Abstract
Food addiction contributes to the obesity pandemic, but the connection between how the gut microbiome is linked to food addiction remains largely unclear. Here we show that Microviridae bacteriophages, particularly Gokushovirus WZ-2015a, are associated with food addiction and obesity across multiple human cohorts. Further analyses reveal that food addiction and Gokushovirus are linked to serotonin and dopamine metabolism. Mice receiving faecal microbiota and viral transplantation from human donors with the highest Gokushovirus load exhibit increased food addiction along with changes in tryptophan, serotonin and dopamine metabolism in different regions of the brain, together with alterations in dopamine receptors. Mechanistically, targeted tryptophan analysis shows lower anthranilic acid (AA) concentrations associated with Gokushovirus. AA supplementation in mice decreases food addiction and alters pathways related to the cycle of neurotransmitter synthesis release. In Drosophila, AA regulates feeding behaviour and addiction-like ethanol preference. In summary, this study proposes that bacteriophages in the gut microbiome contribute to regulating food addiction by modulating tryptophan and tyrosine metabolism.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
The datasets that support the findings of the study are available from the corresponding author upon reasonable request. The raw metagenomics sequence data derived from human samples in the IRONMET-CGM, IRONMET, Aging Imageomics and Health Imageomics cohorts have been deposited in the European Nucleotide Archive under project numbers PRJEB58106, PRJEB39631, PRJEB52682 and PRJEB61680, respectively. The raw metagenomics sequence data from the second FMT experiment have also been deposited in the European Nucleotide Archive under project number PRJEB39631. The source data for the mice and Drosophila studies can be found in Supplementary Tables 70–75.
References
Blüher, M. Obesity: global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 15, 288–298 (2019).
Praxedes, D. R. S. et al. Prevalence of food addiction determined by the Yale Food Addiction Scale and associated factors: a systematic review with meta-analysis. Eur. Eat. Disord. Rev. 30, 85–95 (2022).
Gupta, A., Osadchiy, V. & Mayer, E. A. Brain-gut-microbiome interactions in obesity and food addiction. Nat. Rev. Gastroenterol. Hepatol. 17, 655–672 (2020).
Vasiliu, O. Current status of evidence for a new diagnosis: food addiction-a literature review. Front. Psychiatry 12, 824936 (2022).
Schulte, E. M., Potenza, M. N. & Gearhardt, A. N. A commentary on the ‘eating addiction’ versus ‘food addiction’ perspectives on addictive-like food consumption. Appetite 115, 9–15 (2017).
Randolph, T. The descriptive features of food addiction; addictive eating and drinking. Q. J. Stud. Alcohol 17, 198–224 (1956).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-V) (American Psychiatric Association, 2013).
Gearhardt, A. N., Corbin, W. R. & Brownell, K. D. Development of the Yale Food Addiction Scale version 2.0. Psychol. Addict. Behav. 30, 113–121 (2016).
Martín-García, E., Domingo-Rodriguez, L. & Maldonado, R. An operant conditioning model combined with a chemogenetic approach to study the neurobiology of food addiction in mice. Bio. Protoc. 10, e3777 (2020).
Domingo-Rodriguez, L. et al. A specific prelimbic-nucleus accumbens pathway controls resilience versus vulnerability to food addiction. Nat. Commun. 11, 782 (2020).
Cryan, J. F. et al. The microbiota-gut-brain axis. Physiol. Rev. 99, 1877–2013 (2019).
Bäckhed, F., Manchester, J. K., Semenkovich, C. F. & Gordon, J. I. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc. Natl Acad. Sci. USA 104, 979–984 (2007).
Ridaura, V. K. et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341, 1241214 (2013).
Boulangé, C. L., Neves, A. L., Chilloux, J., Nicholson, J. K. & Dumas, M.-E. Impact of the gut microbiota on inflammation, obesity, and metabolic disease. Genome Med. 8, 42 (2016).
García-Cabrerizo, R., Carbia, C., O´Riordan, K. J., Schellekens, H. & Cryan, J. F. Microbiota-gut-brain axis as a regulator of reward processes. J. Neurochem. 157, 1495–1524 (2021).
Novelle, M. G. Decoding the role of gut-microbiome in the food addiction paradigm. Int. J. Environ. Res. Public Health 18, 6825 (2021).
Hsu, B. B. et al. Dynamic modulation of the gut microbiota and metabolome by bacteriophages in a mouse model. Cell Host Microbe 25, 803–814.e5 (2019).
David, L. A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505, 559–563 (2014).
Minot, S. et al. The human gut virome: inter-individual variation and dynamic response to diet. Genome Res. 21, 1616–1625 (2011).
Shkoporov, A. N. et al. The human gut virome is highly diverse, stable, and individual specific. Cell Host Microbe 26, 527–541.e5 (2019).
Schulfer, A. et al. Fecal viral community responses to high-fat diet in mice. mSphere 5, e00833-19 (2020).
Ross, R. et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 16, 177–189 (2020).
Schulte, E. M., Grilo, C. M. & Gearhardt, A. N. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin. Psychol. Rev. 44, 125–139 (2016).
Adams, R. C., Sedgmond, J., Maizey, L., Chambers, C. D. & Lawrence, N. S. Food addiction: implications for the diagnosis and treatment of overeating. Nutrients 11, 2086 (2019).
Roux, S. et al. Minimum information about an uncultivated virus genome (MIUViG). Nat. Biotechnol. 37, 29–37 (2019).
Fan, S. et al. Microbiota-gut-brain axis drives overeating disorders. Cell Metab. 35, 2011–2027.e7 (2023).
Lechner, W. V., Sidhu, N. K., Kittaneh, A. A. & Anand, A. Interventions with potential to target executive function deficits in addiction: current state of the literature. Curr. Opin. Psychol. 30, 24–28 (2019).
Luijten, M., Schellekens, A. F., Kühn, S., MacHielse, M. W. J. & Sescousse, G. Disruption of reward processing in addiction: an image-based meta-analysis of functional magnetic resonance imaging studies. JAMA Psychiatry 74, 387–398 (2017).
Escrichs, A. et al. Whole-brain dynamics in aging: disruptions in functional connectivity and the role of the rich club. Cereb. Cortex 31, 2466–2481 (2021).
Huckins, J. F. et al. Reward-related regions form a preferentially coupled system at rest. Hum. Brain Mapp. 40, 361–376 (2019).
Zilverstand, A., Huang, A. S., Alia-Klein, N. & Goldstein, R. Z. Neuroimaging impaired response inhibition and salience attribution in human drug addiction: a systematic review. Neuron 98, 886–903 (2018).
Volkow, N. D., Wise, R. A. & Baler, R. The dopamine motive system: implications for drug and food addiction. Nat. Rev. Neurosci. 18, 741–752 (2017).
Hellyer, P. J., Scott, G., Shanahan, M., Sharp, D. J. & Leech, R. Cognitive flexibility through metastable neural dynamics is disrupted by damage to the structural connectome. J. Neurosci. 35, 9050–9063 (2015).
Sternberg, D. E., Heninger, G. R. & Both, R. H. Plasma homovanillic acid as an index of brain dopamine metabolism: enhancement with debrisoquin. Life Sci. 32, 2447–2452 (1983).
Alex, K. D. & Pehek, E. A. Pharmacologic mechanisms of serotonergic regulation of dopamine neurotransmission. Pharmacol. Ther. 113, 296–320 (2007).
Everitt, B. J. Neural and psychological mechanisms underlying compulsive drug seeking habits and drug memories–indications for novel treatments of addiction. Eur. J. Neurosci. 40, 2163–2182 (2014).
Volkow, N. D., Michaelides, M. & Baler, R. The neuroscience of drug reward and addiction. Physiol. Rev. 99, 2115–2140 (2019).
Volkow, N. D., Fowler, J. S., Wang, G. J., Swanson, J. M. & Telang, F. Dopamine in drug abuse and addiction: results of imaging studies and treatment implications. Arch. Neurol. 64, 1575–1579 (2007).
Everitt, B. J. et al. Review. Neural mechanisms underlying the vulnerability to develop compulsive drug-seeking habits and addiction. Philos. Trans. R. Soc. Lond. B Biol. Sci. 363, 3125–3135 (2008).
Goldstein, R. Z. & Volkow, N. D. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat. Rev. Neurosci. 12, 652–669 (2011).
Weygandt, M. et al. Impulse control in the dorsolateral prefrontal cortex counteracts post-diet weight regain in obesity. Neuroimage 109, 318–327 (2015).
Riga, D. et al. Optogenetic dissection of medial prefrontal cortex circuitry. Front. Syst. Neurosci. 8, 230 (2014).
Wang, G. J. et al. Brain dopamine and obesity. Lancet 357, 354–357 (2001).
Volkow, N. D. et al. Low dopamine striatal D2 receptors are associated with prefrontal metabolism in obese subjects: possible contributing factors. Neuroimage 42, 1537–1543 (2008).
Pfaffly, J. et al. Leptin increases striatal dopamine D2 receptor binding in leptin-deficient obese (ob/ob) mice. Synapse 64, 503–510 (2010).
Johnson, P. M. & Kenny, P. J. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat. Neurosci. 13, 635–641 (2010).
Dong, T. S. et al. A distinct brain-gut-microbiome profile exists for females with obesity and food addiction. Obesity 28, 1477–1486 (2020).
Kursa, M. B. & Rudnicki, W. R. Feature selection with the boruta package. J. Stat. Softw. 36, 1–13 (2010).
Lundberg, S. M. et al. From local explanations to global understanding with explainable AI for trees. Nat. Mach. Intell. 2, 56–67 (2020).
Dodd, D. et al. A gut bacterial pathway metabolizes aromatic amino acids into nine circulating metabolites. Nature 551, 648–652 (2017).
Negatu, D. A. et al. Gut microbiota metabolite indole propionic acid targets tryptophan biosynthesis in Mycobacterium tuberculosis. mBio 10, e02781-18 (2019).
Shaw, C., Hess, M. & Weimer, B. C. Microbial-derived tryptophan metabolites and their role in neurological disease: anthranilic acid and anthranilic acid derivatives. Microorganisms 11, 1825 (2023).
Scofield, M. D. et al. The nucleus accumbens: mechanisms of addiction across drug classes reflect the importance of glutamate homeostasis. Pharmacol. Rev. 68, 816–871 (2016).
Kalivas, P. W. The glutamate homeostasis hypothesis of addiction. Nat. Rev. Neurosci. 10, 561–572 (2009).
Fetcho, R. N. et al. A stress-sensitive frontostriatal circuit supporting effortful reward-seeking behavior. Neuron 112, 473–487.e4 (2024).
Biria, M. et al. Cortical glutamate and GABA are related to compulsive behaviour in individuals with obsessive compulsive disorder and healthy controls. Nat. Commun. 14, 3324 (2023).
Shyu, C., Chavez, S., Boileau, I. & Le Foll, B. Quantifying GABA in addiction: a review of proton magnetic resonance spectroscopy studies. Brain Sci. 12, 918 (2022).
Ducker, G. S. & Rabinowitz, J. D. One-carbon metabolism in health and disease. Cell Metab. 25, 27–42 (2017).
Fanet, H., Capuron, L., Castanon, N., Calon, F. & Vancassel, S. Tetrahydrobioterin (BH4) pathway: from metabolism to neuropsychiatry. Curr. Neuropharmacol. 19, 591–609 (2021).
Fussi, F., Savoldi, F. & Curti, M. Identification of N-carboxyethyl γ-aminobutyric acid in bovine brain and human cerebrospinal fluid. Neurosci. Lett. 77, 308–310 (1987).
McFarland, K., Lapish, C. C. & Kalivas, P. W. Prefrontal glutamate release into the core of the nucleus accumbens mediates cocaine-induced reinstatement of drug-seeking behavior. J. Neurosci. 23, 3531–3537 (2003).
Moulin, T. C. et al. Transient administration of dopaminergic precursor causes inheritable overfeeding behavior in young Drosophila melanogaster adults. Brain Sci. 10, 1–10 (2020).
Kaun, K. R., Devineni, A. V. & Heberlein, U. Drosophila melanogaster as a model to study drug addiction. Hum. Genet. 131, 959–975 (2012).
Devineni, A. V. & Heberlein, U. Preferential ethanol consumption in Drosophila models features of addiction. Curr. Biol. 19, 2126–2132 (2009).
Chvilicek, M. M., Titos, I. & Rothenfluh, A. The neurotransmitters involved in Drosophila alcohol-induced behaviors. Front. Behav. Neurosci. 14, 607700 (2020).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45, 2–19 (2017).
Boileau, I. et al. Higher binding of the dopamine D3 receptor-preferring ligand [11C]-(+)-propyl-hexahydro-naphtho-oxazin in methamphetamine polydrug users: a positron emission tomography study. J. Neurosci. 32, 1353–1359 (2012).
Payer, D. E. et al. Heightened D3 dopamine receptor levels in cocaine dependence and contributions to the addiction behavioral phenotype: a positron emission tomography study with [11C]-+-PHNO. Neuropsychopharmacology 39, 311–318 (2014).
Glickstein, S. B., DeSteno, D. A., Hof, P. R. & Schmauss, C. Mice lacking dopamine D2 and D3 receptors exhibit differential activation of prefrontal cortical neurons during tasks requiring attention. Cereb. Cortex 15, 1016–1024 (2005).
Puig, J. et al. The aging imageomics study: rationale, design and baseline characteristics of the study population. Mech. Ageing Dev. 189, 111257 (2020).
Granero, R. et al. Validation of the Spanish Version of the Yale Food Addiction Scale 2.0 (YFAS 2.0) and clinical correlates in a sample of eating disorder, gambling disorder, and healthy control participants. Front. Psychiatry 9, 208 (2018).
Torrubia, R., Ávila, C., Moltó, J. & Caseras, X. The Sensitivity to Punishment and Sensitivity to Reward Questionnaire (SPSRQ) as a measure of Gray’s anxiety and impulsivity dimensions. Pers. Individ. Dif. 31, 837–862 (2001).
Corr, P. J., Deyoung, C. G. & Mcnaughton, N. Motivation and personality: a neuropsychological perspective. Soc. Personal Psychol. Compass. 7, 158–175 (2013).
Golden, C. A Manual for the Clinical and Experimental Use of the Stroop Color and Word Test (Stoelting, 1978).
Whiteside, S. P. & Lynam, D. R. The Five Factor Model and impulsivity: using a structural model of personality to understand impulsivity. Pers. Individ. Dif. 30, 669–689 (2001).
Cándido, A., Orduña, E., Perales, J. C., Verdejo-García, A. & Billieux, J. Validation of a short Spanish version of the UPPS-P impulsive behaviour scale. Trastor. Adict. 14, 73–78 (2012).
Chen, S., Zhou, Y., Chen, Y. & Gu, J. fastp: an ultra-fast all-in-one FASTQ preprocessor. Bioinformatics 34, i884–i890 (2018).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Tamames, J. & Puente-Sánchez, F. SqueezeMeta, a highly portable, fully automatic metagenomic analysis pipeline. Front. Microbiol. 9, 3349 (2019).
Li, D., Liu, C. M., Luo, R., Sadakane, K. & Lam, T. W. MEGAHIT: an ultra-fast single-node solution for large and complex metagenomics assembly via succinct de Bruijn graph. Bioinformatics 31, 1674–1676 (2015).
Hyatt, D. et al. Prodigal: prokaryotic gene recognition and translation initiation site identification. BMC Bioinform. 11, 119 (2010).
Buchfink, B., Reuter, K. & Drost, H. G. Sensitive protein alignments at tree-of-life scale using DIAMOND. Nat. Methods 18, 366–368 (2021).
Herwig, R., Hardt, C., Lienhard, M. & Kamburov, A. Analyzing and interpreting genome data at the network level with ConsensusPathDB. Nat. Protoc. 11, 1889–1907 (2016).
Schmieder, R. & Edwards, R. Quality control and preprocessing of metagenomic datasets. Bioinformatics 27, 863–864 (2011).
Magoc, T. & Salzberg, S. L. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics 27, 2957–2963 (2011).
Menzel, P., Ng, K. L. & Krogh, A. Fast and sensitive taxonomic classification for metagenomics with Kaiju. Nat. Commun. 7, 11257 (2016).
Mills, R., Rozanov, M., Lomsadze, A., Tatusova, T. & Borodovsky, M. Improving gene annotation of complete viral genomes. Nucleic Acids Res. 31, 7041–7055 (2003).
Camacho, C. et al. BLAST+: architecture and applications. BMC Bioinform. 10, 421 (2009).
Moraru, C., Varsani, A. & Kropinski, A. M. VIRIDIC—A novel tool to calculate the intergenomic similarities of prokaryote-infecting viruses. Viruses 12, 1268 (2020).
Bolduc, B. et al. vConTACT: an iVirus tool to classify double-stranded DNA viruses that infect Archaea and Bacteria. PeerJ 5, e3243 (2017).
Martinez-Hernandez, F. et al. Single-virus genomics reveals hidden cosmopolitan and abundant viruses. Nat. Commun. 8, 15892 (2017).
Shmakov, S. A., Wolf, Y. I., Savitskaya, E., Severinov, K. V. & Koonin, E. V. Mapping CRISPR spaceromes reveals vast host-specific viromes of prokaryotes. Commun. Biol. 3, 321 (2020).
Mayneris-Perxachs, J. et al. Caudovirales bacteriophages are associated with improved executive function and memory in flies, mice, and humans. Cell Host Microbe 30, 340–356.e8 (2022).
Lin, H. & Peddada, S. D. Analysis of compositions of microbiomes with bias correction. Nat. Commun. 11, 3514 (2020).
Zhou, C., Wang, H., Zhao, H. & Wang, T. fastANCOM: a fast method for analysis of compositions of microbiomes. Bioinformatics 38, 2039–2041 (2022).
Yang, L. & Chen, J. A comprehensive evaluation of microbial differential abundance analysis methods: current status and potential solutions. Microbiome 10, 130 (2022).
Carvajal-Rodríguez, A., de Uña-Alvarez, J. & Rolán-Alvarez, E. A new multitest correction (SGoF) that increases its statistical power when increasing the number of tests. BMC Bioinform. 10, 209 (2009).
Wu, T. et al. clusterProfiler 4.0: a universal enrichment tool for interpreting omics data. Innovation 2, 100141 (2021).
Fernandes, A. D. et al. Unifying the analysis of high-throughput sequencing datasets: characterizing RNA-seq, 16S rRNA gene sequencing and selective growth experiments by compositional data analysis. Microbiome 2, 15 (2014).
Ritchie, M. E. et al. Limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47 (2015).
Robinson, M. D., McCarthy, D. J. & Smyth, G. K. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 26, 139–140 (2010).
Szklarczyk, D. et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 47, D607–D613 (2019).
Kamburov, A., Stelzl, U., Lehrach, H. & Herwig, R. The ConsensusPathDB interaction database: 2013 Update. Nucleic Acids Res. 41, D793–D800 (2013).
Shen, X., Tokoglu, F., Papademetris, X. & Constable, R. T. Groupwise whole-brain parcellation from resting-state fMRI data for network node identification. Neuroimage 82, 403–415 (2013).
Finn, E. S. et al. Functional connectome fingerprinting: identifying individuals using patterns of brain connectivity. Nat. Neurosci. 18, 1664–1671 (2015).
Jenkinson, M., Bannister, P., Brady, M. & Smith, S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage 17, 825–841 (2002).
Yan, C. G. et al. A comprehensive assessment of regional variation in the impact of head micromovements on functional connectomics. Neuroimage 76, 183–201 (2013).
Deco, G. & Kringelbach, M. L. Hierarchy of information processing in the brain: a novel ‘intrinsic ignition’ framework. Neuron 94, 961–968 (2017).
Zhao, S., Li, H., Han, W., Chan, W. & Li, L. Metabolomic coverage of chemical-group-submetabolome analysis: group classification and four-channel chemical isotope labeling LC-MS. Anal. Chem. 91, 12108–12115 (2019).
Whiley, L. et al. Ultra-high-performance liquid chromatography tandem mass spectrometry with electrospray ionization quantification of tryptophan metabolites and markers of gut health in serum and plasma-application to clinical and epidemiology cohorts. Anal. Chem. 91, 5207–5216 (2019).
Lai, Y., Liu, C. W., Chi, L., Ru, H. & Lu, K. High-resolution metabolomics of 50 neurotransmitters and tryptophan metabolites in feces, serum, and brain tissues using UHPLC-ESI-Q exactive mass spectrometry. ACS Omega 6, 8094–8103 (2021).
García-Blanco, A. et al. miRNA signatures associated with vulnerability to food addiction in mice and humans. J. Clin. Invest. 132, e156281 (2022).
Mancino, S. et al. Epigenetic and proteomic expression changes promoted by eating addictive-like behavior. Neuropsychopharmacology 40, 2788–2800 (2015).
Martín-García, E. et al. New operant model of reinstatement of food-seeking behavior in mice. Psychopharmacology 215, 49–70 (2011).
Deroche-Gamonet, V., Belin, D. & Piazza, P. V. Evidence for addiction-like behavior in the rat. Science 305, 1014–1017 (2004). (1979).
Paxinos, G. & Franklin, K. B. J. The Mouse Brain in Stereotaxic Coordinates (Academic Press, 1997).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29, 15–21 (2013).
Liao, Y., Smyth, G. K. & Shi, W. FeatureCounts: an efficient general purpose program for assigning sequence reads to genomic features. Bioinformatics 30, 923–930 (2014).
Castells-Nobau, A. et al. Conserved regulation of neurodevelopmental processes and behavior by FoxP in Drosophila. PLoS ONE 14, e0211652 (2019).
Wu, Q. et al. Excreta quantification (EX-Q) for longitudinal measurements of food intake in Drosophila. iScience 23, 100776 (2020).
Shell, B. C. et al. Measurement of solid food intake in Drosophila via consumption-excretion of a dye tracer. Sci. Rep. 8, 11536 (2018).
Kubrak, O. et al. The gut hormone allatostatin C/somatostatin regulates food intake and metabolic homeostasis under nutrient stress. Nat. Commun. 13, 692 (2022).
Ja, W. W. et al. Prandiology of Drosophila and the CAFE assay. Proc. Natl Acad. Sci. USA 104, 8253–8256 (2007).
Diegelmann, S. et al. The CApillary FEeder assay measures food intake in Drosophila melanogaster. J. Vis. Exp. 2017, 55024 (2017).
Itskov, P. M. et al. Automated monitoring and quantitative analysis of feeding behaviour in Drosophila. Nat. Commun. 5, 4560 (2014).
Acknowledgements
This work was partially funded by Instituto de Salud Carlos III (ISCIII, Madrid, Spain) through the project PI15/01934 to J.M.F.-R. and the projects PI20/01090 and PI23/00575 (co-funded by the European Union under the European Regional Development Fund (FEDER) ‘A way to make Europe’) to J.M.-P. (HR22-00737). The Aging Imageomics Study was funded by Pla estratègic de recerca i innovació en salut 2016–2020 from Generalitat de Catalunya (reference no. SLT002/16/00250). Health Imageomics was funded by Health LivingLab operation of the Girona Healthy Region Program, which was granted by the Projectes d’Especialització i Competitivitat Territorial of the RIS3Cat and the Operative Programme of the European Regional Development Fund of Catalonia 2014–2020. This work was also supported by the Spanish ‘Ministerio de Ciencia e Innovación (MICIN), Agencia Estatal de Investigación’ (PID2020-120029GB-I00/MICIN/AEI/10.13039/501100011033, RD21/0009/0019, to R.M.; the ‘Generalitat de Catalunya, AGAUR’ (2017 SGR-669, to R.M.; the ‘ICREA-Acadèmia’ (2020, to R.M.); the ‘European Commission-DG Research’ (PainFact, H2020-SC1-2019-2-RTD-848099, QSPain Relief, H2020-SC1-2019-2-RTD-848068, to R.M.); the Spanish ‘la Caixa’ Foundation under project code LCF/PR/HR22/52420017 to R.M. and J.M.F.-R.; the Spanish ‘Instituto de Salud Carlos III, RETICS-RTA’ (RD16/0017/0020, to R.M.); the Spanish ‘Ministerio de Sanidad, Servicios Sociales e Igualdad, Plan Nacional Sobre Drogas’ (PNSD-2021I076, to R.M.; PNSD-2023I040, to E.M.G.; and Ministerio de Ciencia e Innovación (ERA-NET) PCI2021-122073-2A to E.M.G. This study has been co-financed by FEDER funds from the European Union (‘A way to build Europe’) and the Generalitat of Catalonia: Agency for Management of University and Research Grants (2021SGR00990) and Department of Health (SLT002/16/00250) to R.P. IDIBGI is a CERCA Programme/Generalitat de Catalunya. J.M.-P. and A.C.N. are funded by Instituto de Salud Carlos III (Madrid, Spain) through the Miguel Servet Program CP18/00009 and Sara Borrell Program CD20/00051 (co-funded by the European Union under the European Social Fund ‘Investing in Your Future’), respectively. L.V.-C. is funded by the Program for the Promotion of Talent and Employability (Generalitat de Catalunya) SLT017_20_000164. This study was conducted using samples and/or data from the Aging Imageomics Study, supported by the Generalitat de Catalunya through the Strategic Plan for Health Research and Innovation 2016–2020 (SLT002/16/00250). We particularly acknowledge the participants of the IDIBGI Horizontal Aging Program and the IDIBGI Biobank (Biobanc IDIBGI, B.0000872), integrated in the Platform ISCIII Biomodels and Biobanks, for their collaboration. This study was conducted using samples and/or data from the Healthy Imageomics Study, supported by the Specialization and Territorial Competitiveness Projects within the RIS3Cat and the Catalonia European Regional Development Fund (ERDF) Operational Programme 2014–2020. It was co-financed by the ERDF of the European Union under the Catalonia ERDF Operational Programme 2014–2020 and by the Diputació de Girona. Illustrations were created with Biorender.com.
Author information
Authors and Affiliations
Contributions
A.C.-N. researched the data, performed the statistical analysis and wrote the manuscript; A.C.-N., L.V.-C. and I.P. performed the Drosophila experiments; E.M.-G. and R.M. supervised, performed or analysed the experiments in mice; M.R.-D., A.M.-A. and M.A.-R. performed the clinical or neuropsychological examination; V.P.-B. and A.M. contributed with the determination and analysis of the microbiota; A.E. and G.D. researched the MRI data; R.P., M.J. and J.S. performed the metabolomics analyses; M.M.-G. helped in the identification of the bacteriophage host; J.P., J.G.-O., R.R. and L.R.-T. contributed to the discussion and reviewed the manuscript. J.M.-P. and J.M.F.-R. carried out the conception and coordination of the study, performed the statistical analysis and wrote the manuscript. All authors participated in final approval of the version to be published. We thank R. Martín and C. Zapata for their technical support.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competinginterests.
Peer review
Peer review information
Nature Metabolism thanks Serguei Fetissov, A. Veronica Witte and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Yanina-Yasmin Pesch, in collaboration with the Nature Metabolism team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1
Consort diagram for the discovery cohort (IRONMET-CGM). The diagram illustrates recruitment numbers and participant flow for the IRONMET-CGM study.
Extended Data Fig. 2 Gut microbiome and YFAS.
a) fastANCOM microbiome differential abundance volcano plot at the family level for YFAS controlling for age, BMI, gender, and education years as covariates in the discovery cohort IRONMET-CGM. The W-statistic represents the number of times the null hypothesis is rejected (two-sided t-test) by the analysis for a given family from all K models. Beta represents the effect size given by the coefficient of the log-linear regression model of each family against the YFAS score. Dotted lines show W-statistic quantile detection thresholds: >0.6 (red), >0.7 (light blue), >0.8 (green), >0.9 (dark blue). c–e) ANCOM-BC (two-sided Z-test using the statistic W = log2Fold Change/standard error) and b, f, g) ZicoSeq (omnibus F-statistic) microbiome differential abundance volcano plot at the family level for YFAS controlling for age, BMI, gender, and education years as covariates in b) the discovery cohort (IRONMET-CGM) c) women with obesity of the validation cohort (IRONMET) and, d, f) women and d, g) men of the discovery cohort (IRONMET-CGM). Fold change associated with a unit change in the YFAS score and log10 p values adjusted for multiple testing are plotted for each family.
Extended Data Fig. 3 Gut microbiome and YFAS components.
ANCOM-BC microbiome differential abundance (two-sided Z-test using the statistic W = log2Fold Change/standard error) volcano plot at the family level for a) YFAS in the discovery cohort (IRONMET-CGM) and b) for YFAS in the validation cohort 1 (IRONMET); c) YFAS motivation, d) YFAS persistence, e) YFAS compulsivity for the discovery cohort IRONMET-CGM; f) YFAS motivation, g) YFAS persistence, h) YFAS compulsivity for the validation cohort IRONMET. Fold change associated with a unit change in the YFAS score and log10 p values adjusted for multiple testing are plotted for each family. All analyses were performed controlling for age, waist circumference, sex (only when individuals of both sexes were included in the analysis), and education years as covariates.
Extended Data Fig. 4 Gut microbiome and YFAS in IRONMET-CGM.
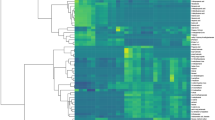
a–i) ANCOM-BC microbiome differential abundance (two-sided Z-test using the statistic W = log2Fold Change/standard error) volcano plot at the phylum level for a) YFAS motivation, b) YFAS persistence, c) YFAS compulsivity for the discovery cohort IRONMET-CGM; d) YFAS motivation, e) YFAS persistence, f) YFAS compulsivity for women of the discovery cohort IRONMET-CGM; g) YFAS motivation, h) YFAS persistence, i) YFAS compulsivity for men of the discovery cohort IRONMET-CGM. Fold change associated with a unit change in the YFAS score and log10 p values adjusted for multiple testing are plotted for each family. Heat map of two-sided Spearman’s correlations between iqlr-transformed abundances of Gokushovirus WZ-2015a and YFAS, addiction-like criteria (motivation, persistence, compulsivity) and sensitivity to reward (SPSR) and punishment (NU (UPPS)) for j) women and k) men. All analysis were performed controlling for age, BMI, sex, and education years as covariates.
Extended Data Fig. 5 Gut microbiome and Stroop Colour-Word Test and fMR metastability parameters associated with Gokushovirus.
a) ANCOM-BC differential abundance (two-sided Z-test using the statistic W = log2Fold Change/standard error) plot at the family level for the Stroop Colour-Word Test – Word Colour (SCWT-WC) controlling for age, BMI, sex, and education years as covariates in men from the Aging Imageomics cohort (n = 475). Fold change associated with a unit change in the SCWT-WC score and log10 p values adjusted for multiple testing are plotted for each family. b, c) SHAP summary plot for the metastability in the resting-state networks associated with the iqlr-transformed Gokushovirus WZ-2015a levels identified through the Boruta algorithm after controlling for age, BMI, sex (only when applicable), and education level in the whole b) cohort and c) men, respectively. Each dot represents an individual sample. The X-axis represents the SHAP value: the impact of a specific resting-state network on the iqlr-transformed Gokushovirus WZ-2015a levels prediction of a specific individual. Features are sorted in decreasing order based on their overall importance for final prediction (average SHAP values shown in bold).
Extended Data Fig. 6 Metabolomics of nucleus accumbens in recipient mice according to the presence of Gokushovirus in donor’s microbiota.
a) Dot-plot of HMDB pathways enrichment in the NAc of recipient mice from metabolites significantly associated with the presence or absence (<10 counts) of Gokushovirus WZ-2015a from the human donor’s microbiota. b) Metabolite concept network depicting significant metabolites involved in the selected pathways. c) Volcano plot of metabolites identified in the DS of the recipient mice according to the presence or absence (<10 counts) of Gokushovirus WZ-2015a in the human donor’s microbiota using robust linear regression models (t-statistic based on M-estimation with Huber weighting solved using Iteratively Reweighted Least Squares) controlling for donors age, sex, BMI, and education years. Fold change and log10 p values adjusted for multiple comparisons are plotted. d) Dot-plot of KEGG enriched pathways in the DS of recipient mice from metabolites significantly associated with the presence or absence (<10 counts) of Gokushovirus WZ-2015a from the human donors microbiota. e) Metabolite concept network depicting significant metabolites involved in the selected pathways.
Extended Data Fig. 7 Genes expressed in the medial prefrontal cortex of recipient mice according to the presence of Gokushovirus in donor’s microbiota.
a) Dot-plot of KEGG enriched pathways in the mPFC of recipient mice from genes significantly downregulated with the presence or absence (<10 counts) of Gokushovirus WZ-2015a from the human donor’s microbiota. b) Dot-plot of GO biological processes enrichment analysis from genes significantly downregulated with the presence or absence (<10 counts) of Gokushovirus WZ-2015a from the human donor’s microbiota in the mPFC of recipient mice. c) Gene concept network depicting significant genes involved in the selected metabolic processes.
Extended Data Fig. 8 Microbiome families associated with the presence of food addiction and differential metabolites between the AA and control mice in the Nucleus accumbens.
Volcano plot of differential microbiome families associated with the presence of food addiction in a) all individuals (n = 147) and in b) women (n = 101) identified using ANCOM-BC (two-sided Z-test using the statistic W = log2Fold Change/standard error) controlling for age, sex (only when individuals of both sexes were included in the analysis), and waist circumference. Fold changes and p values adjusted for multiple testing are plotted. c) Dot plot of significant (q-values < 0.1) over-represented (one-sided hypergeometric test) HMDB pathways identified from significantly differential metabolites between the AA and control mice in the NAc. d) Dot plot of KEGG module-based pathway over-representation analysis (one-sided hypergeometric test) based on the molecular function significantly associated with the iqlr-transformed Gokushovirus WZ-2015a levels identified using fastANCOM (padj<0.05). e) Metabolite concept network depicting significant metabolites involved in the selected pathways.
Extended Data Fig. 9 Metabolites associated with YFAS.
a) Volcano plot of metabolites associated with YFAS identified employing robust linear regression models (t-statistic based on M-estimation with Huber weighting solved using Iteratively Reweighted Least Squares) in the IRONMET-CGM cohort adjusting for age, sex, BMI, years of education. b) Scatter-plots (two-sided partial Spearman’s rank correlation test adjusted for age, BMI, sex and education years) between 3-ethilmalic acid and YFAS residuals. Scatter-plots show tendency line with 95% confidence interval, each dote represent and independent participant. c) Dot-plot of KEGG enriched pathways (one-sided hypergeometric test) from metabolites significantly associated with YFAS in IRONMET-CGM cohort. P values were corrected for multiple testing using the Storey correction (q-values). d) Metabolite concept network depicting significant metabolites involved in the selected pathways. e) Dot plot of significantly over-represented (one-sided hypergeometric test) HMDB pathways identified from significantly differential metabolites associated with YFAS identified in the IRONMET-CGM. P values were corrected for multiple testing using the Storey correction (q-values). f) Metabolite concept network depicting significant metabolites involved in the selected pathways.
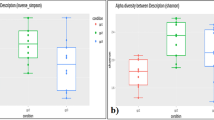
Extended Data Fig. 10 Experiments of food addiction in Drosophila.
a–c) Cumulative plot of the PI over time. The middle line represents the mean and the shading the S.E.M and Cumulative PI at 40 min of flies choosing between a 5% sucrose or 5% sucrose food + 15% ethanol. Flies expressing impTNT or TNT in the dopaminergic neurons by means of the ple-Gal4 promoter with and without dietary supplementation of AA (200 mg/L). PI ranging from −1 to +1, positive values indicate a preference for ethanol and negative values indicate preference for sucrose (PimpTNT-TNT < 0.0001). The graph represents data from a minimum of 3 independent experiments. Bar graphs represent mean with S.E.M. Significance was calculated using Mann–Whitney test (****p < 0.0001). d) Gene–gene interaction network (minimum confidence score > 0.15) constructed using differentially expressed mPFC genes (abs(logFC>1), pFDR<0.2) via the Search Tool for the Retrieval of Interacting Proteins/Genes (STRING) database. The network nodes are genes and the edges represent the predicted functional interactions. The thickness indicates the degree of confidence prediction of the interaction. e) Dot plot of GO BP, CC and MF over-representation analysis (one-sided hypergeometric test) of differentially expressed mPFC genes according to the presence or absence (<10 counts) of Gokushovirus WZ-2015a in the human donor’s microbiota. P values were corrected for multiple comparisons using the Storey correction (q-value). f) Gene-concept network depicting the connections of those genes involved in the GO biological process, cellular compartment and molecula function over-representation results. g) Gene-concept network depicting the connections of those genes involved in the KEGG-based over-representation results.
Supplementary information
Supplementary Information
IRONMET-CGM protocol.
Supplementary Tables
The file contains Supplementary Tables 1–75.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Castells-Nobau, A., Puig, I., Motger-Albertí, A. et al. Microviridae bacteriophages influence behavioural hallmarks of food addiction via tryptophan and tyrosine signalling pathways. Nat Metab 6, 2157–2186 (2024). https://doi.org/10.1038/s42255-024-01157-x
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s42255-024-01157-x
This article is cited by
-
Gut virome dynamics: from commensal to critical player in health and disease
Nature Reviews Gastroenterology & Hepatology (2026)
-
Gut phages fuel food addiction
Nature Reviews Microbiology (2025)
-
Viewing Psychiatric Disorders Through Viruses: Simple Architecture, Burgeoning Implications
Neuroscience Bulletin (2025)