), potassium dihydrogen phosphate and sodium hydroxide (Merck, Darmstadt, Germany). The transdermal patch components were the backing membrane (3M-9720) and release liner (SCOTCHPAK 9755), gifted by 3M, St. Paul, USA. PVC-based adhesive tape (Uniferoze, Karachi, Pakistan).
Male Albino Wistar rats (weighing 150-200 g), were used for the skin sensitivity and pharmacodynamic studies obtained from the animal house, Faculty of Pharmacy and Health Sciences, University of Balochistan, Quetta. The ARRIVE guidelines for the care and use of laboratory animals were followed32. The animals were kept in a controlled environment (25 ± 1 °C) and free access to food and water was provided. None of the rats were euthanized in the study. The study protocol was reviewed and approved by the Institutional Ethical Committee, Faculty of Pharmacy and Health Sciences, University of Balochistan, vide Ref No. FoP&HS/66/22). All methods were performed in accordance with the relevant guidelines and regulations.
Dose calculation
Controlled release systems deliver the active pharmaceutical ingredient at a constant rate as compared to conventional dosage forms. Baker describes the equation for the calculation of dose (Mo) delivered for a required duration of action (te) from a controlled release system considering Me as minimum effective concentration and t1/2 as the half-life of the drug33.
The minimum effective concentration of clozapine is 0.6 mg/L; half-life and volume of distribution are 2 h and 6 L, respectively34. The patch was designed to deliver the drug for 24 h. The transdermal dose calculated by using (Eq. 1) was
So, ~ 50 mg.
Drug solubility studies
To evaluate the solubility of clozapine in various solvents, like ethanol, acetone, isopropyl alcohol, and methanol, an excess amount of the drug was added into the solvents and stirred using a magnetic stirrer (78-1 Magnetic heating stirrer China) for 24 h at room temperature then the solution was filtered and analyzed through UV visible spectrophotometer (UV-1800, Shimadzu Corporation Kyoto, Japan) at 259 nm. The quantity of drug dissolved was estimated using a calibration curve obtained for the concentration range of 20 to 80 µg/ml (\(\text{y}=0.0099x-0.0073\), \({r}^{2}=0.9992\))21.
Design of experiment
Three factors three level Central composite design (CCD) was used to study the effect of matrix-forming polymer (X1, Eudragit), plasticizer (X2, Polyethylene glycol), and permeation enhancer (X3, oleic acid) as formulation variables on tensile strength of the patch (Y1), flux (Y2) and percentage drug release at 24 h (Y3)35. The Design-Expert Software (version 13.0.1.0, Stat-Ease, Inc. Minneapolis, MN, USA) was used to apply the CCD, and 19 runs were obtained as given in Table 1. The relationship between the input and response variables was expressed by generating response variable curves and perturbation plots and was statistically analyzed by two-way analysis of variance (ANOVA) at significance < 0.05 for the fitness of mathematical models36. A polynomial equation for each response variable was generated, and numerical and graphical optimization techniques were adapted to get the optimum quantities of the input variables and attain the targeted critical responses. Based on the desirability function the predicted formulation was prepared, and the observed responses were compared with that of the predicted ones by calculating the percentage of error (PE ≤ 5%)37. The dependent and independent variables with target constraints are listed in supplementary Table S1. The mathematical relationship between dependent and independent variables is given by the following equation,
where Yi is the dependent variable, B0 is the intercept, B1 to B3 are regression coefficients, and X1, X2, and X3 are the independent variables designated from the initial trials.
Fabrication of clozapine matrix patch
The solvent casting method was used to fabricate the formulations F1-F19 (Table 1)38. Initially, a solution of 50 mg clozapine in 10 ml Isopropanol: Ethanol mixture was used. The required amount of polymers (Eudragit RS-100 and Eudragit RL-100 in 1:1 ratio), plasticizer (Polyethylene glycol), and permeation enhancer (Oleic acid) were then dissolved in the drug mixture (Table 1). The prepared mixture of each formulation was poured on a backing membrane (3M-9720) and placed in a petri dish. The resulting patches were dried at room temperature for 24 h, and a release liner (SCOTCHPAK 9755) was attached. The patches were then cut to appropriate sizes and stored in aluminum foil until further use.
Fourier transform infrared spectroscopy
Fourier Transform Infrared (FTIR) analysis (Thermo-Nicolet AVATAR 330, Madison, USA) was used to study the drug-excipient interactions of the clozapine transdermal patch. Pure clozapine and, matrix gel with clozapine were studied for this purpose. The samples were scanned at a wide spectral range of 4000–500 cm−130. The spectrum was analyzed through EZ OMNIC® version 7.
Differential scanning calorimetry studies
A differential scanning calorimeter (DSC), and Discovery 250 TA instrument (TA Instrument, New Castle, USA) were used to determine the thermal behavior of pure clozapine and clozapine with matrix gel. Instrument calibration was carried out with the Indium standard. Nitrogen purging was set at 50 mL/min through the cooling unit. 3–10 mg of each sample was hermetically sealed and heated with a ramp of 40 °C/min till 220 °C39.
Weight and thickness studies
The prepared clozapine transdermal patches (4 cm × cm) were weighed (n = 5) using an analytical balance (Sartorius CP-2245, Gottingen, Germany). The patches were also measured for uniform thickness by using a Vernier caliper (Mitutoyo, Japan) at random points40.
Drug content evaluation
Clozapine content was determined using a validated liquid chromatographic method as per the USP monograph41. A standard 125 µg/mL solution was prepared in the mobile phase (Methanol:water: triethylamine, 80:20:0.75). The test solutions from the samples of the same nominal concentration were prepared from the patches. Chromatographic separation utilized a C18 column (4.6 × 250 mm, Zorbax Extend C-18) operated at 25 °C with a flow rate of 1 mL/min (HPLC system: Shimadzu LC-20A, Japan). Clozapine was detected at 257 nm using a UV detector (SPD-20A, Shimadzu, Japan).
Moisture content and moisture uptake studies
Arora and Mukherjee42 reported that the method was used to measure the moisture content and uptake of the clozapine transdermal patches. Moisture content was measured after calculating the initial weight of the individual patches and placing them in a desiccator containing activated silica at room temperature. After every 24 h, the patches were weighed individually to obtain a constant weight. The amount of moisture content was calculated by calculating the difference between initial and final weight and dividing by the final weight of the patches, as shown in Eq. 3.
For measuring the moisture uptake, individual patches were weighed and kept in a desiccator containing a saturated solution of potassium chloride at room temperature. After every 24 h, the patches were weighed individually until the weight of the patches was steady. The difference between final and initial weight concerning initial weight (Eq. 4) was applied to calculate the percentage of moisture uptake of the patches42,43.
Evaluation of folding endurance
Folding endurance is defined as the property of a patch that stands for repeated folding at the same point until it is broken. The folding endurance of all the batches of formulated patches was measured by folding them repeatedly at the same point40.
Measurement of tensile strength (TS)
For measuring the mechanical properties of the patch, the tensile strength test was performed using the tensile strength tester (Yuellan YL-S90, China) in compression mode. The instrument consists of two load cells, lower and upper, grips. Each formulation of 4 cm2 was placed on the lower fixed cell grip, and increasing force was applied to the upper mobile cell grip at an extension speed of 5 mm/min. All the formulations were tested in triplicate44,45.
In vitro release studies
The release studies of clozapine from matrix patches (n = 3) were carried out through USP apparatus 5, paddle over the disk (Erweka DT-600, Heusenstamm. Germany). A 600 mL of phosphate buffer pH 7.4 as release medium was filled in the vessel. Temperature was adjusted to 37 ± 0.2 °C. USP transdermal sandwich (90 mm diameter, 17″ mesh, Labecx, Santa Clarita California, USA) was used to hold the patch’s flat surface before immersing it into the medium containing vessel. The paddle was set at 50 revolutions per minute. Aliquots of 10 mL were drawn and replaced with fresh medium at specified time points, i.e., 0.25, 0.5, 1, 2, 3, 4, 6, 8, 12, and 24 h. The drawn samples were assayed through a UV–visible spectrophotometer (UV-1800, Shimadzu Corporation Kyoto, Japan) at 259 nm46,47. Mathematical models such as zero order, first order, Higuchi, and Korsmeyer–Peppas (Eqs. 5–8) were applied to interpret the results48. Rate constants and coefficient of correlation were calculated using DDSolver®49:
where Qo and Qt are the initial amount of drug in dosage form and drug released at time t, respectively. ko, k1, and kH are first-order, zero-order, and Higuchi rate constants, respectively (Eqs. 5–7). “a” is a structural and geometric characteristic of dosage form, and “n” is the release exponent in Korsmeyer–Peppas model (Eq. 8).
In vitro permeation studies
In vitro permeation studies were conducted with the help of Franz diffusion cell (PermeGear V9-CB, USA). The receptor compartment was filled with 5 mL phosphate buffer saline (PBS), pH 7.4. The temperature of the assembly was maintained at 37 ± 0.2 °C through the water circulating jacket. The patches were fixed securely on the Strat-M membrane (Merck Millipore) in such a way that the drug containing surface of the patch was fixed on the glossy surface of the membrane. The surface area of both membrane and patch was 1 cm2. The readings were taken in triplicate. To maintain the sink condition, samples of 0.5 mL were drawn and replaced with an equal volume of medium at specified time intervals, i.e., 0.25, 0.5, 1, 2, 3, 4, 6, 8, 12, and 24 h. The samples were analyzed through HPLC (Shimadzu LC Model 20A)50. The permeation parameters such as permeability coefficient (Eq. 9), lag time (determined by the x-intercept of the linear plot between the amount permeated and time), flux (determined by the slope of the linear plot between the amount permeated and time), diffusion coefficient (Eq. 10), and regression coefficient were determined according to the method stated by Ubaidulla et al.9,51.
where P and DC are the permeation and diffusion coefficients, respectively. “J” denotes the flux, “C” represents the concentration of the drug in a single formulation, “h” is the thickness of the membrane, and “L” is the lag time.
Skin sensitivity test
The skin sensitivity test was performed according to the method reported by Jianping et al.52. For skin irritation studies, Male Wistar Albino Rats (weighing 150–200 g) were used, by dividing them into three groups (n = 5). The rats were kept in cages for seven days before the test to make them adjust to their environment. A day before the experiment, the dorsal abdominal skin of the rats was shaved with an electric clipper. The control group, labeled as Group I, was not given any treatment. For test group II, the optimized clozapine transdermal patch was applied on the animal skin with the help of PVC-based adhesive tape, whereas formalin solution (0.8% v/v) was used to cause skin irritation in group III (Formalin group). The visual signs of erythema and irritation were observed for 6 days and were recorded and scored according to the method mentioned by Draize et al.53.
In vivo neuro-pharmacological studies
To perform various neuro-pharmacological tests (open field, rearing, and forced swimming tests). Male Wistar Albino Rats (weighing 150–200 g) were divided into 3 groups; group I (control) received distilled water orally, and to group II (test) optimized clozapine patch was applied with a size equivalent to the 50 mg/kg clozapine, and to group III (standard) clozapine was given orally in the dose of 50 mg/kg before tests. The in vivo neuro-pharmacological data were subjected to 1-sample t test with significance level (α) at 0.05 using the Minitab Statistical Software version 21.3.1, 2022. A p value < 0.05 indicated a significant difference and > 0.05 presented a no significant difference.
Open field test
The open field test was carried out using an apparatus of an arena surrounded by 42 cm high walls with a total area of 75 cm2 divided into 25 equally distant lines. The experiment was carried out in a quiet area lit by white light. Only the squares crossed with all four paws were counted and the locomotor activity was observed for 10 minutes54.
Rearing test
Animals were put into a 1000 ml beaker to perform the test. Observations were made for 10 min for the sum of upward movement while having their front legs on the walls of the beaker in erect standing position55,56. The exploratory motor activity of the animals was assessed by placing them in a 1000 ml beaker. The number of rearing (standing on the hind limbs in an upright position) was counted for 10 min.
Forced swimming test
The forced swimming test was performed in an apparatus consisting of a transparent cylinder, 30 cm high and 15 cm diameter. The cylinder was filled with tap water, while the temperature was maintained at 25 ± 2 °C throughout the observation. The animals were allowed to swim for 360 s and the last 240 s were observed for the test. All the groups were kept individually, to record the mobility time using a stopwatch. Mobility time was then subtracted from the last 240 s and stated as immobility time. Swimming or trying to get out of the water was considered as mobility and failure to such behavior was considered immobility57,58.
In silico PBPK and simulation of clozapine patches
The systemic disposition of clozapine from optimized transdermal patches was predicted using the ‘Transdermal Compartmental Absorption and Transit’ (TCAT ®) model embedded in GastroPlus™ software version 9.9 (Simulations Plus Inc., Lancaster, CA, USA). Different formulations’, physiological and pharmacokinetic parameters (logP, pKa, blood: plasma ratio, unbound fraction in plasma, effective permeability) obtained from the literature4,59,60 and Absorption, Distribution, Metabolism, Excretion, and Toxicity (ADMET™) predictor (Simulations Plus Inc., Lancaster, CA, USA) module were incorporated as shown in Table 2. The initial validation of the model was performed using experimental plasma profiles for intravenous and oral routes61,62. The pharmacokinetics parameters were calculated after processing in the PKPlus® module of GastroPlus® (compartmental modeling) from the reported in vivo clozapine plasma concentration time. The relative accuracy between predicted PK parameters against the observed PK parameters was calculated by comparing the fold error (FE) between the observed and predicted values according to the Eq. 11:
For simulations in GastroPlus®, “Transdermal → Reservoir Patches” as dosage form was selected for predictive modeling. In the dermal physiology tab, the human arm with a maximum area of 9 cm2 was selected as the dosing application region for simulation. The diffusivity value for the dermal layer was calculated while other layers of skin were used as predicted by the default in silico method present in GastroPlus®. The simulated plasma concentration of the optimized clozapine patch (50 mg) after transdermal administration was compared to the plasma concentration after the oral administration of the 75 mg dose.
Drug stability studies
For stability testing, three batches of the optimized formulation were subjected to accelerated stability conditions (40 °C/75% ± 5% RH) for 6 months in a stability chamber (NuAire, Plymouth, MN, United States), adopting the WHO guidelines of the International Conference on Harmonization (ICH) of “Medicines for Human Use”63. After regular intervals of 0, 1, 3, and 6 months, samples were withdrawn to check any physical appearance change and analyze the flux, drug content, in vitro drug release, and TS (Tensile Strength)64. Formulations were also evaluated for various physical characteristics, including morphology, shape, and color. Statistical software, Minitab, version 19 (Minitab, Pennsylvania, United States) was used to determine the shelf-life.
Results
Solubility studies
For patch formulation purposes, ethanol was selected as the most suitable solvent, along with isopropanol and methanol with acetone. Therefore, ethanol with isopropanol and methanol with acetone was used in the ratios of 50:50. In the case of methanol: acetone, the solubility of the drug was found to be 2.755 ± 0.05 mg/ml while the solubility was 5.238 ± 0.04 mg/ml in ethanol: isopropanol. It was found that most of the matrix polymers were also miscible with these solvent systems. Hence, based on the solubility of the drug and the polymers, a mixture of ethanol and isopropanol (50:50) was selected as a suitable system for the preparation of a matrix patch of clozapine.
Fourier transform infrared studies
The Fourier Transform Infrared (FTIR) spectra of pure clozapine drug demonstrated characteristic peaks at around 3300 cm−1 (N–H stretching), 2990 and 2930 cm−1 (C-H stretching), 1550 cm−1 (aromatic C=N stretching), 1450 cm−1 (C=C stretching), 790 cm−1 (C-Cl stretching) (Fig. 1a). Similarly, IR spectrum of clozapine with polymer gel showed peaks at around 2960 and 1730 cm−1 indicating aliphatic stretching vibration and C=O stretching vibration of the ester group of Eudragit polymer respectively (Fig. 1b).
Differential scanning calorimetry studies
Pure clozapine DSC thermogram showed a single endothermic peak at around 184 °C (Fig. 2a). In the physical mixture of the drug and the matrix gel, a single endothermic peak at around 142 °C and a broadband-wide endothermic peak from around 190 to 220 °C (Fig. 2b).
Weight and thickness studies
The mean weight for formulations, F1 to F19 was in the range of 186.166 ± 1.094 and 393.437 ± 0.858 mg, and the average thickness was recorded between 0.120 ± 0.010 and 0.270 ± 0.010 mm (Table 3).
Drug content evaluation
The mean percentage drug content was between the range of 91.986 ± 1.090% and 93.870 ± 0.910% for the sample (n = 5) formulations (Table 3).
Moisture content and moisture uptake studies
The mean values for moisture content were in the range of 0.500 ± 0.055 to 1.236 ± 0.058%, and mean moisture uptake values were found to be between 0.393 ± 0.102 and 1.216 ± 0.100% (Table 3). A slight increase was observed in moisture content and uptake values when the concentration of the hydrophilic plasticizer (polyethylene glycol) was increased.
Evaluation of folding endurance
The results of the folding endurance showed a folding tolerability of greater than 300 (> 300) repetitions and the patches withstand repeated folding and bending without cracking or breaking (Table 3).
Measurement of tensile strength
The best-fitted model for tensile strength was linear (p = 0.0014), and it was observed that as the concentration of the plasticizer PEG (X2), increased tensile strength increased significantly (p = 0.0002) in a linear fashion as also expressed by the coefficient value in the polynomial equation (+ 0.021) (Table 4). The effect of oleic acid (X3) was also positive but an insignificant rise in tensile strength was observed with the rise in penetration enhancer concentration (p = 0.7516) (Table 4). However, as the Eudragit amount was increased, the tensile strength decreased insignificantly (p = 0.3261). Their relationship is also presented in Figs. 5a-b and 6a. The formulation (F5) containing the highest concentration of PEG 400 (20%) showed the highest tensile strength value of 1.392 kg/cm2 (Table 1).
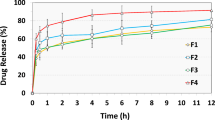
In vitro release studies
Figure 3 represents the release profile of the patches indicating a significant amount of clozapine was released from all the formulations within 24 h. The linear model was the best-fitted model for the in vitro drug release (p < 0.0001). The negative coefficient value (-17.12) also indicated that as the concentration of the polymer (Eudragit) was raised the drug release was controlled (p < 0.0001) (Table 4). as presented in Figs. 5c-d and 6b. The formulations (F5, F6, F7, and F12) containing the maximum amount of Eudragit (200 mg), released comparably lowest amount of clozapine within 24 h.
However, it was observed that PEG 400 and oleic acid participated in increasing the percentage of drug release from the patch, but this effect was insignificant (p = 0.9661 and p = 0.7454). The coefficient values of both X2 and X3 are also low (+ 0.0833 and + 0.6373) (Table 4).
The kinetic models; zero order, first order, Higuchi and Korsmeyer-Peppas were applied to the release data. The results are presented in supplementary Table S2. It was observed that the Korsmeyer Peppas model showed the highest R2 ranging from 0.995 to 0.999 and Model Selection Criteria (MSC) ranging from 3.388 to 7.212 and the lowest Akaike Information Criterium (AIC) ranging from 11.562 to 54.625. The “n” values of the model were ≥ 0.5, showing non-Fickian drug release. The Korsmeyer Peppas release constant (kKP) was highest in formulations with low concentrations of polymers and decreased proportionally with an increase in the number of polymers. The dissolution profile of the clozapine patches after the Korsmeyer Peppas model was best fitted in the Higuchi model.
In vitro permeation studies
The cumulative amount of clozapine from the formulations ranged from 2936.04 to 4045.74 µg/cm2 (Fig. 4), and the flux value from 124.909 to 182.049 μg/cm2/h (Table 1). The permeation parameters were computed and presented in Table 5. The relationship of the independent variables with flux is best fitted to the linear model (p < 0.0001). The oleic acid concentration significantly increased flux (p < 0.0001) as also expressed by the coefficient value (+ 14.56) (Table 4). The highest flux of 182.049 µg/cm2/h (Table 1) with a lag time of 0.618 h (Table 5) was obtained at 2.34% oleic acid (F6). The influence of PEG 400 (plasticizer) was also found positive on flux but statistically insignificant (p = 0.4473). The relationship is presented in Figs. 5e-f and 6c. Whereas the rate-controlling polymer Eudragit (X1) higher concentration, reduced the flux insignificantly (p = 0.4593) which is also clear from the coefficient value (-1.46) (Table 4).
Response surface 3D curves showing effect of Eudragit (X1), PEG (X2) and Oleic acid (X3) on Tensile strength (Y1), Flux (Y2) and Q24, drug release percentage at 12 h (Y3). The interactive effect of Eudragit and PEG, and Eudragit and Oleic acid on (a, b) tensile strength, (c, d) flux and (e, f) % drug release (Q) at 24 h.
Optimization by experimental design
The influence of parameters including the amount of polymer (X1), the concentration of permeation enhancer (X2), and the concentration of plasticizer (X3) were examined on the Tensile Strength (Y1), flux (Y2), and Q24 (% drug release after 24 h) (Y3) to optimize the clozapine transdermal matrix type patch. The relationship between the input and output variables is presented by 3D response surface curves (Fig. 5a-f). The perturbing effect of independent variables on critical response variables (Y1-Y3) is expressed in Fig. 6a-c.
The data of experimental batches, and results obtained from the CCD, were utilized to detect ideal conditions for the clozapine matrix patch to obtain an optimized formulation based on the target constraints and, for all conditions, the desirability was found to be 1. Based on the desirability parameters, the software suggested the predicted values of the optimized batch for TS as 0.971 kg/cm2, flux as 133.936 μg/cm2/h, and Q24 as 85% (see Fig. 7a,b and Table 6).
The optimized formulation (Fopt.) demonstrated experimental values, with a TS of 1.220 kg/cm2, a flux of 147.376 μg/cm2/h, and a Q24 release of 94.874% (Table 6).
Skin sensitivity test
The optimized batch was studied and compared with standard irritants for skin sensitivity (Fig. 8). After applying the patch and the standard irritant, the animals were visually inspected for any type of allergy, redness, rashes, and irritation. The Draize score method was applied to interpret the results. Scores for control (Group I), optimized clozapine patch, Formulation Fopt., (Group II), and formalin (Group III) are provided in Table 7. The scores of 2 or less than 2 were deemed as negative9. Scores after applying the clozapine patch (Fopt.) were recorded 1 ± 0.707 and 0.4 ± 0.547 for edema and erythema, respectively.
In vivo neuro-pharmacological studies
Neuro-pharmacological studies including open-field, rearing and forced-swimming tests were conducted on rats and the results are presented as under (Table 8).
Open field test
The mean number of squares crossed for the control group was 165.431 ± 2.953 squares, while for the clozapine matrix patch was 174.760 ± 2.110 squares, and for the clozapine (standard drug) treated group was 178.153 ± 1.625 squares (P value = 0.014). The values were obtained for the matrix patch which suggests that the open field activity of the patch is comparable to the standard drug (Table 8).
Rearing test
The results of the rearing test showed that the mean number of moving attempts for the control group was 50.396 ± 1.311, and 59.261 ± 1.233 for the clozapine matrix patch while in the clozapine (standard drug) treated group it was 62.180 ± 1.220 (P value = 0.005). These results indicate that the rearing test of the patch is comparable to the standard drug (Table 8).
Forced swimming (mobility time) test
The results of the forced swimming test showed that the mean time spent for immobility by control 103 ± 15, standard 70 ± 08, and test 82 ± 09 s (P = value 0.037). Immobility in water is considered specific to depression and reduction in immobility might be due to diminished fear or the anxiolytic effect of clozapine65,66.
In silico PBPK and simulation of clozapine patches
Different formulations and pharmacokinetic and physiological parameters are illustrated in Table 9. The pharmacokinetics parameters for the intravenous and oral routes calculated with PKPlus® and reported literature were clearance = 0.479 L/h/kg, half-life (t1/2) = 5.1 h, and volume of distribution (Vd) = 3.5 L/kg. The mean pharmacokinetic parametric values for the IV, oral and transdermal simulated curves were calculated as 2521.800 ng/mL (Cmax), 0.024 h (Tmax), 980.880 ng-h/mL (AUCt) and 990.750 ng-h/mL (AUCinf) for 25 mg IV, 81.986 ng/mL (Cmax), 2.853 h (Tmax), 956.660 ng-h/mL (AUCt) and 985.180 ng-h/mL (AUCinf) for 75 mg oral and 38.396 ng/mL (Cmax), 28.960 h (Tmax), 1625.500 ng-h/mL (AUCt) and 1175.700 ng-h/mL (AUCinf) for 50 mg transdermal routes respectively. The fold error value among experimental and simulated results was found less than 2.
Drug stability studies
The results of the stability studies showed, that the physical appearance of the patch was unchanged after 6 months. The drug content of the patch was found to be 93.15 ± 0.69% after 6 months, while Q24, TS, and flux were observed as, 93.65 ± 0.54%, 1.01 ± 0.43 kg/cm2, and 161.50 ± 0.81 μg/cm2/h, respectively (Supplementary Table S3 and Fig. S1). A significant difference was observed between months (p value = 0.028) and no significant difference was found between the batches (p value = 0.554) for clozapine content during the stability period. The shelf life of the patch was calculated through Minitab® 19.2020.1 (USA) and it was found to be 30.405 months.
Discussion
Solubility studies
Clozapine is a BCS class II drug and has poor solubility in water. Li, C., et al. in their study ranked the solubility of clozapine as water < isopropanol < ethanol < methanol < acetone < DMF respectively67. Consequently, solubility studies of clozapine were conducted to select the most appropriate solvent system for film casting68. Clozapine was found more soluble in Ethanol and isopropanol mixture (50:50). Eudragit RL 100 and RS 100 were also soluble in this solvent mixture69.
Design of experiment
The formulation factors and their levels were selected based on the literature review30,38. It has been found that polymers, plasticizers, and permeation enhancers are important excipients for formulating matrix-type transdermal drug delivery systems that affect the behavior of drug release and permeation from the system, as well as elastic properties of the matrix patch70. The release of the drug from transdermal patches ensures its ability to cross the barrier membrane and produce therapeutic or pharmacological effects, with the release rate directly influencing the amount of its permeation. Moreover, adequate elasticity is required to maintain the physical integrity of the patch and resist patch fracture with skin folding71. In this work, Eudragit RS-100 and Eudragit RL-100 were used as matrix-forming polymers to achieve controlled release of clozapine, with polyethylene glycol as a plasticizer and oleic acid as a permeation enhancer.
Fourier transform infrared studies
The FTIR spectra of pure clozapine drug and matrix gel with clozapine were studied. The characteristic peaks of clozapine were observed, confirming the identity of clozapine. FTIR spectrum of polymer gel with clozapine showed peaks similar to the pure clozapine at around 1400 to 700 cm−1 but the spectrum suggests the clozapine is dispersed within the polymer network. This indicates the proper blending of clozapine within the polymer matrix. Other researchers have also observed the same behavior of clozapine in polymer systems72,73.
Differential scanning calorimetry studies
DSC thermogram of clozapine alone and with matrix gel were determined. A single endothermic peak of pure clozapine at around 184 °C corresponding to its melting at this temperature and indicates the crystalline nature of the clozapin. The same peak was not visible with matrix polymer while the appearance of a broadband-wide endothermic peak from around 190 to 220 °C is considered might be due to the dispersion of clozapine in an amorphous state in the presence of Eudragit polymers and their melting. A single endothermic peak at around 142 °C is considered due to Eudragit polymer29,73.
Weight and thickness studies
The weight and thickness of the formulation were determined and their mean and SD values were calculated. The low ± SD values and minimal differences in mean weight and thickness, suggest uniformity among the formulated patches. The uniformity in weight and thickness of the patches is indicative of the fact that the method adopted for the formulation of patches is reproducible38.
Drug content evaluation
The drug content of all the formulations was within the pharmacopeial acceptable range of 90–110%41. Therefore, all formulations passed the content uniformity test.
Moisture content and Moisture uptake studies
Evaluation of moisture content and moisture uptake is an important measure of the diffusion of drugs across the skin; it reveals the uptake of water by the patch from cells and the environment when applied to the skin74. The prepared patches showed low moisture content and moisture uptake, enhancing their stability and reducing the chances of brittleness during storage.
Evaluation of folding endurance
The folding endurance is a measure of the durability and flexibility of the transdermal patch. The results of the folding endurance indicated a better flexibility and capacity of the patch to remain intact at high mechanical stress (Table 3). This also helps keep the patch intact in case of skin folding after application75.
Measurement of tensile strength
Tensile strength validates the strength of the fabricated patches and the possibility of film cracking76. It has been observed that increasing the concentration of PEG and oleic acid in the formulation increased the tensile strength (Y1). This could occur due to improvement in the flexibility of matrix polymer by the plasticizer and permeation enhancer77,78. It has been reported that oleic acid used in the transdermal formulation improved the plasticizing property of the polymer77. However, a decrease in the tensile strength was observed as the amount of Eudragit increased. This decrease in tensile strength could occur due to an increase in the brittleness of the matrix patch thereby decreasing the patch’s mechanical stability and strength79. Hence, the results of the tensile strength folding endurance test indicated that the patches are strong as well as elastic and therefore could withstand forces of wear and tear during handling.
In vitro release studies
In matrix-type transdermal patches, drug delivery is mainly influenced by the release of drugs from the patches80. The release of clozapine was observed controlled with an increase in the concentration of Eudragit and the release was lowest from the formulations that contained the highest amount of Eudragit. A possible cause of this effect is the fact that polymer solution viscosity increases by increasing polymer concentration which ultimately forms the viscous barrier around the patch and hinders its release in dissolution media81. It has been reported that the drug release from these types of polymers is governed by the absorption of water from the medium and swelling of polymer film12. In addition, the presence of a plasticizer, PEG 400, also accounts for the highest drug release by improving the flexibility and smoothness of Eudragit patches82.
To determine the release kinetics of the patches, data obtained from in vitro drug release studies were plotted in various kinetic models. It is generally considered that an appropriate model is one with the highest R2 and MSC and lowest AIC values83. Similarly, the clozapine transdermal formulations were best fitted with the Korsmeyer Peppas model with non-Fickian drug release. The same model was observed and fitted by Kaur et al. where transdermal patches of astaxanthin were formulated using HPMC and Eudragit as matrix polymers84. The Higuchi model was also fitted indicating diffusion controlled release mechanism. Previously the matrix-type transdermal patches of chlorpheniramine maleate were prepared using eudragit polymer, followed the diffusion-controlled release kinetics85.
In vitro permeation studies
Because of the increase in the concentration of independent variables, the cumulative amount permeation of clozapine and the flux varied among the formulations. The flux was observed to increase with an increase in the concentration of oleic acid. This increase, presumably, is caused by enhanced partitioning of a drug in a lipophilic membrane causing lipid fluidization and, thereby, increasing the flux of the drug86. It was also observed that increasing the concentration of permeation enhancer (Oleic Acid) increased the amount of clozapine permeation and decreased lag time. In a previous study conducted by Agarwal et al., the flux of the clozapine transdermal patch was found to be 90.84 ± 1.48 µg/cm2/h when oleic acid was used as a penetration enhancer29. Lipophilicity was considered the most important factor influencing the penetration of the drug through the skin87. Oleic Acid is a fatty acid of lipophilic nature88, and its log P value is 7.789. Due to its physicochemical properties, Oleic Acid induces the partitioning of the drug (clozapine) from the matrix patch to the lipophilic membrane and, afterward, into the acceptor phase. In addition, disrupting the lipid bilayer and increasing the flux of the drug is another significant characteristic of Oleic Acid90. Moreover, the addition of plasticizers such as PEG 400 in a transdermal patch increases the mobility and flexibility of the polymer chain, thereby resulting in improved flux of the drug30. While the flux was observed to decrease with an increase in the concentration of Eudragit. A possible cause of this effect is the fact that an increase in the amount of polymer forms thickened gel-like solution which retards the diffusion of drug molecules from the matrix patch to the skin surface91.
Optimization using design of experiment
The marked similarity was recorded between the predicted values and measured practical values. The predicted values were very close to the practical values, which suggested the precision and consistency of the mathematical model. Hence, it was concluded that the proposed model could be applied to know about the design space.
Skin sensitivity test
The optimized formulation (Fopt.) was studied for skin sensitivity. The Draize scores after applying the clozapine patch were found optimum. In a previous study by Patel, 2020, similar results of the Draize score for matrix-type transdermal patches of clozapine were found, i.e., 0.67 ± 0.52 for erythema and 0.83 ± 0.41 for edema30. Therefore, the Fopt. can be said free of any skin sensitivity reaction.
In vivo neuro-pharmacological studies
The most common use of animal models is to predict and record the therapeutic response of any pharmacological agent92. In this regard, several neuro-pharmacological studies were conducted on Male Albino Wistar Rats to establish the effects of clozapine in in vivo animal models.
Open field test
In previous studies, an open-field test has been conducted to validate it as an important behavioral model for showing anxiety93. The open-field model induces fear in rodents by triggering feelings of social isolation in large empty spaces. It has been observed that anxiolytic treatment increases exploratory and locomotor activities94. In a study conducted by Mead et al., 2008, it was demonstrated that clozapine possesses an intrinsic anxiolytic property that is not related to its anti-psychotic effect or its effects on motor functions or memory processes and learning95. The results of our study showed an adequate increase in total square crossings and locomotion, thus suggesting anxiolytic behavior in animals treated with clozapine.
Rearing test
Rearing is also considered a measure of exploration and animals show a decrease in this behavior when they are introduced in a novel and unfamiliar environment. Opposite of this behavior has been observed in animals treated with anxiolytic agents94. Previously, it has been established that atypical antipsychotics, such as clozapine and olanzapine do possess anxiolytic effects95. The results of the study showed an increase in rearing frequency and number in the clozapine-treated group, thus suggesting its anxiolytic potential.
Forced swimming (mobility time) test
A forced swimming test is performed to evaluate the antidepressant effects of pharmacological agents96. In the present study, animals treated with clozapine transdermal patch spent more time in struggling on the surface of the water, indicating antidepressant activity and results are comparable with a reference group.
In silico PBPK and simulation of clozapine patches
The prediction of the systemic disposition for the optimized clozapine transdermal patch was carried out using the TCAT® model. Analyzing the IV and oral administration of 25 mg and 75 mg clozapine respectively to simulate the systemic disposition in individuals with an average weight of 70 kg as a comparison parameter, the two-compartmental model was selected with the help of the PKPlus® module97. Observing the fold error value less than 2 among experimental and simulated results suggested that the predicted values are comparable with the experimental values.
After testing different clozapine application areas and dosage values, the model integrated pharmacokinetic parameters and TCAT® model for the optimized clozapine patch using values of 50 mg as the dose and 9 cm2 as the application surface area. The predicted plasma concentration profiles after 75 mg oral and 50 mg transdermal administration of Clozapine are shown in Fig. 9a. A similarity between bioavailability profiles can be readily observed from both curves though having different dosage strengths Fig. 9b, which may be explained by the fact that clozapine shows 27% to 35% oral bioavailability98,99. A cumulative increase in the plasma concentration of clozapine administered by a transdermal route as shown in Fig. 9c was a bit slower at the initial treatment when compared with the oral route; however, it becomes equivalent to oral plasma concentration in 10–15 h. This suggests that continuous therapy with multiple dosing could maintain the plasma levels in the therapeutic window above minimum therapeutic concentration.
This is an important feature of the transdermal route as the release kinetics and cutaneous absorption can provide controlled plasma drug concentrations100. Thus, based on the in silico pharmacokinetic model, it was possible to formulate reservoir-type transdermal patches as an alternative to oral administration, thereby avoiding excessive hepatic elimination and suspected side effects.
Drug stability studies
The optimized formulation was observed to be safe, potent and effective throughout its storage at accelerated conditions. The drug content of the patches was within the specified pharmacopeial limits, while the release and permeation data were optimum. Similarly, in a previous study conducted by Agarwal et al., comparable results were obtained and the clozapine transdermal patch showed significant stability after six months with assay and flux of 98.76 ± 0.37%, and 104.89 ± 1.43 μg/cm2/h, respectively29.
Conclusion
The matrix-type transdermal patch of clozapine was formulated and optimized using a central composite design with the 3-level, 3-factor model. The patch comprising matrix polymers, Eudragit RS 100 and Eudragit RL 100, polyethylene glycol as a plasticizer, and oleic acid as a permeation enhancer could be ideal for the transdermal delivery of clozapine. The in vitro studies of the patch suggested efficient delivery of the drug across the skin. This was also reinforced by conducting in vivo neuro-pharmacological studies in animals. A plasma level comparable to oral and IV routes with a fold error of less than 2 was also predicted for a 50 mg patch from the in silico model. The optimized formulated clozapine matrix patch, with no skin irritation (Formulation Fopt.), can be used as a suitable and appropriate alternative for delivering clozapine by the transdermal route and achieving better patient compliance with minimal side effects.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Yang, Z. et al. Once-daily versus divided dosing regimens of clozapine: A cross-sectional study in Singapore. Schizophr. Res. https://doi.org/10.1016/j.schres.2023.10.001 (2023).
Nucifora, F. C. Jr., Mihaljevic, M., Lee, B. J. & Sawa, A. Clozapine as a model for antipsychotic development. Neurotherapeutics 14, 750–761. https://doi.org/10.1007/s13311-017-0552-9 (2017).
Pharma, M. Clozapine Prescribing Information (2021).
Lee, J., Kim, M.-G., Jeong, H.-C. & Shin, K.-H. Physiologically-based pharmacokinetic model for clozapine in Korean patients with schizophrenia. Transl. Clin. Pharmacol. 29, 33 (2021).
Manjunath, K. & Venkateswarlu, V. Pharmacokinetics, tissue distribution and bioavailability of clozapine solid lipid nanoparticles after intravenous and intraduodenal administration. J. Control. Release 107, 215–228. https://doi.org/10.1016/j.jconrel.2005.06.006 (2005).
Prausnitz, M. R. & Langer, R. Transdermal drug delivery. Nat. Biotechnol. 26, 1261–1268 (2008).
Prausnitz, M. R., Mitragotri, S. & Langer, R. Current status and future potential of transdermal drug delivery. Nat. Rev. Drug Discov. 3, 115–124 (2004).
Gannu, R., Vamshi Vishnu, Y., Kishan, V. & Madhusudan Rao, Y. Development of nitrendipine transdermal patches: in vitro and ex vivo characterization. Curr. Drug Deliv. 4, 69–76 (2007).
Ubaidulla, U., Reddy, M. V., Ruckmani, K., Ahmad, F. J. & Khar, R. K. Transdermal therapeutic system of carvedilol: Effect of hydrophilic and hydrophobic matrix on in vitro and in vivo characteristics. Aaps Pharmscitech 8, E13–E20 (2007).
Kusum Devi, V., Saisivam, S., Maria, G. & Deepti, P. Design and evaluation of matrix diffusion controlled transdermal patches of verapamil hydrochloride. Drug Dev. Ind. Pharm. 29, 495–503 (2003).
Pratiwi, G., Susanti, S. & Shiyan, S. Application of factorial design for optimization of PVC-HPMC polymers in matrix film ibuprofen patch-transdermal drug delivery system. Indonesian J. Chemom. Pharm. Anal. 11–21 (2020).
Hayyat, A. & Siddique, N. Individual and combined effect of Eudragit® RS 100 and Eudragit® RL 100 on sustained release characteristics of ropinirole HCl-loaded microparticles. Pharm. Sci. Res. 10, 6 (2023).
Manna, S., Dhanalakshmi, D., Bhowmik, M., Jana, S. & Jana, S. Cellulose derivative-based bioadhesive blend patch for transdermal drug delivery. Front. Mater. 9, 835507. https://doi.org/10.3389/fmats.2022.835507 (2022).
Mutalik, S. & Udupa, N. Glibenclamide transdermal patches: Physicochemical, pharmacodynamic, and pharmacokinetic evaluations. J. Pharm. Sci. 93, 1577–1594. https://doi.org/10.1002/jps.20058 (2004).
Li, D. et al. Preparation of plasticized poly (lactic acid) and its influence on the properties of composite materials. PLOS ONE 13, e0193520. https://doi.org/10.1371/journal.pone.0193520 (2018).
Güngör, S., Erdal, M. S. & Özsoy, Y. Plasticizers in transdermal drug delivery systems. Recent Adv. Plast. 5, 91–112 (2012).
Wu, P. C., Tsai, P. J., Lin, S. C. & Huang, Y. B. Formulation optimization of arecoline patches. Sci. World J. 2014, 945168. https://doi.org/10.1155/2014/945168 (2014).
Asnani, A. J. & Parashar, V. V. Effect of different plasticizers on Eudragit RS100 and RL100 free film. Der Pharmacia Lettre 3, 257–263 (2011).
Ahmed, T. A., El-Say, K. M., Aljaeid, B. M., Fahmy, U. A. & Abd-Allah, F. I. Transdermal glimepiride delivery system based on optimized ethosomal nano-vesicles: Preparation, characterization, in vitro, ex vivo and clinical evaluation. Int. J. Pharm. 500, 245–254. https://doi.org/10.1016/j.ijpharm.2016.01.017 (2016).
Schafer, N., Balwierz, R., Biernat, P., Ochędzan-Siodłak, W. & Lipok, J. Natural ingredients of transdermal drug delivery systems as permeation enhancers of active substances through the stratum corneum. Mol. Pharm. 20, 3278–3297. https://doi.org/10.1021/acs.molpharmaceut.3c00126 (2023).
Mittal, A., Sara, U. S., Ali, A. & Mohammed, A. Design, development, physicochemical, in vitro and in vivo evaluation of monolithic matrix type transdermal patches containing nitrendipine. Pharm. Dev. Technol. 14, 422–434 (2009).
Kim, M.-J. et al. Skin permeation enhancement of diclofenac by fatty acids. Drug Deliv. 15, 373–379. https://doi.org/10.1080/10717540802006898 (2008).
Gupta, R., Dwadasi, B. S., Rai, B. & Mitragotri, S. Effect of chemical permeation enhancers on skin permeability: In silico screening using Molecular Dynamics simulations. Sci. Rep. 9, 1456. https://doi.org/10.1038/s41598-018-37900-0 (2019).
Walker, M. & Hadgraft, J. Oleic acid: A membrane “fluidiser” or fluid within the membrane?. Int. J. Pharm. 71, R1–R4. https://doi.org/10.1016/0378-5173(91)90078-3 (1991).
Padula, C., Pescina, S., Nicoli, S. & Santi, P. New insights on the mechanism of fatty acids as buccal permeation enhancers. Pharmaceutics https://doi.org/10.3390/pharmaceutics10040201 (2018).
Chen, A., Yarmush, M. L. & Maguire, T. Physiologically based pharmacokinetic models: integration of in silico approaches with micro cell culture analogues. Curr. Drug Metab. 13, 863–880. https://doi.org/10.2174/138920012800840419 (2012).
Wang, W. & Ouyang, D. Opportunities and challenges of physiologically based pharmacokinetic modeling in drug delivery. Drug Discov. Today 27, 2100–2120. https://doi.org/10.1016/j.drudis.2022.04.015 (2022).
Sun, Z. et al. Application of physiologically based pharmacokinetic modeling of novel drugs approved by the U.S. food and drug administration. Eur. J. Pharm. Sci. 200, 106838. https://doi.org/10.1016/j.ejps.2024.106838 (2024).
Agrawal, M. B. & Patel, M. M. Design, development and in vivo evaluation of clozapine loaded adhesive diffusion controlled system for the treatment of schizophrenia. J. Drug Deliv. Sci. Technol. 64, 102629 (2021).
Patel, M. M. Formulation, optimization, and in vivo evaluation of clozapine loaded transdermal drug delivery system for the treatment of schizophrenia. Asian J. Pharm. (AJP) 14 (2020).
Nikam, A. et al. A systematic overview of Eudragit® based copolymer for smart healthcare. Pharmaceutics 15, 587 (2023).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. The ARRIVE guidelines animal research: Reporting in vivo experiments. PLoS Biol 8, e1000412 (2010).
Baker, R. W. Controlled Release of Biologically Active Agents. (John Wiley & Sons, 1987).
Stark, A. & Scott, J. A review of the use of clozapine levels to guide treatment and determine cause of death. Aust. N. Z. J. Psychiatry 46, 816–825 (2012).
Adena, S. K. R., Upadhyay, M., Vardhan, H. & Mishra, B. Development, optimization, and in vitro characterization of dasatinib-loaded PEG functionalized chitosan capped gold nanoparticles using Box-Behnken experimental design. Drug Dev. Ind. Pharmacy 44, 493–501 (2018).
Parhi, R. & Suresh, P. Formulation optimization and characterization of transdermal film of simvastatin by response surface methodology. Mater. Sci. Eng. C 58, 331–341 (2016).
Farooqi, S. et al. Quality by design (QbD)-based numerical and graphical optimization technique for the development of osmotic pump controlled-release metoclopramide HCl tablets. Drug Des. Dev. Therapy 14, 5217–5234. https://doi.org/10.2147/DDDT.S278918 (2020).
Aggarwal, G., Dhawan, S. & Harikumar, S. Formulation, in vitro, and in vivo evaluation of matrix-type transdermal patches containing olanzapine. Pharm. Dev. Technol. 18, 916–925 (2013).
Siddiqui, F. et al. Formulation development and optimization of taste-masked azithromycin oral suspension with ion exchange resins: Bioanalytical method development and validation, in vivo bioequivalence study, and in-silico PBPK modeling for the paediatric population. J. Drug Deliv. Sci. Technol. 79, 104048 (2023).
Sarkar, G. et al. Taro corms mucilage/HPMC based transdermal patch: An efficient device for delivery of diltiazem hydrochloride. Int. J. Biol. Macromol. 66, 158–165 (2014).
USP24-NF24. Clozapine tablet, http://www.pharmacopeia.cn/v29240/usp29nf24s0_m19050.html#google_vignette (2021).
Arora, P. & Mukherjee, B. Design, development, physicochemical, and in vitro and in vivo evaluation of transdermal patches containing diclofenac diethylammonium salt. J. Pharm. Sci. 91, 2076–2089 (2002).
Bagyalakshmi, J., Vamsikrishna, R. P., Manavalan, R., Ravi, T. K. & Manna, P. K. Formulation development and in vitro and in vivo evaluation of membrane-moderated transdermal systems of ampicillin sodium in ethanol: pH 4.7 buffer solvent system. AAPS PharmSciTech 8, E50–E55 (2007).
Ghosh, T. K. et al. Assessment of morphology and property of graphene oxide-hydroxypropylmethylcellulose nanocomposite films. Int. J. Biol. Macromol. 66, 338–345 (2014).
Satturwar, P. M., Fulzele, S. V. & Dorle, A. K. Evaluation of polymerized rosin for the formulation and development of transdermal drug delivery system: A technical note. AAPS Pharmscitech 6, E649–E654 (2005).
Imtiaz, M. S. et al. Formulation development and evaluation of drug-in-adhesive-type transdermal patch of metoclopramide HCl. Polym. Bull. (2022).
Agnihotri, S. A. & Aminabhavi, T. M. Controlled release of clozapine through chitosan microparticles prepared by a novel method. J. Control. Release 96, 245–259. https://doi.org/10.1016/j.jconrel.2004.01.025 (2004).
Costa, P. & Sousa Lobo, J. Evaluation of mathematical models describing drug release from estradiol transdermal systems. Drug Dev. Ind. Pharm. 29, 89–97 (2003).
Zhang, Y. et al. DDSolver: an add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 12, 263–271 (2010).
Haq, A., Goodyear, B., Ameen, D., Joshi, V. & Michniak-Kohn, B. Strat-M® synthetic membrane: Permeability comparison to human cadaver skin. Int. J. Pharm. 547, 432–437. https://doi.org/10.1016/j.ijpharm.2018.06.012 (2018).
Sikandar, M. et al. Nanoclay-based composite films for transdermal drug delivery: Development, characterization, and in silico modeling and simulation. Int. J. Nanomed. 3463–3481 (2022).
Jianping, W. et al. Development and evaluation of the sinomenine transdermal patch (2008).
Draize, J. H. Methods for the study of irritation and toxicity of substances applied topically to the skin and mucous membranes. J. Pharmacol. Exp. Ther. 82, 377–390 (1944).
Abdul Jabbar, S. M. et al. Studies on neuropharmacological and analgesic effects of Periploca aphylla extract in mice. Pure Appl. Biol. (PAB) 5, 1207–1215 (2021).
Kasture, V. S., Deshmukh, V. & Chopde, C. Anxiolytic and anticonvulsive activity of Sesbania grandiflora leaves in experimental animals. Phytother Res. 16, 455–460 (2002).
Sanchez-Mateo, C., Prado, B. & Rabanal, R. Antidepressant effects of the methanol extract of several Hypericum species from the Canary Islands. J. Ethnopharmacol. 79, 119–127 (2002).
Iqbal, J., Muhammad, S. & Ahmad, M. Evaluation of acute toxicity, sedative and analgesic effects of Taverniera glabra methanolic extract on mice. Pak. J. Pharm. Sci. 29 (2016).
Can, A. et al. The mouse forced swim test. J. Visual. Exp.: JoVE e3638. https://doi.org/10.3791/3638 (2012).
Tassaneeyakul, W. et al. Steady-state bioequivalence study of clozapine tablet in schizophrenic patients. 8, 47–53 (2005).
DrugBank. Clozapine hydrochloride. https://go.drugbank.com/salts/DBSALT002286 (2005).
Cheng, Y. F., Lundberg, T., Bondesson, U., Lindström, L. & Gabrielsson, J. Clinical pharmacokinetics of clozapine in chronic schizophrenic patients. Eur. J. Clin. Pharmacol. 34, 445–449. https://doi.org/10.1007/BF01046700 (1988).
Choc, M. G. et al. Single- vs multiple-dose pharmacokinetics of clozapine in psychiatric patients. Pharm. Res. 7, 347–351. https://doi.org/10.1023/A:1015859103824 (1990).
Organization, W. H. Stability testing of active pharmaceutical ingredients and finished pharmaceutical products, Annex 10. WHO Expert Comm Specif Pharm Prep 52, 309–351 (2018).
Banerjee, S. et al. Accelerated stability testing of a transdermal patch composed of eserine and pralidoxime chloride for prophylaxis against (±)-anatoxin A poisoning. J. Food Drug Anal. 22, 264–270 (2014).
Porsolt, R. D., Anton, G., Blavet, N. & Jalfre, M. Behavioural despair in rats: a new model sensitive to antidepressant treatments. Eur. J. Pharmacol. 47, 379–391. https://doi.org/10.1016/0014-2999(78)90118-8 (1978).
Slattery, D. A. & Cryan, J. F. Using the rat forced swim test to assess antidepressant-like activity in rodents. Nat. Protoc. 7, 1009–1014. https://doi.org/10.1038/nprot.2012.044 (2012).
Li, C. et al. Enhancement of clozapine solubility in three aqueous choline chloride-based deep eutectic solvents: Experimental and COSMO-RS prediction. J. Mol. Liq. 359, 119298. https://doi.org/10.1016/j.molliq.2022.119298 (2022).
Yu, S. et al. Solid-liquid phase equilibrium of clozapine in aqueous binary solvent mixtures. Journal of Molecular Liquids 329, 115371 (2021).
Chavda, Y., Bhimani, B., Patel, G. & Daslaniya, D. Preparation and evaluation eudragit® polymers by solvent.
Kakar, S., Singh, R. & Semwal, A. Transdermal drug delivery as a boon. Asian Pac. J. Health Sci. 1, 13–25 (2014).
Imtiaz, M. S. et al. Formulation development and evaluation of drug-in-adhesive-type transdermal patch of metoclopramide HCl. Polym. Bull. 1–14 (2021).
Ali, A., Ali, A. & Maghrabi, I. Clozapine-carboxylic acid plasticized co-amorphous dispersions: Preparation, characterization and solution stability evaluation. Acta Pharm. (Zagreb, Croatia) 65, 133–146. https://doi.org/10.1515/acph-2015-0014 (2015).
Akhgari, A., Heshmati, Z. & Makhmalzadeh, B. S. Indomethacin electrospun nanofibers for colonic drug delivery: preparation and characterization. Adv. Pharm. Bull. 3, 85 (2013).
Patel, K. N., Patel, H. K. & Patel, V. A. Formulation and characterization of drug in adhesive transdermal patches of diclofenac acid. Int. J. Pharm. Pharm. Sci. 4, 296–299 (2012).
Nair, R. S., Ling, T. N., Shukkoor, M. S. A. & Manickam, B. Matrix type transdermal patches of captopril: ex vivo permeation studies through excised rat skin. J. Pharm. Res. 6, 774–779 (2013).
Garala, K. C., Shinde, A. J. & Shah, P. H. Formulation and in-vitro characterization of monolithic matrix transdermal systems using HPMC/Eudragit S 100 polymer blends. Int. J. Pharm. Pharm. Sci. 1, 108–120 (2009).
Ghanbarzadeh, B. & Almasi, H. Physical properties of edible emulsified films based on carboxymethyl cellulose and oleic acid. Int. J. Biol. Macromol. 48, 44–49. https://doi.org/10.1016/j.ijbiomac.2010.09.014 (2011).
Luangtana-anan, M., Nunthanid, J. & Limmatvapirat, S. Effect of molecular weight and concentration of polyethylene glycol on physicochemical properties and stability of shellac film. J. Agric. Food Chem. 58, 12934–12940. https://doi.org/10.1021/jf1031026 (2010).
El-Malah, Y. & Nazzal, S. Effect of Eudragit RS 30D and talc powder on verapamil hydrochloride release from beads coated with drug layered matrices. AAPS PharmSciTech 9, 75–83. https://doi.org/10.1208/s12249-007-9008-6 (2008).
Sharma, S., Aggarwal, G. & Dhawan, S. Design and evaluation of Olanzapine transdermal patches containing vegetable oils as permeation enhancers. Sch. Res. Library 2, 84–98 (2010).
Limpongsa, E. & Umprayn, K. Preparation and evaluation of diltiazem hydrochloride diffusion-controlled transdermal delivery system. AAPS PharmSciTech 9, 464–470 (2008).
Yousuf, M., Ahmad, M., Usman, M. & Ali, I. Ketotifen fumarate and salbutamol sulphate combined transdermal patch formulations: In vitro release and Ex vivo permeation studies. Indian J. Pharm. Sci. 75, 569–577 (2013).
Ekenna, I. C. & Abali, S. O. Comparison of the use of kinetic model plots and DD solver software to evaluate the drug release from griseofulvin tablets. J. Drug Deliv. Ther. 12, 5–13 (2022).
Kaur, R., Arora, S. & Goswami, M. Formulation development and evaluation of Transdermal patch of Astaxanthin. Mater. Today Proc. https://doi.org/10.1016/j.matpr.2022.11.119 (2022).
Rajabalaya, R. et al. Design and in vitro evaluation of chlorpheniramine maleate from different eudragit based matrix patches: Effect of plasticizer and chemical enhancers. Ars Pharm. 50, 177–194 (2010).
Parhi, R. & Panchamukhi, T. RSM-based design and optimization of transdermal film of ondansetron HCl. J. Pharm. Innov. 15, 94–109 (2020).
Rhee, Y.-S. et al. Effects of vehicles and enhancers on transdermal delivery of clebopride. Arch. Pharm. Res. 30, 1155–1161 (2007).
Stimson, N. F. National Institutes of Health public access policy assistance: one library’s approach. J. Med. Library Assoc. JMLA 97, 238 (2009).
Rowe, R. C., Sheskey, P. & Quinn, M. Handbook of Pharmaceutical Excipients (Libros Digitales-Pharmaceutical Press, 2009).
Moreira, T. S. A., Pereira de Sousa, V. & Pierre, M. B. R. A novel transdermal delivery system for the anti-inflammatory lumiracoxib: influence of oleic acid on in vitro percutaneous absorption and in vivo potential cutaneous irritation. AAPS PharmSciTech 11, 621–629 (2010).
Prajapati, S. T., Patel, C. G. & Patel, C. N. Formulation and evaluation of transdermal patch of repaglinide. Int. Sch. Res. Notices 2011 (2011).
Takeda, H., Tsuji, M. & Matsumiya, T. Changes in head-dipping behavior in the hole-board test reflect the anxiogenic and/or anxiolytic state in mice. Eur. J. Pharmacol. 350, 21–29 (1998).
Seibenhener, M. L. & Wooten, M. C. Use of the open field maze to measure locomotor and anxiety-like behavior in mice. JoVE (J. Vis. Exp.) e52434 (2015).
Ishaq, H. Anxiolytic effect of herbal medicine, Khamira Gaozaban Ambri Jadwar Ood Salib Wala (KGJ) in Experimental Rat Models. Pak. J. Pharm. Sci. 27 (2014).
Mead, A., Li, M. & Kapur, S. Clozapine and olanzapine exhibit an intrinsic anxiolytic property in two conditioned fear paradigms: Contrast with haloperidol and chlordiazepoxide. Pharmacol. Biochem. Behav. 90, 551–562 (2008).
Ishaq, H., Javed, I., Tariq, T. & Mahmood, I. Antidepressant activity of the herbal extract, khamira gaozaban ambri jadwar ood salib wala. Int. J. Pharm. 3, 450–456 (2013).
Guitton, C., Kinowski, J.-M., Gomeni, R. & Bressolle, F. A Kinetic Model for Simultaneous Fit of Clozapine and Norclozapine Concentrations in Chronic Schizophrenic Patients during Long- Term Treatment. Clinical Drug Investigation 16, 35–43. https://doi.org/10.2165/00044011-199816010-00005 (1998).
Ravikrishna, V. & Krishnaveni, J. Development and evaluation of clozapine intranasal mucoadhesive in situ gels for brain targeting. J. Drug Deliv. Ther. 9, 198–207 (2019).
Abdulla, N. A., Balata, G. F., El-ghamry, H. A. & Gomaa, E. Intranasal delivery of Clozapine using nanoemulsion-based in-situ gels: An approach for bioavailability enhancement. Saudi Pharm. J. 29, 1466–1485. https://doi.org/10.1016/j.jsps.2021.11.006 (2021).
Yamamoto, S., Karashima, M., Arai, Y., Tohyama, K. & Amano, N. Prediction of human pharmacokinetic profile after transdermal drug application using excised human skin. J. Pharm. Sci. 106, 2787–2794. https://doi.org/10.1016/j.xphs.2017.03.003 (2017).
Acknowledgements
The authors thanks the Department of Pharmaceutics and Bioavailability and Bioequivalence Research facility for their support. Furthermore It’s an academic research work having no external funding
Author information
Authors and Affiliations
Contributions
AQ, SUJ, MHS, MS, RIY, and FRA conception and designed of the research study, data collection, data analysis, interpretation, and drafting of the manuscript. AQ, FS, AJM, GM, MTS, SM, MY and MA involved in the laboratory experimentation. All authors involved in reviewing the manuscript. All authors critically revised the paper and agree to be responsible for all aspects of the work. All author give agreement to publish this research.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qadir, A., Jan, S.U., Shoaib, M.H. et al. Formulation development and evaluation, in silico PBPK modeling and in vivo pharmacodynamic studies of clozapine matrix type transdermal patches. Sci Rep 15, 1204 (2025). https://doi.org/10.1038/s41598-024-81918-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-81918-6
Keywords
This article is cited by
-
Bioinspired Chitosan-Based Patches Enriched With Lipid-Casein Nanocarriers: An Innovative Approach for Wound Management and Evaluation in a Rat Model
Journal of Pharmaceutical Innovation (2025)
-
Formulation, characterization, and evaluation of transdermal patches of ranolazine for chronic angina pectoris
Naunyn-Schmiedeberg's Archives of Pharmacology (2025)