Abstract
Factor H (FH) is a negative regulator of the alternative pathway (AP) of complement however, five human factor H-related (FHR) proteins, can also function ex vivo as positive regulators. We compare bulk FH and FHR mRNA expressions in both the human rheumatoid arthritis (RA) synovium and blood cells from the Pathobiology of Early Arthritis Cohort (PEAC) and the Stratification of biological therapies for Rheumatoid Arthritis by Pathobiology (STRAP) Cohort. FH and FHR proteins were detected using multiplexed immunohistochemistry (MIHC) in synovium. In three pathotypes, in the synovium, no differences were found in the expression of FHR mRNA. In the synovium, a significant negative correlation was observed between FH expression and the disease activity score and X-ray joint space narrowing. In RA patients, there was a significant positive correlation between FHR3 mRNA level, anti-cyclic citrullinated peptide (CCP) antibodies and rheumatoid factor (RF). FHR proteins were co-localized in the synovial lining area along with complement C3 while FH was almost undetectable in the synovial lining but abundant in sub-synovial lining areas. We do not know whether FH and FHR proteins are locally generated and deposited in synovium or come from circulation. In sum, due to the absence of FH but the presence of FHRs, the synovial lining might fail to be protected from complement-mediated attack, and FHR3 may play a particularly important pathogenic role.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a lifelong chronic inflammatory autoimmune disease. The disease process primarily targets the synovium of the joints and affects approximately 0.24–1.0% of the world population1,2, with the prevalence among women higher than among men3. Early RA (eRA) of less than one year duration can be diagnosed in patients with inflammatory arthritis using serological biomarkers such as anti-citrullinated protein antibodies (ACPA aka anti-CCP) and rheumatoid factors (RF)4. Acute phase reactants such as C-reactive protein (CRP) levels and an elevated erythrocyte sedimentation rate (ESR) are also measured as inflammatory biomarkers in RA. Disease activity scores measured across 28 joints (DAS28) combined with ESR or CRP measures, i.e., DAS28-ESR and DAS28-CRP, are clinically validated tools to determine clinical activity and severity of the disease5,6. The etiology and pathology of RA are complex, and it is now known that the disease process is initiated many years before the development of clinically apparent arthritis and a diagnosis7.
The focus of this study is on the complement system and expression of activation pathway components as well as inhibitors in eRA and chronic RA, both in synovium and circulating blood cells i.e. PBMCs. It is well accepted that the complement system plays an important role in the development of experimental models of RA8,9. We have previously shown, using bulk RNA-sequencing, that many complement mRNAs are significantly expressed in the eRA synovium cell pathotypes compared with the blood cell pathotypes10. The expression of many complement genes such as C2, FCN1, FCN3, CFB, CFP, C3AR1, C5AR1, and CR1 were correlated with DAS28-ESR10.
Overall, the complement system is activated by three pathways, namely the classical pathway (CP), lectin pathway (LP) and alternative pathway (AP), and each plays a role in immune and inflammatory responses11,12,13. The activation of these three pathways leads to the sequential cleavage of the centrally important C3 and C5 complement proteins, resulting in the formation of a terminal membrane attack complex (MAC, aka C5b-9) and release of pro-inflammatory mediators14. Each pathway has unique components, and each pathway is controlled by different natural plasma and membrane-bound complement inhibitors. The AP activation components include C3, factor B (FB), and factor D (FD). In the AP, the central complement pathway protein C3 is cleaved by the C3 convertases, while C5 is cleaved by the amplification of C5 convertases15. C3 cleavage continues to ultimately produce C3a, C3b, iC3b, C3c, C3dg and other fragments, while FB is cleaved into Bb and Ba by FD16,17. The AP is specifically regulated by the major plasma protein factor H (FH). There is an inverse correlation between FH mRNA expression in the RA synovium with DAS28-ESR10, supporting an important role for a relative lack of FH control of the AP in RA complement-dependent inflammation and injury.
FH belongs to a protein family which includes factor H-like protein 1 (FHL1) and five factor H-related (FHR) proteins18 i.e., FHR1, FHR2, FHR3, FHR4, and FHR519, which were originally discovered using Western blot analysis by Zipfel and Skerka20. FHR proteins are mainly generated in the liver19, and their mRNA and protein detection in the eRA or RA synovium has not been explored in-depth, especially in relation to FH and levels of C3 activation. One study has shown that factor H family proteins such as FHL-1, FHR-1 and FHR-5, as well as the recombinant mini-FH, are able to bind to both monocytes and neutrophils21. FHR1 and FHR5 proteins have been shown to modulate opsonization through their interactions with DNA, dead cells and pentraxins22. FHL-1 protein is an alternatively spliced transcript of the FH gene, and FHR proteins are transcribed from separate genes but are structurally and antigenically similar to FH20.
The main role of FHR proteins, in contrast to FH, appears to be to enhance complement activation and opsonization, thus counter-balancing the inhibitory or regulatory effects of FH23. Relevant binding ligands of FH are C3b, C3c, C3d, heparin, sialic acid, and C-reactive protein (CRP), while FHR1 ligands are native C3, C3(H2O), C3b, Pentraxins, FP, extracellular matrix, apoptotic cells, and microbes23; FHR2 ligands are C3b and microbes23; FHR3 ligands are C3b, C3d, microbes and heparin18,23; FHR4 ligands are C3b, C3d, CRP, apoptotic cells, and microbes18,23; and FHR5 ligands are C3b, heparin, pentraxins, extracellular matrix, apoptotic cells, microbes and CRP18,23. Although studied ex vivo, it is not known which of these interactions are most relevant in vivo. It has been shown that FH and FHR gene mutations, polymorphisms and deletions are associated with many different human diseases including atypical hemolytic uremic syndrome (aHUS), C3 glomerulopathy (C3G), and age-related macular degeneration (AMD)18. No genetic linkage or rare mutation associations with RA have been reported. We have previously shown in eRA that FHR4 synovial mRNA expression at 6 months following treatment was positively correlated with the DAS28-ESR, suggesting its potential role in the development of worse therapeutic responses by promoting AP activation10. We have also evaluated the expression of mRNA encoding mouse FH, FHR-B, and FHR-C in various murine autoimmune disease models, including inflammatory arthritis, age-related macular degeneration and lupus and found that the mRNAs for CFH, CFHR-B and CFHR-C were universally present in the liver from mice with and without dense deposit disease, diabetes mellitus, basal laminar deposits, collagen antibody-induced arthritis24.
The liver also generates CRP protein after stimulation with IL-625, but it is also expressed by many other cell types such as lymphocytes, macrophages, and adipocytes26. CRP is a biomarker and regulator of systemic inflammation in RA27, and it is believed to play a role in bone destruction and disease progression in RA. There is a significant correlation between CRP serum levels and synovial inflammation in RA patients28. FHR4 that binds to pentameric CRP in the presence of calcium, and also binds and modifies FH, but independently of calcium29. Further studies have shown that FHR4 protein bound to native CRP activates the complement system30. FHR5 protein also binds to CRP31.
In this study, we examined, using MIHC imaging analysis, the presence of all five FHR proteins simultaneously along with FH, C3c, and MAC in the synovium from eRA patients. We also examined and analyzed bulk RNA-seq data from the PEAC (pathobiology of early arthritis cohort) clinical studies to assess in eRA patients the levels of mRNA expression from all five human FHR genes in synovium as well as from the cells of the blood in three different RA pathotypes namely lymphoid pathotype, myeloid pathotype and pauci immune32. FHR3 mRNA expression was also examined in the STRAP (Stratification of Biological Therapy for RA by Pathobiology) clinical study, i.e., in RA patients who failed treatment to Disease Modifying Anti-Rheumatic Drugs (DMARDs). In addition, we determined the correlations between five FHR mRNA expression and DAS28-CRP in eRA synovium. Gender-based differences in FHR and FH gene expression were examined. Finally, the variations in FHR mRNA expression in eRA were analyzed based on ACPA and RF status.
Materials and methods
General characteristics of synovial biopsies and blood from pathobiology of early arthritis cohort
To determine the levels of expression of mRNA encoded by all five FHR genes in three different pathotypes, we examined data from the PEAC study website (https://peac.hpc.qmul.ac.uk/) created by three of our coauthors32. Synovial biopsies (n = 87) and blood samples (n = 67) were obtained as previously detailed32. In the PEAC study, a total of 46 (51%) synovial biopsies were classified as lympho-myeloid (B cells, T cells, plasmacytoid, dendritic cells, NK cells), 21 (23%) as diffuse-myeloid (macrophage, basophil, eosinophil, neutrophil), 17 (19%) as pauci-immune fibroid (synoviocytes, few immune cells) and 6 (7%) as unclassified by histological analysis32. We also analyzed limited FHR mRNA expression data from another clinical trial, stratification of biological therapies for rheumatoid arthritis by pathobiology (STRAP) (n = 208) (https://r4ra.hpc.qmul.ac.uk/), in which synovial biopsies were obtained similarly using ultrasound but in patients who have failed prior DMARD treatment33. STRAP primary data is not publically available at this time. We have examined eRA synovial biopsies from PEAC (n = 23) for MIHC for various FHR proteins, FH, C3c, MAC (C5b-9), immune cells staining.
RNA extraction from synovial biopsies and blood, RNA sequencing, RNA-sequencing data processing
In PEAC clinical studies the RNA from synovial biopsies (n = 87) and blood PBMCs (n = 67) was extracted based on the published protocol by our coinvestigators32. Similarly, RNA from synovial biopsies was extracted in the STRAP study (n = 208)32. RNA was extracted from a minimum of 10 mg of synovial tissue homogenized at 4 °C in Trizol reagent (ThermoFisher Scientific, Invitrogen Division, UK). Chloroform was mixed with the lysate and following centrifugation the aqueous RNA layer was transferred to a new microcentrifuge tube. Isopropanol at 4 °C was mixed with the RNA layer. Following incubation and centrifugation, the isopropanol was removed and the RNA pellet washed with 70% ethanol. The pellet was re-dissolved in RNase-free water. Whole blood samples were preserved in RNALater solution (ThermoFisher Scientific, UK) (500µL whole blood: 1.3mL RNALater solution) and stored at − 80 °C prior to extraction. Blood samples in RNALater solution were thawed on ice and RNA prepared using the Ambion Ribo-Pure Blood kit (ThermoFisher Scientific, UK), as per the manufacturer’s instructions. The concentration of RNA samples was measured using the NanoDrop 2000 C (Lab Tech, UK).
For RNA sequencing 1 µg of total RNA was used for library preparation using TruSeq RNA Sample Preparation Kit v2 (Illumina). Generated libraries were amplified with 10 PCR cycles. The size of the libraries was confirmed using 2200 TapeStation and High Sensitivity D1K screen tape (Agilent Technologies). The libraries were first multiplexed (five per lane) and then sequenced on Illumina HiSeq2500 (Illumina) to generate 50 million of paired end 75 bp reads (154 samples) or 30 million single end 50 bp reads (10 samples).
For RNA-sequencing data processing transcript abundances and average transcript lengths were imported into R using Bioconductor package tximport 1.4.0 and summarized over NCBI RefSeq transcript isoforms. Imported abundances were normalized in R, including a correction for average transcript length and incorporating batch, sex, and pathotype as model covariates, using DESeq2 1.14.134. Transcript abundances underwent regularized log expression (RLE) transformation. The transcript abundances for the remaining synovium and blood samples were re-imported into R, normalized, and underwent RLE transformation followed by Principal components analysis (PCA) again to confirm homogeneity of each dataset. The quantification and statistical analysis of all of the RNA-sequencing data have been described in detail32.
Collection and processing of synovial biopsies from eRA subjects for MIHC of FHR proteins
We performed MIHC studies to analyze the expression of all five FHR proteins using synovial biopsies from eRA patients obtained in Accelerated Medicines Partnership® Rheumatoid Arthritis and Systemic Lupus Erythematosus (AMP® RA/SLE) studies10. The disease duration of eRA patients from which we obtained formalin-fixed paraffin-embedded (FFPE) synovial histology sections was less than 12 months. All eRA patients (male or female) from the AMP and PEAC clinical trials were tested for ACPA positivity, RF, and other blood markers. We also analyzed the presence of FHR proteins in some synovial biopsies from eRA patients (n = 9), which were collected locally by our team as a part of the Institutional Joint Biology Program (IJBP) at the University of Colorado Anschutz Medical Campus. Written ethical informed consent was obtained from all eRA patients according to the preapproved Colorado Multiple Institutional Review Board protocol (COMIRB # 20-1908 and 15-1389). All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols related to these studies were approved by the Institutional Review Board committee. Some of the synovial biopsies were used to standardize various complement protein antibodies (antigen retrieval, dilution, etc.) for FH and FHR proteins MIHC. Briefly, six to eight synovial biopsies (< 1–2 mm) from eRA patients (n = 9) were obtained using a needle (14 to 20 gauge) under local anesthesia from either the knee, ankle, wrist, and metacarpophalangeal (MCP) joints. These synovial biopsies were fixed in 10% neutral buffered formalin (NBF) and embedded in paraffin wax, followed by sectioning and staining with Hematoxylin and Eosin (H&E). FFPE synovial sections were processed for eight-color FHR1, FHR2, FHR3, FHR4, FHR5, FH, C3c, MAC (C5b-9), as well as for immune cells as well as macrophages and fibroblasts using MIHC staining followed by imaging analysis.
MIHC and multispectral fluorescence imaging for five FHR proteins from synovial biopsies from the joints of eRA subjects
Prior to MIHC analysis, using AMP synovial biopsies for histopathology, one section from each eRA synovial biopsy was used for examining their quality regarding the presence or absence of damage of the synovial lining and sub-synovial areas or other artifacts such necrosis or excessive fat tissue, etc. For histopathology and structural integrity, synovial sections were also stained using H&E followed by examination under the light microscope by a pathologist. For MIHC, we used the antibodies described below as well as antigen retrieval (AR) procedures to detect various FHR proteins.
FHR1, FHR2, FHR3, FHR4, FHR5, FH, C3c and MAC protein positive staining were measured in synovial cells by MIHC. Synovial sections from eRA patients. Through our collaboration with the Human Immune Monitoring Shared Resource (HIMSR) at the University of Colorado School of Medicine we performed multispectral imaging using the PhenoImager HT instrument (formerly Vectra Polaris, Akoya Biosciences). To quantify percentage of positive cells of human FHR1, FHR2, FHR3, FHR4, FHR5, FH, MAC/C5b-9 and C3c FFPE eRA synovial sections were stained consecutively with specific primary antibodies for FHR1 (dilution 1:100, Opal 690) (Abcam, Waltham, MA): FHR2 (dilution 1:100, Opal 480) (LifeSpan BioSciences); FHR3 (dilution 1:50, Opal 570) (Antibodies-online, Limerick PA); FHR4 (dilution 1:400, Opal 650) (Gift from Dr. Paul Morgan, UK); FHR5 (dilution 1:500, Opal 620) (abcam); FH (dilution 1:200, Opal 540) (Abcam); Mac/C5b-9 (dilution 1:500, Opal 520) (Abcam) and C3c (dilution 1:800, Opal 780) (LifeSpan BioSciences). Opal is a fluorochrome product (Akoya Biosciences, Marlborough, MA). The Opal dilution used for all markers was 1:150 except C3c and it was 1:25. We used 300 µl of the diluted fluorochrome solution, in two consecutive 150 µl injections. Briefly, the slides with eRA synovial section were deparaffinized, heat treated (94° for 20 min) in antigen retrieval buffer (Leica ER1 or ER2), blocked (Antibody Diluent, Akoya Biosciences), and incubated with primary antibodies as mentioned above, followed by horseradish peroxidase (HRP)-conjugated secondary antibody polymer (Anti-Rabbit/Anti-Mouse Polymer, Akoya Biosciences), and HRP-reactive Opal fluorescent reagents (Akoya Biosciences). Opal reagent was used to detect multiple markers in a single eRA synovial biopsy section. The slides were stripped between each stain with heat treatment in antigen retrieval buffer. The antigen retrieval buffers used for CFHR1 and CFHR5 were Leica ER2 buffer (pH9), while all other markers received AR in Leica ER1 buffer (pH6). Spectral DAPI (Akoya Biosciences) was applied after the completion of the final antibody staining step and slides were cover slipped with ProLong Diamond mounting media (ThermoFisher). Whole slide scans were collected with PhenoImager HT v2.0.0 software using the 20 × objective with a 0.5 μm resolution. Regions of interest were selected and re-scanned using the 20 × objective and the multispectral imaging cube. Spectral references and unstained control images were measured and inForm software v3.0 was used to create a multispectral library reference. To detect cell nuclei in synovium 4′,6-diamidino-2-phenylindole (DAPI) was used. After MIHC staining, whole slide scans of the synovial biopsies were imaged.
Multispectral imaging to quantify cells expressing FHR proteins
To quantify the percentage of single or double positive synovial cells expressing various FHR proteins, FH, C3c, and MAC (C5b-9), we performed multispectral imaging using the PhenoImager HT 9-color instrument (formerly Vectra Polaris, Akoya Biosciences). To quantify levels of FHR, FH, C3c and MAC, FFPE eRA synovial sections were stained consecutively with specific primary antibodies for FHR proteins, FH, C3c and MAC as mentioned above. Briefly, the slides were deparaffinized, heat treated in antigen retrieval buffer, blocked, and incubated with primary antibodies, followed by horseradish peroxidase (HRP)-conjugated secondary antibody polymer, and HRP-reactive OPAL fluorescent reagents. The slides were stripped between each stain with heat treatment in antigen retrieval buffer. As mentioned above, the whole slide scans were collected with PhenoImager HT v2.0.0 software. Some sections were also scanned using 40x objective for better and more detailed images. Imaging analysis of the synovial sections was done blindly. The multispectral images (.im3 files) were spectrally unmixed and analyzed with tissue segmentation, cell segmentation, and phenotyping using inForm software v3.0 (Akoya Biosciences). Data were compiled and summarized using PhenoptrReports (Akoya Biosciences).
MIHC, imaging analysis and quantification of eRA synovium for macrophages and fibroblasts
The presence of macrophages and fibroblasts in the synovial biopsies from eRA MIHC was used according to our previously published protocol35,36. Here, FPPE synovial biopsy sections from each eRA patient were used in duplicate. To quantify percentage of positive cells of human FHR1, FHR2, FHR3, FHR4, FHR5, FH, FAP and CD68 FFPE eRA synovial sections were stained consecutively with specific primary antibodies for FHR1 (dilution 1:100, Opal 690) (Abcam, Waltham, MA ): FHR2 (dilution 1:100, Opal 480)(LifeSpan BioSciences, Lynnwood, WA); FHR3 (dilution 1:50, Opal 570) (Antibodies-online, Limerick PA); FHR4 (dilution 1:400, Opal 650) (Gift from Dr. Paul Morgan, UK); FHR5 (dilution 1:500, Opal 620)(abcam); FH (dilution 1:200, Opal 540) (Abcam); FAP (fibroblast associated protein) (dilution 1:100, Opal 520) (Abcam) and CD68 (dilution 1:500, Opal 780) (Dako). The Opal dilution used for all markers was 1:150 except CD68 and it was 1:25. Briefly, the slides with eRA synovial section were deparaffinized, heat treated (94° for 20 min) in antigen retrieval buffer (Leica ER1 or ER2), blocked (Antibody Diluent, Akoya Biosciences), and incubated with primary antibodies as mentioned above, followed by horseradish peroxidase (HRP)-conjugated secondary antibody polymer (Anti-Rabbit/Anti-Mouse Polymer, Akoya Biosciences), and HRP-reactive Opal fluorescent reagents (Akoya Biosciences). Opal reagent usestyramide signal amplification (TSA), allowing the detection of multiple markers in a single eRA synovial biopsy section. The slides were stripped between each stain with heat treatment in antigen retrieval buffer. Spectral DAPI (Akoya Biosciences) was applied after the completion of the final antibody staining step and slides were cover slipped with ProLong Diamond mounting media (ThermoFisher). Whole slide scans were collected with PhenoImager HT v2.0.0 software using the 20 × objective. As mentioned above spectral references and unstained control images were measured and inForm software v3.0 was used to create a multispectral library reference. In parallel, human tonsils were used as a positive control for macrophage and fibroblast analysis. For quantification, multiple composite images from each eRA synovial biopsy were generated along with individual staining for complete analysis of macrophages and fibroblasts. The 9-color images were analyzed with inForm software V3 (Akoya Biosciences) to unmix adjacent fluorochromes, subtract autofluorescence, segment the tissue, segment cellular membrane, cytoplasm, and nuclear compartments, and identify positive and negative cells for each marker according to morphology and cell marker expression. The algorithm was applied to all images in the project, exported as .txt files, and Phenoptr Reports (Akoya Biosciences) was used to merge the data from all fields and all markers into one file. Phenoptr Reports was then used to identify cells expressing combinations of markers, calculate cell percentages and densities, and summarize the data by slide ID.
Analysis of FHR gene expression from eRA and RA synovial biopsies
We datamined the PEAC database to explore mRNA expression encoded by FHR1, FHR2, FHR3, FHR4, and FHR5 in three cell pathotypes (lymphoid, myeloid, and fibroid) and their correlations with DAS28-CRP in the synovial and blood cell pathotypes from eRA patients (n = 87), integrated with deep phenotypic profiling32. In this study, we compared bulk RNA-seq gene expression for all FHR proteins from male and female eRA subjects. The levels of expression of FHR and FH mRNA were also compared based on the anti-CCP (aka ACPA) and RF positive and negative status in eRA subjects. We also analyzed data related to FHR3 mRNA expression and its relationship to DAS28-CRP from the STRAP trial33 The relationship between FHR3 expression and anti-CCP or RF status was also examined in the late stage of the disease. The RF status is positive if anti-CCP > = 10 and if RF > = 20.
Statistical analyses
All data relating to the percentage of synovial cells expressing various FHR proteins, FH, macrophages, and fibroblasts from MIHC studies were analysed using student t-tests using the GraphPad Prism program. P-values shown on the pathotype boxplots of the PEAC study were derived from ANOVA using the Volcano3D R package (v2.0.7). The correlation plots between baseline expression of PEAC synovium and baseline DAS28-CRP (Spearman’s correlation), as well as correlations between FHR3 and CCP or RF, are shown.
Results
Presence of FHR proteins in synovial biopsies from eRA patients
Synovial biopsies were examined using MIHC for the presence of all five human FHR proteins as well as FH, C3c, and MAC (C5b-9) (Fig. 1). We found that all five FHR proteins were expressed in synovial cells (Fig. 1A, B). The composite image shown confirms that FHR1, FHR2, FHR3, FHR4, and FHR5 proteins are present in the synovium with individual FHR shown using a pseudo color-coding scheme (Fig. 1). The presence of FHR1, FHR2, FHR3, FHR4, and FHR5 is shown in magenta, white, green, pink and yellow colors, respectively (Fig. 1A, B). All eRA and chronic RA samples showed the presence of the FHR proteins. The presence of FH, C3c and MAC is shown in cyan, red and orange colors, respectively (Fig. 1A). All individual positive control staining patterns in the synovium for FHR1, FHR2, FHR3, FHR4, FHR5, C3c, FH and MAC (C5b-9) proteins have been shown (Supplemental Fig. 1B, 1 C, 1D, 1E, 1 F,1G, 1 H, 1I).
A representative composite image from nine eRA synovial samples generated after MIHC showing the presence of all five human FHR proteins along with complement component C3c and membrane attack complex (a.k.a. C5b-9). A The presence of FHR1 (magenta color), FHR2 (white color), FHR3 (green color), FHR4 (pink color), FHR5 (yellow color), FH (cyan color), C3c (red color) and MAC (C5b-9) (orange color) has been shown in the synovial biopsies. B FHR2 and FHR3 compared with FH dominantly present in the synovial lining of synovial biopsies. A false color-coding key was used for each complement protein shown in this composite image. Adipocytes = black cobble-like stone cells in the synovium. A minimum of three to five composite images were generated using a single synovial biopsy with 2 sections from each patient. eRA synovial biopsies n = 9. Magnification = × 40. Scale bar = 100 μm. *p < 0.05.
All FHR proteins are present and expressed by various cells in the synovial lining as well as in the sub-synovial lining areas. Specifically, compared with FH, FHR2 and FHR3 were predominantly present in the synovial lining (Fig. 1A, B). FH was undetectable in synovial lining as compared to the sub-synovial lining area (Fig. 1A, B). In this composite image, FHR4 (pink color), and FH (cyan color) were predominately expressed by the synovial cells present in the sub-synovial lining area (Fig. 1). In contrast C3c (red color) was predominately found in cells present in the synovial lining (Fig. 1A). The pattern of expression of FH, as well as five FHR proteins, in the synovial cells suggests that there is local regional regulation and counter-regulation, respectively, of the AP in the synovial microenvironment.
Quantitative measurements of FHR proteins in the synovial cells from eRA patients
The composite images after MIHC were used to quantify the percentage of synovial cells positive for individual FHR proteins in eRA synovial biopsies (Fig. 2). Surprisingly, FHR2 and FHR3 proteins were present the synovial cells in the synovial lining and in the sub-synovial area. FHR2 protein was present significantly higher in the synovial cells compared with FHR1 (p < 0.037), FHR4 (p < 0.0039) and FHR5 (p < 0.0012) (Fig. 2A). FH protein was also present significantly at a higher level in the synovial cells than FHR1 (p < 0.0017), FHR4 (0.00012), and FHR5 (p < 0.000039) (Fig. 2A). C3c protein was present significantly (p < 0.05) higher than FHR1, FHR2, FHR3, FHR4, FHR5, FH and MAC (C5b-9) (Fig. 2A). The percentage of synovial cells positive for both FHR2/C3c, FHR4/C3c and FHR5/C3c was significantly lower than FHR3/C3c (Fig. 2B). There were no differences in the synovial cells stained for C3c/MAC and C3c/FH (Fig. 2B). But the correlation between C3c and MAC positive synovial cells was positive (r = 0.83, p < 0.0092). The correlation between C3c and FHR2 and FHR3 were negative and non-significant (r − 0.73, p < 0.069; r = − 0.49, p < 0.20 respectively). These data show that synovial cells are differentially and highly positive for FHR2 and FHR3, in addition to the presence of FH and C3c proteins in abundance. The data we have shown might represent both extra cellular and intracellular stores.
Showing percentage of FHR, FH, C3c and MAC single and double positive synovial cells in the synovium from eRA patients. MIHC was used to generate composite images followed by quantitation of single and double positive cells showing the presence of FHR1, FHR2, FHR3, FHR4, FHR5, FH, C3c, and MAC. A Presence of single positive synovial cells expressing FHR1, FHR2, FHR3, FHR4, FHR5, FH, C3c, and MAC. B Presence of double positive synovial cells positively stained for proteins FHR1/C3c, FHR2/C3, FHR3/C3, FHR4/C4, FHR5/C3c, FH/C3c and MAC/C3c. Synovial cells expressed a lower level of FHR1, FHR4, FHR5 and MAC. eRA synovial biopsies n = 8. Data are shown as mean ± SEM. *p < 0.05 considered significant.
Expression of FHR proteins in synovial macrophages and fibroblasts
We next determined using MIHC the presence of all five FHR and FH in synovial macrophages and synovial fibroblasts. Again, we used composite images after 9-color MIHC staining (Fig. 3). As mentioned above, all FHR proteins and FH protein were present in the synovium (Fig. 3A). The macrophages (red color) and fibroblasts (orange color) were present predominately in the synovial lining of eRA patients (Fig. 3). It was noted that the synovial macrophages and synovial fibroblasts were largely co-located in the synovial lining in eRA and chronic RA samples. Nonetheless chronic RA biopsies have both these cell types in abundance in the multilayer synovial lining. In the sub-synovial lining area, many synovial cells predominantly expressed FHR3 (Fig. 3B). These data show that synovial macrophages and synovial fibroblasts also expressed specific FHR proteins and FH.
A representative composite image from eight synovial samples showing the presence of macrophages and fibroblasts expressing FHR proteins in eRA patients. A Synovial cells showing the presence of FHR1 (magenta color), FHR2 (white color), FHR3 (green color), FHR4 (pink color), FHR5 (yellow color), FH (cyan color), DAPI (blue), macrophages (red color) and fibroblasts (orange color). B Synovium cells showing the predominance of FHR3 (green color) in the sub synovial lining area. A false color-coding key was used for each complement protein, macrophages and fibroblasts shown in this composite image. Adipocytes = black cobble-like stone cells in synovium. A minimum of three to five composite images were generated using a single synovial biopsy with 2 sections from each patient. Magnification = × 40. eRA synovial biopsies n = 8. Scale bar = 100 μm.
Quantitative measurements of synovial macrophages and fibroblasts stained for FHR proteins in the synovial biopsies from eRA patients
We determined the percentage of synovial macrophages and synovial fibroblasts from composite images positive for individual FHR proteins in the synovial biopsies from eRA patients (Fig. 4). Synovial macrophages expressed significantly higher levels of FHR2 compared to FHR1 (p < 0.018), FHR4 (p < 0.0009) and FHR5 (p < 0.0010) (Fig. 4A). Similarly synovial macrophages expressed significantly higher levels of FHR3 compared to FHR1 (p < 0.041), FHR4 (p < 0.0074) and FHR5 (p < 0.0074) (Fig. 4A). In contrast synovial fibroblasts have significantly higher levels of FHR2 compared to FHR1 (p < 0.017), FHR3 (p < 0.005), FHR4 (p < 0.004) and FHR5 (p < 0.008) (Fig. 4B). FHR1, FHR3, FHR4, and FHR5 were almost undetectable in contrast to FHR2 in the synovial fibroblasts (Fig. 4B). Interestingly, 17% of the synovial cells other than macrophages and fibroblasts were positive for FHR3 (data not shown), though the identity of these cells remains unknown. All of these data show that specific synovial cells are differentially positive for specific FHR proteins in the synovium from eRA patients.
Bar graphs show the presence of macrophages and fibroblasts positive for individual FHR proteins in the synovium from eRA patients. MIHC composite images were analyzed for the presence of percentages of synovial macrophages (CD68 positive) and fibroblasts (FAP) positive for FHR1, FHR2, FHR3, FHR4 and FHR5 proteins. A Percentage of macrophages positive for FHR1, FHR2, FHR3, FHR4 and FHR5 proteins. B Percentage of fibroblasts positive for FHR1, FHR2, FHR3, FHR4 and FHR5 proteins. Both macrophages and fibroblasts have a low level of FHR1, FHR4 and FHR5 proteins compared with FHR2 and FHR3 proteins. eRA synovial biopsies n = 8. Data are shown as mean ± SEM. *p < 0.05 considered significant.
Regional localization of FHR proteins in the synovium from eRA patients
To further explore and quantitate differences in regional localization, we examined synovial biopsies from eRA patients composite images after MIHC for levels of various FHR proteins along with FH (Fig. 5). After scanning many synovial composite images using MIHC, we found that there was a clear and distinct regional localization and colocalization of some FHR and FH proteins (Fig. 5). For example, FHR2 (white color) protein was not only predominately present in the synovial lining but it was also present in the sub-synovial lining areas (Fig. 5A, B). Although FH (cyan color) was rarely present in the synovial lining, and was abundantly present in the sub-synovial areas, FHR2 protein could occasionally be localized with FH protein in the synovial lining (Fig. 5A, B). FHR4 (pink color) protein was present in cells in the sub-synovial lining area (Fig. 5C). Rarely FHR1, FHR2 and FHR4 were also co-localized in the sub-synovial lining area (Fig. 5D). There was distinct regional localization/and or distribution of C3c (red color) and FH (cyan color) in the synovial lining and sub-synovial lining areas, respectively (Fig. 5D). These data related to the localization of FHR along with FH and C3c further show that there is pronounced regional alteration in the localization of FHR proteins in the synovium from eRA patients.
Representative snapshots of MIHC composite images showing the regional and differential distribution of FHR proteins in the synovial biopsies from eRA patients. A Composite image showing coexistence of FHR2/FH in the synovial lining but coexistent of FHR5/FH in the sub synovial lining area. B FH is predominately present in the sub synovial lining area, not in the synovial lining area. C FHR1 and FHR4 proteins are positively stained in cells in the synovial lining area. FHR3 is also present in the sub-synovial lining areas. D C3c is predominately and constantly present in the synovial lining cells. The coexistence of FHR1, FHR2, and FHR4 was also noticed in the sub-synovial lining areas. A false color-coding key represents FHR1 = magenta, FHR2 = white, FHR3 = green, FHR4 = pink, FHR5 = yellow, C3c = red, FH = cyan and DAPI = blue. SL = synovial lining. SSL = sub synovial lining Magnification = × 40. eRA synovial biopsies n = 4. Scale bar = 100 μm.
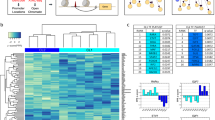
Gene expression of FHR in three different pathotypes in synovium and blood from eRA patients
We also analyzed and compared the bulk RNA-seq data, generated in the PEAC study, based on specific pathotypes (lymphoid, myeloid and fibroid) for baseline gene expression of FHR1, FHR2, FHR3, FHR4 and FHR5 in synovium and in the blood from eRA patients (Supplemental Fig. 2). Although the trends of FHR1 and FHR3 gene expression in the synovium were higher in the myeloid pathotype, these were not statistically significant (Supplemental Fig. 2A & B). The mRNA expression from FHR2 was not detected in the original database from the PEAC clinical study. In the blood, the mRNA expression of FHR1, FHR3, and FHR4 was also not different in the three pathotypes (Supplemental Fig. 2E, 2 F, 2G). The negative scale numbers indicate low RNA counts. There was no detection of FHR5 mRNA expression in either of the three pathotypes in the blood due to negative numbers (Supplemental Fig. 2H). Overall, these data show that all three synovial or blood cell pathotypes, i.e., lymphoid, myeloid, and fibroid, transcribed FHR1, FHR3, and FHR4 mRNA equally.
Gender-based differences in +FHR and FH expression in eRA
We analyzed gene expression data related to the expression of FHR and FH in males and females in the synovium and blood from eRA patients (Supplemental Fig. 3). There were no significant differences in the expression of FHR1, FHR3, FHR4, FHR5, and FH both in synovium and in blood in both genders (Supplemental Fig. 3). However, in the synovium, in females, non-significant higher trends in gene expression of FHR1 and FHR3 were noticed (Supplemental Fig. 3A, 3B). In contrast, in blood, in males, non-significant higher trends in gene expression of FHR1 and FHR4 were noticed (Supplemental Fig. 3F, 3 H). These data show that, based on gender, there were no significant differences in the gene expression of FHR and FH in synovium or in blood cells in the eRA population.
Correlation between FHR3 gene expression and ACPA and RF in the STRAP clinical trial
In RA synovium, there were positive and significant correlations between the expression of FHR3 and RF (r = 0.14, p = 0.038) and FHR3 and anti-CCP (r = 0.17, p = 0.015) (Fig. 6A, B). These correlation data suggest that some FHR proteins may be associated with increased pathogenic during the evolution of RA.
Correlations between FHR3, RF, and anti-CCP in the synovium from RA patients from STRAP clinical trial. A Positive and significant correlation between FHR3 gene expression and RF autoantibodies. B Positive and significant correlation between FHR3 gene expression and anti-CCP autoantibodies. RF rheumatoid factor antibody. CCP anti-cyclic citrullinated peptide antibody. STRAP n = 208. Correlation = r and *p < 0.05 are considered significant.
Correlation between FHR, and FH gene expression with X-ray erosion and joint space narrowing
Radiographic joint destruction in RA is measured by the Sharp/van der Heijde scoring method37 and the Genant-modified Sharp score (GSS) is normally used to measure joint space narrowing for RA patients38. We found, in RA synovium from the STRAP study, there were no significant correlations between FHR3 expression and X-ray erosions (r = 0.042 p = 0.58) (Fig. 7A) and FHR3 and X-ray joint space narrowing (r = − 0.089, p = 0.24) (Fig. 7B). The correlations between FH and X-ray erosion was negative and non-significant (r = − 0.18, p = 0.13) (Fig. 7C) but the correlation between FH and X-ray joint space narrow was negative but significant (r = − 0.23, p = 0.05) (Fig. 7D).
Correlations between FHR3, X-ray erosion, and X-ray joint space narrowing from the STRAP clinical trial. A No correlation between FHR3 mRNA expression and X-ray erosion in RA patients. B No correlation between FHR3 mRNA expression and X-ray joint space narrowing in RA patients. C No correlation between FH mRNA expression and X-ray erosion in RA patients. D A negative and significant correlation between FH mRNA expression and X-ray joint space narrowing in RA patients. X-ray erosion = radiographically (X-ray) demonstrable bone erosion in RA. X-ray joint space narrowing = radiographs (X-ray) used to manually measure and quantify joint space to determine the severity of RA. STRAP n = 208. Correlation = r and *p < 0.05 are considered significant.
Correlations between FHR and DAS28-CRP in the synovium from eRA patients
To explore the correlation between FHR mRNA expression and DAS28-CRP, a marker for inflammation in the body, we examined the correlation in the synovium and blood from eRA patients (Supplementary Figure. 4). While all the correlations between DAS28-CRP and FHR1 (r = 0.077, p = 0.51), FHR3 (r = 0.01, p = 0.93), FHR4 (r = 0.051, p = 0.65) and FHR5 (r = 0.23, p = 0.84) in synovium were positive, they were not significant (Supplementary Figure. 4 A, 4 C, 4E & 4G). Similarly, only weak positive trends in correlations between DAS28-CRP and FHR1 (r = 0.02, p = 0.88), FHR3 (r = 0.28 p = 0.033), and FHR4 (r = 0.01, p = 0.94) in blood cells gene expression were noticed, but these correlations were also not significant (Supplementary Fig. 4B, 4D, 4 F). As mentioned above, FHR2 mRNA expression was not detected in the synovium or in the blood cells. FHR4/5 are expressed at very low levels in the synovium and FHR1/3/4 are expressed at very low levels in the blood. However, FHR5 mRNA expression in blood was undetectable in contrast to the synovium in eRA patients (Supplementary Fig. 4G, 4 H). In contrast, in the synovium there was again a negative significant correlation between FH mRNA levels and DAS28-CRP (r = − 0.32, p = 0.0037) (Supplementary Fig. 5A). In contrast, in blood there was a positive and non-significant correlation (r = 0.11, p = 0.42) between FH and DAS28-CRP (Supplementary Fig. 5B). The lack of correlations between FHR expression and DAS28-CRP show that DAS28-CRP and FHR expression are likely not dependent on each other. FHR proteins may not be directly related to inflammation or clinical disease score activity, or their effects might be independent and focused on regional complement dysregulation. In contrast, FH expression decreases with increasing DAS28-CRP, indicating inflammation or disease activity score increases with the decrease in FH expression, confirming the likely regulatory role of local produced FH in inflammation specifically in the joints.
FHR and FH mRNA expression based on anticyclic citrullinated protein antibodies status
Based on anti-cyclic citrullinated protein antibodies (anti-CCP) positive and negative status, no significant differences were noticed in expression of FHR1, FHR3, FHR4, and FHR5, mRNAs in the synovium as well as in blood from eRA patients (Supplementary Fig. 6). In synovium, FHR4 and FHR5, while in blood, FHR1 and FHR3 were below detection limits both in anti-CCP positive and negative subjects (Supplementary Fig. 6C, 6D, 6E, 6 F). These data show that the presence or absence of the anti-CCP autoantibodies, which develop during eRA, have no relationship to bulk mRNA expression of FHR1, FHR3, FHR4, FHR5, and FH mRNA in the synovium and blood cells locally or systemically.
FHR and FH mRNA expression based on rheumatoid factor status
We found that based on RF positive and negative status, there were no significant differences in the expression of FHR1, FHR3, FHR4, and FHR5 mRNAs in the synovium as well as in blood from eRA patients (Supplementary Fig. 7). The expressions of FHR4 and FHR5 mRNAs were below the detection limits in the eRA synovium, while FHR1, FHR3, and FHR4 mRNA levels were below the detection limits in the blood (Supplementary Fig. 7C, 7D, 7E, 7 F). Again, the presence or absence of RF does not exhibit a relationship to the bulk mRNA expression by FHRs.
Discussion
In this study we utilized paired synovial and blood (PBMCs) samples collected via the PEAC, STRAP and AMP® RA/SLE clinical studies10,32,39,40,41 to measure proteins associated with the complement system, including C3 fragments, MAC components, FH, and members of the FHR family. We then utilized clinical data including DAS28-CRP, ACPA, RF, and gender as well as gene expression data to perform bioinformatic analyses and evaluate correlations with disease32,39,40. We found C3 protein to be primarily located within the synovial lining, with a subset of these cells also containing MAC proteins. FH protein positive staining was mostly limited to cells of the sub-synovial lining. Members of the FHR family were widely distributed among cells of the RA joint including the intimal and sub-intimal areas of the synovial lining. In eRA synovium, immune cells such as synovial macrophages and synovial fibroblasts differentially expressed FHR2 and FHR3 proteins, respectively.
The presence of all five FHR proteins along with FH, C3c, and MAC (C5b-9) in the synovium from eRA patients’ knee joints confirms that there is complement activation and likely ongoing counter-regulation of the AP pathway locally in the knee joints. C3c was present in abundance in the synovial lining, which was consistent with previous reports10. Importantly, our data shows that FH was relatively absent from cells of the synovial lining, predominantly being present in the sub-synovial lining area, while FHR proteins were distributed throughout this region. Of these, FHR1 and FHR2 proteins were the major constituents. This type of regional distribution of FHR proteins and FH likely controls the spatial distribution of C3 fragment deposition present in the RA synovium. Since activating FHR proteins compete with inhibitory FH for control of C3, the lack of colocalization of FHR along with FH in synovial lining cells is surprising and suggests that at the very early stages of the disease, activating forces predominate specifically within synovium, and FHR proteins are present to keep FH from controlling this state. We hypothesize that the synovial lining is susceptible to complement-mediated attack because it has less protection by natural inhibitory proteins. Thus, the balance between complement regulators and activators in eRA is lost on the synovial membrane, which leads to dysregulation of the AP on the synovial lining where the disease might initiate.
Normally, FH binds to C3b and sialic acid present on the surface of cells. Thus, if C3b or sialic acid abundance is diminished or absent, then that could dampen FH binding. However, we found C3c to be abundant in the synovial lining which must be derived from abundant C3b and iC3b. This would rule against the lack of complement C3 protein and favor the hypothesis that lack of FH is due to a lack of sialic acid. A membrane-bound enzyme, β-galactoside α2,6-sialyltransferase 1 (ST6Gal1), controls the addition of α2,6-linked sialic acids to the termini of glycans, and it is expressed in many tissues42. This enzyme is related to the transport of sialic acid, and we found that the fibroid pathotype (pauci immune pathotype) has significantly (p = 0.000000026) less ST6Gal1 expression than the lymphoid pathotype (data not shown). Studies have also shown that the reduction of α2,6-sialylation is emblematic of the inflammatory status of synovial fibroblasts in RA43. In this study, it has been shown that the transformation of fibroblasts into pro-inflammatory cells is associated with glycan remodeling. This process involves TNF-α-dependent inhibition of the glycosyltransferase ST6Gal1 and α2–6 sialylation43. Other studies have shown that RA is associated with the reduction of cell-surface sialylation of synovial fibroblasts44. We noticed that FHR1 and FHR2 are present on the synovial lining in the absence of FH (Fig. 3). FHR2 binds to C3b and allows C3 convertase formation but FHR2 bound C3 convertases do not cleave the C3 substrate45. It has been shown that in contrast with FH, FHR-1 lacks the capacity to bind sialic acids, which prevents C3b-binding competition between FH and FHR-1 in host-cell surfaces46. While it might seem that FHR1 antagonizes FH47,48,49 by out competing with FH for binding to sialic acid, FHR1 sialic acid binding sites were shown to be inactive46; therefore, this should not be a possibility. Additionally, we hypothesize that sialic acid levels are diminished in RA tissue due to low levels of ST6Gal1. Alternatively, FHR might be binding to necrotic tissue or damaged cells50 present in the synovial lining and in the sub-synovial lining area, however, we have not seen necrotic cells in the eRA synovium lining under a light microscopic investigation. It has been shown that FH selectively inactivates C3b bound to surfaces bearing host-specific polyanions such as heparan sulfate, therefore limiting complement activation on self surfaces such as the glomerular basement membrane, which are not protected by cell-bound complement regulators51. We have not examined the presence of heparan sulphate on the synovial lining. Nonetheless the FH-C3b interaction has been shown to be enhanced by surface glycosaminoglycans and the FH-glycosaminoglycans interaction is also well known52. It has been shown that the due to FHR-5-surface glycosaminoglycans interaction the ability of FHR-5 to prevent binding of FH to surface C3b is enhanced by surface kidney heparan sulfate52. It has also been shown that the absence of intrinsic FH alters gene expression in cultured kidney endothelial cells and upregulation of genes is involved in inflammation and complement system53. We don’t rule out the possibility that there is upregulation of other FHR genes involved in inflammation in the synovial lining, and these could downstream remodel the synovial microenvironment. Thus, the reason for the presence of FHR proteins in the synovial lining and the absence of FH remains unexplained. It has been shown by using ELISA that FH is present approximately four times less based on the graph scales in the synovial fluid in the RA joints than in the RA serum54. Therefore, FH is not evenly distributed locally vs. systemically54. Thus, there might be a threshold of FH to protect the synovial lining, and due to the presence of FHR proteins, FH failed to protect the synovial lining. Interestingly, it has been shown that FH plays an important role in anti-angiogenesis in synovium55,56. The distribution of FH within the synovial tissues might play a role in the angiogenic process seen in RA joint tissue. Angiogenesis and synovial hyperplasia are the pathological characteristics of RA.
Bone erosion in RA is normally measured using X-rays, and joint space narrowing is a symptom of structural deterioration. In the more advanced stage of the disease, there were positive and highly significant correlations between FHR3 expression and ACPA, RF, but not with X-ray erosions, and X-ray joint space narrowing. A negative and significant correlation between FH expression and X-ray joint space narrowing confirms that FH might be playing a protective role in contrast to FHR3 which increases during the evolution of disease and contributes to pathogenesis in chronic RA. No significant differences were seen in the eRA synovium and in blood in the gene expression of FHR1, FHR3, FHR4, and FHR5 in three different pathotypes, i.e., lymphoid, myeloid, and fibroid (Fig. 6), although myeloid pathotype showed increased trends of FHR1 and FHR3 in the synovium. In contrast, we have demonstrated that FH gene expression was highest in the fibroid pathotype vs. lymphoid and myeloid pathotypes10, with the understanding it might be protecting the fibroid pathotype in eRA from AP activation because the expression of FB was suppressed in this pathotype10. A low expression of TNF has been previously reported in the fibroid pathotype in contrast to lymphoid and myeloid pathotypes in eRA32. Our observation regarding a high expression of FH in fibroid pathotype was consistent with the published studies that FH protected TNF-α-induced inflammation by upregulating EIF3C (eukaryotic translation initiation factor 3 subunit C) in FLS54 confirming anti-inflammatory role of FH in eRA. We noticed that although FHR2 protein was present in the synovium from eRA patients, its gene expression was not found in the PEAC synovial tissue or blood databases32. Interestingly, FHR2 gene expression was also missing from AMP/RA/SLE Network database57, indicating both studies used 10 × Genomics platform, single data source, sequencing platform, and quality control tools. In contrast FHR5 gene expression was present in the synovium but not detected in cells of the blood indicating a more localized expression pattern for this gene. We rule out the possibility of degradation of mRNA for already lower levels of FHR5 proteins in two different independent well controlled studies.
The correlations between DAS28-CRP and FH were negative and significant (Supplementary Fig. 5). FH has been shown to bind to CRP proteins to reduce its proinflammatory activity58. Therefore, FH might be dampening CRP locally to reduce inflammation. CRP is a well-known serum biomarker of chronic inflammation in heart disease, and its role in AMD has also been documented59,60,61. We speculate regardless of how much FH is present in the eRA synovium, the increasing trend in the expression of FHR and CRP might be disturbing the site-specific regulation of AP in the synovium. Nonetheless, FHR, FH, and CRP might play independent roles in inflammation and also interacting with each other independently to activate the complement system in eRA. Previously it has been shown that FH mRNA negatively and significantly correlated with DAS28-ESR in the synovium only10 which is consistent with the correlation between FH gene expression and DAS28-CRP. We don’t know whether FHR proteins, due to their presence in the synovium, have some direct role in inflammation or simply compete with FH in the synovium to dysregulate AP to cause inflammation. The positive correlation between C3c and MAC confirms activation of the AP in the synovium in eRA.
Nonetheless, FHR proteins can recognize various surfaces but can’t regulate AP. Most of the FHR proteins don’t bind to CRP except FHR4, which has been shown to bind pentameric CRP in contrast to FH, which binds monomeric CRP29. In RA, a significant correlation has been demonstrated between serum CRP levels and tissue inflammation scores from knee synovium biopsy samples28. We have shown that a higher levels of FHR4 mRNA expression in the RA synovium were specifically associated with a worse future clinical outcome following treatment10. In another autoimmune disease, ankylosing spondylitis (AS), FHR5 has been shown to be significantly elevated in the synovial fluid vs. healthy controls62 and furthermore, high FHR5 levels in AS were significantly and positively correlated with the high CRP group63. Thus, the role of FHRs may be disease specific.
We asked the question whether there was any gender-based differences in synovium and blood in the gene expression of FHR and FH, and although the trends in the synovium in females were higher, they were not statistically different (Supplementary Fig. 3). A larger study is required to explore FHR gender-based differences. Regardless, the prevalence of RA is three times more in females than males64 and more plasma-based ELISA assays are needed to measure the absolute levels of various FHR in females and males. We speculate that FHR1 and FHR3 might exacerbate the disease in females. In this PEAC study, we also could not find any significant differences in the gene expression of FHR1, FHR3, FHR4, and FHR5 in synovium and blood-based on ACPA and RF status (Supplementary Figs. 6 and 7). Rheumatoid factors (RF) positivity increases the risk of developing RA65,66. Amongst ACPAs, the assay for anti-cyclic citrullinated peptide (anti-CCP2) is widely clinically used as a biomarker for RA and has excellent diagnostic and prognostic value67. However, in the STRAP clinical study, i.e., in the advanced stage of the disease, a significant correlation was seen between FHR3 expression and RF and CCP levels (Fig. 6). Systemic appearance of RF and ACPA predates the onset of RA by many years68 and crucially important to pathogenesis of RA. FHR3 has been shown to be involved in B cell regulation and FHR3 neutralized the adjuvant effect of C3d on B cells69 therefore synovial local imbalance in FHR3 gene expression can alter B cell tolerance affecting RF and CCP levels. Together with these data from PEAC, eRA, and STRAP, RA clinical studies show that higher trends in FHR3 might point out worsening disease outcomes during the development of RA. The high expression of C3c/FHR3 synovial cells vs. C3c/FHR2, C3c/FHR4 and C3c/FHR5 synovial cells confirm FHR3 crucial role in RA. Thus, there is a pathological association of FHR3 in RA but not in eRA, indicating specific roles of FHR at different stages of RA.
We do acknowledge limitations in our current study. We do not have a specific explanation as to why FH presence is low is missing from the synovial lining. FH binds to sialic acid, however, we have not determined the presence of sialic acid using IHC in the synovial lining of eRA patients along with healthy controls. Nonetheless, we examined the expression of the ST6Gal1 enzyme in the fibroid pathotype and another pathotype, as mentioned above. We have also not determined the presence of other C3 fragments iC3b, C3dg, or C3d to which FHR proteins bind. We have not examined, using MIHC, the presence of FHL-1 proteins in the eRA synovial biopsies, as it may play an inflammatory role in arthritis70. FHL-1 is a multifunctional plasma protein in which 3–5 short consensus repeats have 98% sequence similarly with FH, and interestingly FHR-1 uses all three C-terminal domains to make a contact with the surface. These can be altered, both in FH and FHR-1, in patients with atypical hemolytic-uremic-syndrome71. We don’t know if this type of unique alteration can happen in FH and FHR-1 during inflammatory conditions in RA. It has been shown that as a dimeric modulator, FHR-1 competitively removes FH from surfaces that strongly fix opsonic C3b molecules72. We have examined the presence of FHR proteins and FH using MIHC in macrophages and fibroblasts, however, we cannot distinguish between expression or binding of systemic proteins as an explanation for differences in abundance. Nonetheless the expression of various FHR genes and proteins simultaneously can be measured using the combination of RNAscope and MIHC which we have not yet performed. This cutting-edge RNAscope technology will allow for highly specific visualization and quantification of RNA and protein staining within synovium of RA patients. We have not measured the absolute levels of five-complement proteins individually in the synovial fluid from eRA due to the lack of available ELISA methods and availability of paired samples.
We conclude that all five FHR and FH proteins are expressed in the synovium, but FH is mostly absent from the synovial lining as shown in a putative model (Fig. 8). We speculate that this expression asymmetry could be the active hub of AP dysregulation. Nonetheless individual FHR protein roles in RA synovium can be examined by generating individual humanized FHR transgenic mice with or without FH deficiency. But the caveat will be if the same degree of sialic acids, and expression from cells and interactions across species are maintained. Interestingly, the synovial lining is the well-known major site of disease initiation73,74. In sub-synovial tissues, there was a regional distribution of various FHR proteins, and co-expression with FH in eRA and RA biopsies. FHR3 seems to be a pathogenic protein in RA but is also present in eRA, suggesting a role during the evolution of the disease because like FHR1 it competes with FH for binding to C3b75. Thus in vivo, on the synovial lining, FHR proteins can bind but can’t regulate the AP due to the absence of regulatory domains. We hypothesize that this could be the mechanism of complement deregulation locally in the synovium. This study explains the conundrum of why FH, although present in abundance in eRA synovium, fails to protect the synovial lining.
A putative model showing the theoretical inhibition and activation of complement system by FH and FHR proteins respectively on the surface of synovial lining in eRA. A No complement activation in the presence of FH binding to the synovial lining surface bound C3b and sialic acid. B Complement activation in the presence of FHR proteins and absence of FH binding to various complement fragments such as C3b, iC3b, C3dg, and C3d on the surface of the synovial lining. C Complement activation in the presence and binding of various FHR proteins to the synovial lining. All complement fragments, FH, FHR proteins and sialic acid have been color coded. SL = synovial lining (red color arch outer area). Sub synovial lining area FH is present.
Our data suggests the possibility that reintroduction of FH to cells of the synovial lining may have therapeutic benefit. Use of targeted adeno-associated viruses, (AAVs) expressing FH might be possible. Alternatively, inhibitory humanized anti-FHR3 antibodies might be therapeutic for the treatment of RA. In the future, clinical studies also should focus on the role of FHR3 and other FHRs in managing RA.
Data availability
The data that supports the findings of this study are available from the data exploration website (https://peac.hpc.qmul.ac.uk/). Restrictions apply to the availability of these raw data, which were used for the current study, and so are not publicly available. Some MIHC data are, however, available from the corresponding authors upon reasonable request and but restrictions apply to the availability of raw data from PEAC and STRAP study related groups in UK because some of the data such as STRAP shiny app is not public yet.
Abbreviations
- CP:
-
Classical pathway
- AP:
-
Alternative pathway
- LP:
-
Lectin pathway
- MAC (C5b-9):
-
Membrane attack complex
- FH:
-
Factor H
- FHR:
-
Factor H-related protein
- Human FHR1:
-
Human Factor H-related 1
- Human FHR2:
-
Human Factor H-related 2
- Human FHR3:
-
Human Factor H-related 3
- Human FHR4:
-
Human Factor H related 4
- Human FHR5:
-
Human Factor H-related 5
- DAS28-CRP:
-
Disease activity score C-reactive protein
- MIHC:
-
Multiplexed immunohistochemistry
- RA:
-
Rheumatoid arthritis
- PEAC:
-
Pathobiology of early arthritis cohort
- STRAP:
-
Stratification of biological therapies for rheumatoid arthritis by pathobiology
References
Cross, M. et al. The global burden of rheumatoid arthritis: estimates from the global burden of disease 2010 study. Ann. Rheumatol. Dis. 73, 1316–1322 (2014).
Smolen, J. S. et al. Rheumatoid arthritis. Nat. Rev. Dis. Primers. 4, 18001 (2018).
Fallon, E. A. et al. Prevalence of diagnosed Arthritis - United States, 2019–2021. MMWR Morb Mortal. Wkly. Rep. 72, 1101–1107 (2023).
Singh, D. K. et al. Use of rheumatologic testing in patients who eventually receive a diagnosis of rheumatoid arthritis. South Med. J. 112, 535–538 (2019).
Prevoo, M. L., van ‘t Hof, M. A., Kuper, H. H., van Leeuwen, M. A. & van de Putte, L. B. and P. L. van Riel. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheumatol 38: 44–48. (1995).
Sengul, I., Akcay-Yalbuzdag, S., Ince, B., Goksel-Karatepe, A. & Kaya, T. Comparison of the DAS28-CRP and DAS28-ESR in patients with rheumatoid arthritis. Int. J. Rheumatol. Dis. 18, 640–645 (2015).
Nielen, M. M. et al. Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheumatol. 50, 380–386 (2004).
Ballanti, E. et al. Complement and autoimmunity. Immunol. Res. 56, 477–491 (2013).
Holers, V. M. & Banda, N. K. Complement in the initiation and evolution of rheumatoid arthritis. Front. Immunol. 9, 1057 (2018).
Banda, N. K. et al. Analysis of complement gene expression, clinical associations, and biodistribution of complement proteins in the synovium of early rheumatoid arthritis patients reveals unique pathophysiologic features. J. Immunol. 208, 2482–2496 (2022).
Markiewski, M. M. & Lambris, J. D. The role of complement in inflammatory diseases from behind the scenes into the spotlight. Am. J. Pathol. 171, 715–727 (2007).
Merle, N. S., Noe, R., Halbwachs-Mecarelli, L., Fremeaux-Bacchi, V. & Roumenina, L. T. Complement system part II: role in immunity. Front. Immunol. 6, 257 (2015).
Morgan, B. P., Marchbank, K. J., Longhi, M. P., Harris, C. L. & Gallimore, A. M. Complement: central to innate immunity and bridging to adaptive responses. Immunol. Lett. 97, 171–179 (2005).
Morgan, B. P., Boyd, C. & Bubeck, D. Molecular cell biology of complement membrane attack. Semin Cell. Dev. Biol. 72, 124–132 (2017).
Zwarthoff, S. A. et al. Functional characterization of alternative and classical pathway C3/C5 convertase activity and Inhibition using purified models. Front. Immunol. 9, 1691 (2018).
Foley, J. H. et al. Interplay between fibrinolysis and complement: plasmin cleavage of iC3b modulates immune responses. J. Thromb. Haemost. 13, 610–618 (2015).
Nilsson, U. R., Funke, L., Nilsson, B. & Ekdahl, K. N. Two conformational forms of target-bound iC3b that distinctively bind complement receptors 1 and 2 and two specific monoclonal antibodies. Ups J. Med. Sci. 116, 26–33 (2011).
Jozsi, M. & Zipfel, P. F. Factor H family proteins and human diseases. Trends Immunol. 29, 380–387 (2008).
Zipfel, P. F. et al. Factor H family proteins: on complement, microbes and human diseases. Biochem. Soc. Trans. 30, 971–978 (2002).
Zipfel, P. F. & Skerka, C. Complement factor H and related proteins: an expanding family of complement-regulatory proteins? Immunol. Today. 15, 121–126 (1994).
Karpati, E. et al. Complement factor H family proteins modulate monocyte and neutrophil granulocyte functions. Front. Immunol. 12, 660852 (2021).
Karpati, E. et al. Interaction of the factor H family proteins FHR-1 and FHR-5 with DNA and dead cells: implications for the regulation of complement activation and opsonization. Front. Immunol. 11, 1297 (2020).
Sandor, N. et al. The human factor H protein family—an update. Front. Immunol. 15, 1135490 (2024).
Mehta, G., Ferreira, V. P., Skerka, C., Zipfel, P. F. & Banda, N. K. New insights into disease-specific absence of complement factor H related protein C in mouse models of spontaneous autoimmune diseases. Mol. Immunol. 62, 235–248 (2014).
Castell, J. V. et al. Interleukin-6 is the major regulator of acute phase protein synthesis in adult human hepatocytes. FEBS Lett. 242, 237–239 (1989).
Sproston, N. R. & Ashworth, J. J. Role of C-reactive protein at sites of inflammation and infection. Front. Immunol. 9, 754 (2018).
Pope, J. E. & Choy, E. H. C-reactive protein and implications in rheumatoid arthritis and associated comorbidities. Semin Arthritis Rheumatol. 51, 219–229 (2021).
Orr, C. K. et al. The utility and limitations of CRP, ESR and DAS28-CRP in appraising disease activity in rheumatoid arthritis. Front. Med. (Lausanne). 5, 185 (2018).
Mihlan, M. et al. Human complement factor H-related protein 4 binds and recruits native pentameric C-reactive protein to necrotic cells. Mol. Immunol. 46, 335–344 (2009).
Hebecker, M. et al. Molecular basis of C-reactive protein binding and modulation of complement activation by factor H-related protein 4. Mol. Immunol. 47, 1347–1355 (2010).
McRae, J. L. et al. Human factor H-related protein 5 has cofactor activity, inhibits C3 convertase activity, binds heparin and C-reactive protein, and associates with lipoprotein. J. Immunol. 174, 6250–6256 (2005).
Lewis, M. J. et al. Molecular portraits of early rheumatoid arthritis identify clinical and treatment response phenotypes. Cell. Rep. 28, 2455–2470e2455 (2019).
Rivellese, F. et al. Stratification of biological therapies by pathobiology in biologic-naive patients with rheumatoid arthritis (STRAP and STRAP-EU): two parallel, open-label, biopsy-driven, randomised trials. Lancet Rheumatol. 5, e648–e659 (2023).
Love, M. I., Huber, W. & Anders, S. Moderated Estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Holers, V. M. et al. Potential causal role of synovial complement system activation in the development of post-traumatic osteoarthritis after anterior cruciate ligament injury or meniscus tear. Front. Immunol. 14, 1146563 (2023).
Holers, V. M. et al. Decay-accelerating factor differentially associates with complement-mediated damage in synovium after meniscus tear as compared to anterior cruciate ligament injury. Immune Netw. 24, e17 (2024).
van der Heijde, D. How to read radiographs according to the Sharp/van der Heijde method. J. Rheumatol. 27, 261–263 (2000).
Genant, H. K. et al. Assessment of rheumatoid arthritis using a modified scoring method on digitized and original radiographs. Arthritis Rheumatol. 41, 1583–1590 (1998).
Lewis, M. J. Predicting best treatment in rheumatoid arthritis. Semin Arthritis Rheumatol. 64S, 152329 (2024).
Humby, F. et al. and R. R. c. Group. 2021. Rituximab versus Tocilizumab in anti-TNF inadequate responder patients with rheumatoid arthritis (R4RA): 16-week outcomes of a stratified, biopsy-driven, multicentre, open-label, phase 4 randomised controlled trial. Lancet 397: 305–317 .
Donlin, L. T. et al. Methods for high-dimensional analysis of cells dissociated from cryopreserved synovial tissue. Arthritis Res. Ther. 20: 139. (2018).
Jones, M. B. IgG and leukocytes: targets of Immunomodulatory alpha2,6 Sialic acids. Cell. Immunol. 333, 58–64 (2018).
Wang, Y. et al. Loss of alpha2-6 sialylation promotes the transformation of synovial fibroblasts into a pro-inflammatory phenotype in arthritis. Nat. Commun. 12, 2343 (2021).
Kissel, T., Toes, R. E. M., Huizinga, T. W. J. & Wuhrer, M. Glycobiology of rheumatic diseases. Nat. Rev. Rheumatol. 19, 28–43 (2023).
Eberhardt, H. U. et al. Human factor H-related protein 2 (CFHR2) regulates complement activation. PLoS One. 8, e78617 (2013).
Merinero, M. et al. Molecular bases for the association of FHR-1 with atypical hemolytic uremic syndrome and other diseases. Blood 137, 3484–3494 (2021).
Cserhalmi, M., Papp, A., Brandus, B., Uzonyi, B. & Jozsi, M. Regulation of regulators: role of the complement factor H-related proteins. Semin Immunol. 45, 101341 (2019).
Medjeral-Thomas, N. & Pickering, M. C. The complement factor H-related proteins. Immunol. Rev. 274, 191–201 (2016).
Skerka, C., Chen, Q., Fremeaux-Bacchi, V. & Roumenina, L. T. Complement factor H related proteins (CFHRs). Mol. Immunol. 56, 170–180 (2013).
Leffler, J. et al. Annexin-II, DNA, and histones serve as factor H ligands on the surface of apoptotic cells. J. Biol. Chem. 285, 3766–3776 (2010).
Borza, D. B. Glomerular basement membrane Heparan sulfate in health and disease: a regulator of local complement activation. Matrix Biol. 57–58, 299–310 (2017).
Gyapon-Quast, F. et al. Defining the glycosaminoglycan interactions of complement factor H-related protein 5. J. Immunol. 207, 534–541 (2021).
Mahajan, S. et al. Local complement factor H protects kidney endothelial cell structure and function. Kidney Int. 100, 824–836 (2021).
Jia, Y. et al. Complement factor H attenuates TNF-alpha-induced inflammation by upregulating EIF3C in rheumatoid arthritis. J. Transl Med. 21, 846 (2023).
Jiang Li, K. W. et al. Hoh and. Complement factor H in molecular regulation of angiogenesis. Med. Rev. 4, 452–466. https://doi.org/10.1515/mr-2023-0048 (2024).
Ju, Liu & Hoh, J. Loss of complement factor H in plasma increases endothelial cell migration. J. Cancer. 8 (12), 2184–2190 (2017).
Zhang, F. et al. Deconstruction of rheumatoid arthritis synovium defines inflammatory subtypes. Nature 623: 616–624. (2023).
Molins, B. et al. Complement factor H binding of monomeric C-reactive protein downregulates proinflammatory activity and is impaired with at risk polymorphic CFH variants. Sci. Rep. 6, 22889 (2016).
Seddon, J. M., Gensler, G., Klein, M. L. & Milton, R. C. C-reactive protein and homocysteine are associated with dietary and behavioral risk factors for age-related macular degeneration. Nutrition 22, 441–443 (2006).
Seddon, J. M., George, S., Rosner, B. & Rifai, N. Progression of age-related macular degeneration: prospective assessment of C-reactive protein, Interleukin 6, and other cardiovascular biomarkers. Arch. Ophthalmol. 123, 774–782 (2005).
Vine, A. K., Stader, J., Branham, K., Musch, D. C. & Swaroop, A. Biomarkers of cardiovascular disease as risk factors for age-related macular degeneration. Ophthalmology 112, 2076–2080 (2005).
Lee, J. H. et al. Proteomic analysis of human synovial fluid reveals potential diagnostic biomarkers for ankylosing spondylitis. Clin. Proteom. 17, 20 (2020).
Lee, J. H. et al. The complement factor H-related protein-5 (CFHR5) exacerbates pathological bone formation in ankylosing spondylitis. J. Mol. Med. (Berl). 102, 571–583 (2024).
Linos, A., Worthington, J. W., O’Fallon, W. M. & Kurland, L. T. The epidemiology of rheumatoid arthritis in Rochester, Minnesota: a study of incidence, prevalence, and mortality. Am. J. Epidemiol. 111, 87–98 (1980).
Halldorsdottir, H. D., Jonsson, T., Thorsteinsson, J. & Valdimarsson, H. A prospective study on the incidence of rheumatoid arthritis among people with persistent increase of rheumatoid factor. Ann. Rheumatol. Dis. 59, 149–151 (2000).
Nielsen, S. F., Bojesen, S. E., Schnohr, P. & Nordestgaard, B. G. Elevated rheumatoid factor and long term risk of rheumatoid arthritis: a prospective cohort study. BMJ 345, e5244 (2012).
Shapiro, S. C. Biomarkers in rheumatoid arthritis. Cureus 13, e15063 (2021).
Kurowska, W., Kuca-Warnawin, E. H., Radzikowska, A. & Maslinski, W. The role of anti-citrullinated protein antibodies (ACPA) in the pathogenesis of rheumatoid arthritis. Cent. Eur. J. Immunol. 42, 390–398 (2017).
Buhlmann, D. et al. FHR3 blocks C3d-Mediated coactivation of human B cells. J. Immunol. 197, 620–629 (2016).
Friese, M. A. et al. Release of endogenous anti-inflammatory complement regulators FHL-1 and factor H protects synovial fibroblasts during rheumatoid arthritis. Clin. Exp. Immunol. 132, 485–495 (2003).
Luce Perie, S. et al. Unique target binding by the C-terminal region of FHR1 provides a new perception of aHUS pathology Front. Hematol. 3. (2024).
Dopler, A. et al. Deregulation of factor H by factor H-related protein 1 depends on sialylation of host surfaces. Front. Immunol. 12, 615748 (2021).
Tak, P. P. & Bresnihan, B. The pathogenesis and prevention of joint damage in rheumatoid arthritis: advances from synovial biopsy and tissue analysis. Arthritis Rheumatol. 43, 2619–2633 (2000).
Firestein, G. S. Evolving concepts of rheumatoid arthritis. Nature 423, 356–361 (2003).
Fritsche, L. G. et al. An imbalance of human complement regulatory proteins CFHR1, CFHR3 and factor H influences risk for age-related macular degeneration (AMD). Hum. Mol. Genet. 19, 4694–4704 (2010).
Acknowledgements
We are thankful to Mr. William Apruzzese from the AMP/RA/SLE network, who originally worked with this network and provided and shipped most of the eRA biopsies used in this study. All authors are grateful to the Radiology department nursing staff and sonographer nurses at the University of Colorado Anschutz Medical Campus, Aurora, for identifying and generating ultrasound images of the synovitis and helping to obtain synovial biopsies from eRA and RA patients. We are also thankful to the CU Human Immune Monitoring Shared Resource (HIMSR) group at AMC and specifically to Dr. Kimberley Jordan, Ms. Alyssa Howard, and Mr. Troy Schedin for helping to standardize all FHR proteins and also writing the algorithm for calculating the percentage of positive cells in the eRA synovium and also generating MIHC composite images.
Funding
Supported by the National Institutes of Health grant R01 AR51749 to VMH (PI) and NKB (Co-I) and by an Interdisciplinary Joint Biology Program pilot grant to NKB (PI) and RMF (Co-I). This work was supported by the Accelerating Medicines Partnership® Rheumatoid Arthritis and Systemic Lupus Erythematosus (AMP® RA/SLE) Network. AMP is a public-private partnership (AbbVie Inc., Arthritis Foundation, Bristol-Myers Squibb Company, Foundation for the National Institutes of Health, GlaxoSmithKline, Janssen Research and Development, LLC, Lupus Foundation of America, Lupus Research Alliance, Merck & Co., Inc., National Institute of Allergy and Infectious Diseases, National Institute of Arthritis and Musculoskeletal and Skin Diseases, Pfizer Inc., Rheumatology Research Foundation, Sanofi and Takeda Pharmaceuticals International, Inc.) created to develop new ways of identifying and validating promising biological targets for diagnostics and drug development. Funding was provided through grants from the National Institutes of Health (UH2-AR067676, UH2-AR067677, UH2-AR067679, UH2-AR067681, UH2-AR067685, UH2- AR067688, UH2-AR067689, UH2-AR067690, UH2-AR067691, UH2-AR067694, and UM2- AR067678).
Author information
Authors and Affiliations
Consortia
Contributions
NKB is the Co-I on NIH R01 grant-related human eRA and RA studies, conceived the original idea to analyze human CFHR and CFH gene expression from PEAC and STRAP studies, performed MIHC to analyze all CFHR, CFH, C3c, MAC, fibroblasts, and macrophages, analyzed all data, and wrote the first and revised draft of the manuscript. LWM was involved in eRA synovium-related discussions and provided synovial biopsies from the knee joints of OA and RA patients, and some of these biopsies were used for MIHC. KDD provided many eRA biopsies from patients used to standardize the presence of CFHR proteins using MIHC. DS shared his expertise in the areas of CFH and CFHR proteins. RIS discussed the role of CFH and CFHR proteins in-depth, provided input related to the mechanism, and made excellent suggestions. RMF provided synovial discard from OA patients used to standardize MIHC for CFH and CFHR proteins. JS assisted in collecting synovial biopsies, processing histology samples, and following up on the care of eRA and RA patients. RL generated bulk RNA-seq graphs and provided correlation data and also assisted in the statistical section. CP originally conducted PEAC and R4RA, two landmark studies using eRA and RA synovial biopsies from RA patients and shared all data. MJL conducted PEAC and R4RA clinical trials and established two excellent websites related to PEAC and R4RA, provided CFHR and CFH data after discussions, and reviewed this manuscript. VMH is the PI on the NIH R01 grant related to the human eRA and RA studies, originated and supervised the overall project, and reviewed and revised this manuscript. All authors contributed to this manuscript and approved its submission. The members of the accelerating medicines partnership (AMP) in RA/SLE network: University of Rochester Medical Center: Jennifer Anolik, Darren Tabechian, Ralf Thiele, Jennifer Hossler, Brendan Boyce, Nida Meednu, Javier Rangel-Moreno and Christopher Ritchlin. Hospital for Special Surgery (HSS): Vivian Bykerk, Laura Donlin, Susan Goodman, Ed DiCarlo, Dana Orange, John Carrino, Oganna (Kenny), Nwawka Endo Yoshimi, Rahul Satija, Lionel Ivashkiv, Alessandra Pernis, Robert Darnell, Mark Figgie, and Michael McNamara. University of Pittsburgh: Mandy J. McGeachy, Jay Kolls, Aaron Wise, and Andrew Cordle. Feinstein/Northwell: Peter Gregersen, and Diane Horowitz. UK Birmingham (under Feinstein/Northwell): Andrew D. Filer, Jason Turner Holly Adams. UK London (under Feinstein/Northwell): Costantino Pitzalis, and Stephen Kelly Rebecca Hands. Brigham and Women’s Hospital Derrick Todd, Kevin Wei, Deepak Rao and Fumitaka Mizoguchi. University of Colorado (EMORA): V. Michael Holers, Kevin D. Deane, Jennifer A. Seifert, Nirmal K. Banda, Larry W. Moreland, Alexander Merkle, and Colin Strickland. University of California San Diego (EMORA): Gary S. Firestein and David Boyle. Cedars Sinai (EMORA): Michael H. Weisman, Ami Ben-Artzi, and Lindsy Forbess. University of Massachusetts (EMORA): Ellen Gravallese and Karen Salomon-Escoto. Northwestern University (REASON under EMORA Network): Harris Perlman, and Arthur Mandelin Emily Bacalao. Washington University (REASON): Deborah Parks and John Atkinson. Columbia University (REASON): Joan Bathon. Mayo Clinic (REASON): Eric Matteson.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. NKB: royalties, and patents for the treatment of inflammatory diseases using anti-C5aR1ab-C5siRNA conjugate. LWM: none; KDD: none; DS, none; RIS: none; RMF: none; JS, none; RL: none; CP: none; MJL: none; VMH: royalties, consulting income, stock, and stock options in complement therapeutics companies.
Ethical approval and consent to participate
Written ethical informed consent was obtained from all eRA patients according to the preapproved Colorado Multiple Institutional Review Board protocol (COMIRB # 20-1908 and 15-1389). All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols related to these studies were approved by the Institutional Review Board committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the accelerating medicines partnership (AMP) in RA/SLE network are listed in acknowledgements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Banda, N.K., Moreland, L.W., Deane, K.D. et al. Analysis of human factor H-related gene and protein expressed in rheumatoid arthritis synovium identifies a novel mechanism promoting dysregulated complement pathway activation. Sci Rep 15, 19633 (2025). https://doi.org/10.1038/s41598-025-03589-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03589-1