Abstract
Invasive Lobular Carcinoma (ILC), a distinct subtype of breast cancer, is hallmarked by E-Cadherin loss, slow proliferation, and strong hormone receptor positivity. ILC faces significant challenges in clinical management due to advanced stage at diagnosis, late recurrence, and development of resistance to endocrine therapy - a cornerstone of ILC treatment. To elucidate the mechanisms underlying endocrine resistance in ILC, ILC cell lines (MDA-MB-134-VI, SUM44PE) were generated to be resistant to tamoxifen, a selective estrogen receptor modulator. The tamoxifen-resistant (TAMR) cells exhibit a 2-fold increase in tamoxifen IC50 relative to parental cells. Metabolomics and RNA-sequencing revealed deregulation of alanine, aspartate, and glutamate metabolism, purine metabolism, and arginine and proline metabolism in TAMR cells. Among the fifteen commonly dysregulated genes in these pathways, low argininosuccinate synthase (ASS1) expression was identified in the TAMR cells and was significantly correlated with poor outcome in ILC patients, specifically in the context of endocrine therapy. Our study reveals methylation-mediated silencing of ASS1 in TAMR cells as a likely mechanism of downregulation. Demethylation restored ASS1 expression and correspondingly reduced tamoxifen IC50 toward parental levels. Nucleic acid biosynthesis is augmented in TAMR cells, evidenced by an increase in nucleotide intermediates. Both TAMR cell lines demonstrated increased expression of several nucleic acid biosynthesis enzymes, including PAICS, PRPS1, ADSS2, CAD, and DHODH. Furthermore, CAD, the key multifunctional protein of the de novo pyrimidine biosynthesis pathway, is differentially activated in TAMR cells. Treating TAMR cells with Decitabine, a demethylating agent, or Farudodstat, a pyrimidine biosynthesis inhibitor, markedly augmented the efficacy of tamoxifen. Collectively, our study unveils ASS1 downregulation as a novel mechanism underlying acquired tamoxifen resistance in ILC and establishes a metabolic link between ASS1 and nucleic acid biosynthesis. Restoring ASS1 expression or inhibiting pyrimidine biosynthesis reinstated tamoxifen sensitivity. ASS1 could be a potential biomarker and therapeutic target in tamoxifen-resistant ILC patients, warranting further investigation.
Similar content being viewed by others
Introduction
Invasive lobular cancer (ILC) is a distinct histological and molecular subtype accounting for ~15% of all breast cancers and is the second most common subtype of invasive breast cancer after invasive ductal carcinoma (IDC) [1, 2]. Typically, ILC is estrogen receptor (ER) positive, progesterone receptor (PR) positive, and human epidermal growth factor receptor 2 (HER2) negative with a low mitotic index. Loss of E-cadherin is a hallmark of ILC, which contributes to the unique morphology, frequent multifocality, and characteristic metastatic pattern to serosa, including ovaries, gut, and peritoneum [3,4,5]. Patients with ILC face delayed and higher stage at diagnosis, and long-term worse disease-free and overall survival [6, 7]. While endocrine therapy remains the cornerstone in the treatment of ILC, one of the greatest hurdles in the management of ILC is resistance to endocrine therapy, leading to late recurrences [8]. Though a prevalent subtype, ILC remains relatively understudied and is frequently grouped with ER/PR positive IDC; consequently, ILC management, including screening, treatment, and follow-up strategies, is largely based on data from IDC. Hence, there is an unmet need to address the mechanisms underlying endocrine resistance in ILC and develop strategies to overcome resistance.
Tamoxifen, a selective estrogen receptor modulator (SERM), is a cornerstone in endocrine therapy for premenopausal (and certain postmenopausal) women with estrogen receptor-positive (ER+) breast cancer [9]. There is active clinical development of novel SERMs, such as lasofoxifene [10, 11], and bazedoxifene [12]. However, one-third of the patients with ER+/PR+ tumors fail to respond to initial tamoxifen treatment, with many relapsing later [13, 14]. The development of tamoxifen resistance, studied predominantly in IDC is a complex phenomenon, involving an interplay of diverse cellular processes and signaling pathways, including upregulation of receptor tyrosine kinase activity leading to activation of ERK and PI3K pathway, altered expression of ERα and ERβ expression [15] and increased expression of miR-221/222 targeting p27/Kip1 [16]. Recent studies demonstrate alteration of cellular metabolism as an important mechanism underlying the development of drug resistance [17,18,19,20]. Metabolic plasticity in cancer cells allows hijacking and remodeling of existing metabolic pathways to foster cancer cell growth and survival, impacting drug response [21]. For example, a recent study using tumor and adjacent normal tissues from IDC patients revealed distinct enrichment of one-carbon metabolites in IDC tumors [22], yet similar metabolomic analysis of ILC cell lines and their endocrine-resistant derivatives is limited.
To address these key gaps in ILC biology and therapeutic resistance, we developed and characterized tamoxifen-resistant ILC cell lines through concurrent transcriptional and metabolomic profiles with a goal to identify and characterize candidate therapeutic targets and biomarkers toward improved outcomes for ILC.
Results
Tamoxifen-resistant ILC cell lines
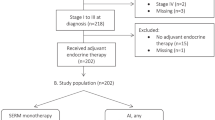
Tamoxifen-resistant (TAMR) cells were generated from two commercially available invasive lobular carcinoma (ILC) cell lines, MDA-MB-134-VI (MB134) and SUM44PE (SUM44). The MB134TAMR cells demonstrated marked morphological changes, with parental MB134 cells growing as a loosely adherent monolayer, while the MB134TAMR cells grown routinely in 100 nM 4-hydroxytamoxifen (4-OHT) acquired a more cuboidal shape and formed larger adherent patches (Fig. 1A). SUM44 and SUM44TAMR cells had similar appearance growing as individually dispersed cells, with SUM44TAMR reflecting an increased proportion of cells with spindle like morphology, grown routinely in 500 nM 4-OHT (increased concentration of 4-OHT due to inherent SUM44 tolerance).
A Phase contrast light microscopy images of parental and tamoxifen-resistant ILC cells with magnified images in the inserts. B Growth kinetics of parental and tamoxifen-resistant MB134 (upper panel) and SUM44 (lower panel) cell lines. Fold change in growth normalized to day 0 at each time point over 72 h. C Dose response to tamoxifen in MB134 and MB134TAMR cells (upper panel) and SUM44 and SUM44TAMR cells (lower panel). Overnight cultures of exponentially growing cells were treated with vehicle or drugs for 5 days. IC50 for TAM was calculated using GraphPad Prism 10. D Transwell Boyden chamber assays comparing the migratory capabilities of parental vs. TAMR, MB134 (upper panel) and SUM44 (lower panel) cell lines. The area covered by migrated cells was quantified in the bar diagram. E Representative image of western blot and densitometry analysis of ERα and HER2 levels in parental vs. TAMR ILC cells. GAPDH was used as a loading control. Representative of three independent experiments is presented in the figures. Statistical differences between groups were evaluated using Student’s t-test. Significance levels are indicated as follows: **p ≤ 0.01, *p < 0.05. P Parental, TAMR Tamoxifen Resistant.
Comparison of growth kinetics demonstrated a significant increase in the growth rate of TAMR cells relative to parental cells (MB134: p = 0.008, SUM44: p = 0.005) (Fig. 1B). In addition, TAMR cells showed >2-fold increase in the half-maximal inhibitory concentration (IC50) for tamoxifen compared to their respective parental counterparts (Fig. 1C), confirming functional tamoxifen resistance. Specifically, tamoxifen IC50 values were 8.4 μM and 16.3 μM for MB134 and MB134TAMR, respectively, and 11.15 μM and 27.3 μM for SUM44 and SUM44TAMR cells, respectively. This was further confirmed using the direct cell counting method, where both TAMR cells showed a similar increase in IC50 for tamoxifen compared to their parental counterpart (Supplementary Fig. S1A). Both TAMR cells demonstrated increased migration compared to the corresponding parental cells over 120 h after seeding the cells, with MB134TAMR 4-fold increase (p = 0.04, Fig. 1D) and SUM44TAMR 1.2-fold increase relative to the corresponding parental cells (p = 0.046, Fig. 1D). To determine if faster growth rate of TAMR cells compared to parental cells is contributing to the increase in migration observed in the TAMR cells, migration assay was performed for a shorter duration of time (72 h). The shorter-duration assay consistently showed marked enhancement of migration of both TAMR cells relative to the corresponding parental cells (MB134 vs. MB134TAMR p = 0.02, and for SUM44 vs. SUM44TAMR p = 0.02) (Supplementary Fig. S1B). This data further supports our conclusion that there is a significant enhancement in the invasive potential of the TAMR cells. To evaluate if these changes were mediated through canonical breast cancer receptor expression, Western blot analysis revealed comparable ERα protein levels, but TAMR cell lines expressed higher levels of HER2 than the parental lines (Fig. 1E): MB134TAMR line showed a 4-fold increase, and SUM44TAMR had a 2-fold increase in HER2 expression.
Collectively, these data show that TAMR cells reflect morphological, phenotypic, and molecular changes relative to parental cell lines.
Metabolic alterations associated with tamoxifen resistance in ILC cell lines
To elucidate the molecular changes associated with tamoxifen resistance in ILC, we subjected parental and TAMR derivatives of MB134 and SUM44 cell lines to metabolic profiling. Untargeted metabolomics profiling, involving comprehensive compound identification through databases like the Human Metabolite Database (HMDB) and an in-house high-resolution mass spectra database, was conducted on metabolites extracted from our representative cell lines. Using the polar metabolites fraction, we identified 120 metabolites across all samples with a QC coefficient of variation <20%. Partial Least Squares Discriminant Analysis (PLS-DA) was performed to summarize the overall metabolic differences between the cell phenotypes. Distinct and tight clustering of the experimental groups suggests distinct metabolic profiles pertaining to each cell line (Supplementary Fig. S2A). A heatmap was used to summarize the relative abundance of each metabolite across our queried cell lines (Supplementary Fig. S2B), where it became evident that the unique histological origin contributed to the metabolic uniqueness of each cell pair. Taking the abundance of unique metabolites in each pair of cell lines (parental vs. TAMR) into consideration, we chose to first analyze each pair separately. PLS-DA was thus performed to observe the metabolic differences of SUM44 parental vs. SUM44TAMR cells. Figure 2A shows the independent clustering of SUM44 parental vs. SUM44TAMR cells, where the model exhibited an R2 value of 0.99 and a Q2 score of 0.97, suggesting good model fit and predictive capability, respectively [23]. Our finding suggests that the acquired tamoxifen resistance contributes to a deregulated metabolic profile distinct from the parental line. Herein, a VIP plot highlights the top 15 deregulated metabolites driving separation of the PLS-DA model (Fig. 2B). Phosphocreatine, 5-amino levulinate, and N-acetyl aspartic acid were the top deregulated metabolites across the SUM44 cell pairs. Importantly, many nucleotides and their derivatives, namely cytidine, uridine monophosphate, uridine diphosphate (UDP)-N-acetyl-D-galactosamine, and UDP-xylose, were among the top deregulated metabolites driving the separation of the PLS-DA model. The metabolic differences of the MB134 cell pair were also probed using a similar analysis, where a PLS-DA model demonstrated independent clustering of MB134 parental and MB134TAMR counterparts with an R2 value of 0.99 and a Q2 score of 0.95, indicating good model fit and predictive ability, respectively (Fig. 2C) [23]. The metabolites driving the separation of the MB134 cell pair are depicted in the VIP plot in Fig. 2D, where UDP-xylose, cytidine 5′-triphosphate, and D-glucosamine 6-phosphate were identified as the top metabolites driving the separation of the PLS-DA model. Collectively, our findings corroborate the notion that acquired resistance contributes to an aberrant metabolic profile.
A Partial Least Squares Discriminant Analysis (PLS-DA) showing metabolic differences between parental and tamoxifen-resistant SUM44 cell pair. B Variable Importance in Projection (VIP) plot highlighting the top 15 metabolites driving the separation between the parental and resistant SUM44 cell pair. C PLS-DA showing metabolic differences between parental and tamoxifen-resistant MB134 cell pair. D VIP plot highlighting the top 15 metabolites driving the separation between the parental and resistant MB134 cell pair. E Overlap of altered pathways in parental vs. tamoxifen-resistant SUM44 and MB134 pairs, represented by impact scores. F Venn diagram illustrating the number of shared and unique pathways altered in SUM44 and MB134 cell pairs, indicating common metabolic changes associated with tamoxifen resistance. G Significantly deregulated KEGG pathways in parental vs. tamoxifen-resistant MB134 cells and H SUM44 cells as determined by RNA sequencing analysis of cell pairs in quadruplicate. I Venn diagram showing the overlap of 52 deregulated pathways between parental and tamoxifen-resistant pairs of SUM44 and MB134 cell lines. J Venn diagram showing the overlap of metabolomic and transcriptomic data, identifying three mutually deregulated pathways in SUM44 and MB134TAMR cells. K Venn diagram showing the overlap of 15 genes within the three mutually deregulated pathways. L Gene-metabolite interaction map illustrating interactions between three deregulated pathways. Circles denote genes and squares denote metabolites.
Systemically, quantitative enrichment analysis uncovered 14 significantly altered pathways that were associated with the acquired tamoxifen resistance in our SUM44 cell pair [–log(p) value >1.32 and pathway impact >0.2]. In comparison, the analysis uncovered 13 significantly altered pathways that were associated with the acquired tamoxifen resistance in the MB134 cell pair. The pathways included alanine, aspartate and glutamate metabolism, tyrosine metabolism, glycine, linoleic acid metabolism, purine metabolism, lysine degradation, arginine biosynthesis, arginine and proline metabolism, as well as D-glutamine and D-glutamate metabolism (Fig. 2E). A full list of the significantly deregulated pathways between our queried cell pairs is summarized in Supplementary Table 1. To investigate mutually deregulated metabolic processes driven by acquired tamoxifen resistance, we identified 10 mutually deregulated pathways between the TAMR and parental cell lines (Fig. 2F & Table 1). The pathways deregulated in both the cell lines were predominantly amino acid metabolism pathways, such as alanine, aspartate, and glutamate metabolism, arginine biosynthesis, and lysine degradation, but also included nucleotide metabolic processes such as the purine metabolism pathway. Importantly, identification of shared metabolic changes across both ILC cell pairs identifies the prominent metabolic processes consistently altered as a result of acquired tamoxifen resistance.
Altered nucleic acid and amino acid pathways associated with tamoxifen resistance
To further validate the observed metabolic alterations and delineate the underlying metabolic rewiring, we subjected all four cell lines to RNA-seq transcriptomic analysis. The volcano plots show the differentially expressed genes between the SUM44 pair (Supplementary Fig. S3A) and the MB134 pair (parental vs. TAMR) (Supplementary Fig. S3B). The genes deregulated in our RNA-seq data were subjected to Gene Set Enrichment Analysis (GSEA). A total of 30,000 genes were analyzed, and gene sets were mapped to the KEGG database. In line with our metabolomics analysis, transcriptomic data were analyzed separately for each pair of cell lines. Significantly altered pathways were identified with a cut-off of FDR < 0.2 for significance for both MB134 cell pairs and SUM44 cell pairs, where up to the top 14 pathways are shown in Fig. 2G, H, respectively. Mutually altered pathways across both cell pairs were next analyzed, with 52 pathways identified to be significantly deregulated as a result of acquired tamoxifen resistance (Fig. 2I). A subset of the pathways deregulated in both MB134TAMR and SUM44TAMR cells is highlighted in Table 2.
To further enable mechanistic understanding, an integrated analysis of both metabolomics and transcriptomics revealed that only three mutually deregulated metabolic pathways exhibited similar alterations in both parental and TAMR ILC cells (across both of our metabolomics and transcriptomics datasets): (1) alanine, aspartate, and glutamate metabolism (AAG); (2) purine metabolism; and (3) arginine and proline metabolism (Fig. 2J). To further investigate these metabolic changes and to confirm the observed trend in tamoxifen-resistant cells, we identified genes overlapping in all dysregulated pathways. While a single gene was not at the intersection of all three pathways, 15 genes were found to partake in at least 2 unique metabolic processes Fig. 2K. There were 4 gene overlaps between AAG and the Purine metabolism pathway, namely ADSS1, ADSS2, ADSL, and PPAT. Additionally, there were 11 genes that overlapped between AAG and Arginine & proline metabolism pathways, namely, ALDH4A1, ASS1, ASL, CPS1, GLS, GLS2, GLUL, GLUD1, GLULD2, GOT1, GOT2 (Supplementary Table 2). As these genes partake in an intricate metabolic network, a gene-metabolite interaction map between our three deregulated pathways was mapped in Fig. 2L to investigate potential association with tamoxifen resistance. This analysis provides a comprehensive view of the molecular landscape associated with tamoxifen resistance in ILC cell lines, with ASS1 (Argininosuccinate Synthase 1) emerging as one of the central players in the observed metabolic and transcriptomic alterations connecting amino acid and nucleotide biosynthesis. Collectively, the integration of our unbiased analyses was able to identify 3 unique metabolic pathways directly associated with tamoxifen resistance at both the metabolite and transcript level. Overlap of the genes within the deregulated pathways identified 15 mutually expressed genes across at least 2 pathways, where ASS1 was determined to be one of the central metabolic hubs within this aberrant metabolic network. ASS1 is a key enzyme in the urea cycle, synthesizing argininosuccinate from aspartate and citrulline. Downregulation of ASS1 could lead to metabolic diversion of aspartate towards nucleic acid biosynthesis, fostering cell proliferation.
Methylation-mediated downregulation of ASS1 is associated with tamoxifen resistance in ILC cell lines
Transcriptomics data revealed a significant downregulation of ASS1 expression in both MB134TAMR (95%, p = 0.01) and SUM44TAMR cells (90%, p = 0.019); (Fig. 3A). This finding was further confirmed in three independent biological replicates by qRT-PCR, where consistent decrease in ASS1 mRNA levels in TAMR cells (MB134TAMR: 40%, p < 0.0001 and SUM44TAMR: 73%, p < 0.0001) compared to the respective parental cells were observed (Fig. 3B). We also evaluated ASS1 expression in ILC cells grown long-term in estrogen deprived (LTED) medium. The MB134-LTED and SUM44-LTED cells grown in the absence of estrogen demonstrated resistance to tamoxifen [24]. Interestingly, two different clones of LTED cells derived from each ILC cell lines showed a significant decrease in ASS1 expression (MB134-LTED: >90%, p < 0.0001, SUM44-LTED: 90%, p < 0.0001; Fig. 3B). Marked reduction of ASS1 protein (60–90%) was observed in TAMR and LTED cells compared to the corresponding parental cell lines (all p < 0.05, Fig. 3C). This observation raises the possibility that estrogen may play a regulatory role in modulating ASS1 expression, although comparable ERα protein levels (as shown in Fig. 1C).
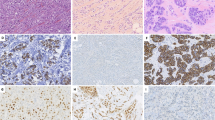
A Comparative expression of ASS1 in parental (P) and tamoxifen-resistant (TAMR) ILC cell lines as determined by change in Fragments Per Kilobase of transcript per Million mapped reads (FPKM) obtained from RNA-seq data. B qRT-PCR analysis showing ASS1 expression, and C western blot and densitometry analysis showing ASS1 protein levels in MB134 and SUM44 cells, their respective tamoxifen-resistant and LTED derivatives (LTEDA and LTEDB). D Schematic diagram showing the CpG island in the ASS1 promoter. E Analysis of the ASS1 promoter region using MSPCR showing amplification of 150 bp methylated DNA in TAMR and LTED derivatives of ILC cell lines and 147 bp unmethylated DNA in parental ILC cell lines. F qRT-PCR analysis showing ASS1 expression in MB134TAMR and SUM44TAMR cells that are either left untreated (UT) or treated with 5 μM 5-aza-2′-deoxycytidine (dAzaC) for 120 h. G Western blot and densitometry analysis showing ASS1 protein levels in MB134TAMR and SUM44TAMR cells after 120 h of dAzaC treatment (n = 2 experiments). Error bars represent the standard deviation of triplicates. Significance levels are indicated as follows: ****p < 0.0001 ***p ≤ 0.001, **p ≤ 0.01, *p < 0.05.
We next investigated the mechanism underlying the silencing of ASS1 in TAMR ILC cells. Computational analysis revealed the presence of a CpG island in the 5′ regulatory region of the ASS1 gene spanning from −499 bp to −6 bp with +1 as the transcription start site (Fig. 3D). Methylation-specific PCR (MSPCR) using methyl CpG-specific primers led to amplification of a 150 bp product from TAMR and LTED cell DNA but not from parental cell DNA. Use of primers specific for unmethylated DNA led to amplification of a 147 bp product from parental cell DNA, but not from TAMR and LTED cell DNA (Fig. 3E). Our data demonstrate methylation of the ASS1 promoter in TAMR and LTED cells but not in the parental counterparts.
To determine if treatment with a demethylating agent would reverse methylation at this specific 5′ regulatory region of the ASS1 gene and enhance expression of ASS1, TAMR cells were treated with the established demethylating agent decitabine (5-aza-2′-deoxycytidine, dAzaC) at 5 μM. When treated for 120 h, MB134TAMR cells showed a 12-fold increase (p < 0.0001), and SUM44TAMR cells showed a 3-fold increase (p = 0.01) in ASS1 mRNA, compared to untreated cells (Fig. 3F). Similarly, a 72-fold and ~2-fold increase of ASS1 protein in dAzaC-treated MB134TAMR (p = 0.0078) and SUM44TAMR (p = 0.01) cells respectively were observed (Fig. 3G). These data support the notion that methylation of the CpG island in the ASS1 promoter contributes to its downregulation in tamoxifen-resistant cells.
To determine if ASS1 downregulation is sufficient to mediate tamoxifen resistance, we knocked down ASS1 in MB134 and SUM44 cells using two independent shRNAs (TRCN0000045554 and TRCN0000045553) and generated shASS1 and shASS1a cells. In MB134-shASS1 cells, there was a 50% reduction in ASS1 mRNA (p = 0.0012), and protein was barely detectable (p = 0.0003), whereas in SUM44-shASS1 cells 80% reduction in both mRNA (p < 0.0001) and protein (p = 0.0001) levels was observed (Fig. 4A, B). A 1.85-fold reduction in ASS1 expression (p = <0.0001) was noted in the MB134-shASS1a cells compared to the control cells (pLKO), while the SUM44-shASS1a exhibited a 3.55-fold decrease in ASS1 expression (p = <0.0001) (Supplementary Fig. S4A, B). The shASS1 cells demonstrated increased tolerance to tamoxifen as evidenced by an increase in IC50 values for tamoxifen compared to the parental cells. For MB134 cells, IC50 values are 9.56 µM vs. 15.28 µM in pLKO vs. shASS1 cells (p = 0.0117), and for SUM44 cells the values are 11.77 µM vs. 18.85 µM in pLKO vs. shASS1 cells (p = 0.008) (Fig. 4C). Similarly, for the second set of ASS1 knockdown cells, IC50 values are 9.87 µM vs. 16.09 µM for MB134-pLKO vs. MB134-shASS1a cells (p = 0.024), and the values are 12.58 µM vs. 17.69 µM for SUM44- pLKO vs. SUM44-shASS1a cells (p = 0.026) (Supplementary Fig. S4C). In addition, we have observed a small but significant increase in growth rate when ASS1 is knocked down in the ILC cell lines (Fig. 4D, MB134: pLKO vs. shASS1, p = 0.04 and SUM44: pLKO vs. shASS1, p = 0.03; Supplementary Fig. S4D, MB134: pLKO vs. shASS1a, p = 0.0011 and SUM44: pLKO vs. shASS1a, p = 0.01). These findings suggest that reduced expression of ASS1 promotes cell growth and resistance to tamoxifen.
MB134 and SUM44 cells were transduced with plasmids expressing shRNA targeting ASS1 or the corresponding empty vector to produce shASS1 and control (pLKO) cell lines. A qRT-PCR analysis showing ASS1 expression, and B Western blot and densitometry analysis of ASS1 protein levels in ASS1 knockdown (shASS1) vs. pLKO (control) MB134 and SUM44 cell lines. C Dose response to tamoxifen and IC50 of tamoxifen in ASS1 knockdown (shASS1) vs. pLKO (control) MB134 (left panel) and SUM44 cell lines (right panel), assessed using the automated cell counting method. D Comparison of growth kinetics of shASS1 vs. pLKO derivatives of MB134 (left panel) and SUM44 cell lines (right panel). Fold change in growth is normalized to day 0 at each time point over 72 h. E Overall survival analysis of all breast cancer patients in relation to ASS1 expression using the METABRIC dataset. F Overall survival analysis of ILC patients who received endocrine therapy in relation to ASS1 expression using the METABRIC dataset. G Overall survival analysis of breast cancer patients who received endocrine therapy in relation to ASS1 expression using the K–M plotter dataset. ****p < 0.0001, ***p ≤ 0.001, **P ≤ 0.01, *p < 0.05.
To determine the significance of ASS1 downregulation in breast cancer patients with respect to disease outcome, we used publicly available datasets. Using the METABRIC dataset, we found that elevated ASS1 expression (upper quartile) is prognostic of poor overall survival (OS), when all subtypes were considered (Fig. 4E, p = 0.001), suggesting our findings are not generalizable to all breast cancer subtypes together. Although previous literature has suggested a tumor suppressive role for ASS1, we confirmed a direct correlation between high ASS1 and poor OS in the GSE25066 dataset [25], and others have confirmed this in the TCGA BRCA dataset [26] (Supplementary Fig. S4E, F). When we specifically analyzed ILC patients treated with endocrine therapy (the focus of this study), low ASS1 expression (lower quartile) was prognostic of poor OS (Fig. 4F, p = 0.04). We also evaluated all endocrine-treated breast cancer patients in METABRIC, and ASS1 was not predictive of OS (data not shown). Thus, our analysis shows that low ASS1 expression, associated with tamoxifen resistance experimentally, is associated with worse survival among endocrine therapy-treated patients and, specifically, endocrine therapy-treated patients with ILC. To evaluate an orthogonal dataset, we used the K–M Plotter dataset to analyze the correlation between ASS1 expression and OS of breast cancer patients who received endocrine therapy and observed that lower ASS1 expression was associated with worse OS (Fig. 4G, p = 0.022). We believe these data support our other work highlighting that low ASS1 is associated with increased tamoxifen resistance, indicated by decreased survival of low ASS1 expressing patients treated with endocrine therapy.
Nucleic acid biosynthesis and pathway intermediates in tamoxifen-resistant ILC cells
Aberrant metabolism of amino acids and one-carbon units in cancers is acknowledged contributor to nucleic acid synthesis, fostering proliferative signaling, resistance to cell death, and metastasis [27]. Purine metabolism is one of the three pathways that were found to be mutually deregulated in both TAMR cells in our multi-omics analysis (Fig. 2J). When subjected to metabolomic analysis, ASS1 knockdown and the respective control cells (shASS1 vs. pLKO) derived from MB134 and SUM44 cell lines showed independent clustering (Supplementary Fig. S5A, C). The VIP plots highlight the top metabolites driving the separation of the ASS1 knockdown vs. the control cells (Supplementary Fig. S5B, D). Importantly, similar enrichment of purine metabolism was observed in both MB134 (p = 0.003) and SUM44 (p = 0.0008) cells upon ASS1 knockdown (Fig. 5A, B). In addition, the observed enrichment of alanine, aspartate, and glutamate metabolism in SUM44-shASS1 cells suggests an association between ASS1 downregulation and metabolic pathways altered in TAMR cells. Our untargeted metabolomics analysis uncovered changes in intermediates of nucleotide metabolism upon acquiring tamoxifen resistance. In particular, we noticed an increase in intracellular abundance of the purine intermediates deoxyguanosine-monophosphate (dGMP) (p = 0.03), guanosine diphosphate (GDP) (p = 0.03) and guanosine monophosphate (GMP) (p = 0.02) (Fig. 5C). Additionally, an increase in the pyrimidine intermediate cytosine monophosphate (CMP) was also evident in the MB134TAMR cells (p = 0.002) (Fig. 5D). Similarly, in SUM44TAMR cells, we observed small but significant increase in ADP (p = 0.009) and ATP (p = 0.05), as well as an elevation in cytosine level (p = 0.0006) (Fig. 5E, F).
A Significantly enriched metabolic pathways in shASS1 vs. pLKO derivatives of MB134 and B SUM44 cell lines. C Changes in the levels of purine (dGMP, dGDP, GDP, GMP, IMP) and D pyrimidine (UDP, UMP, and CMP) nucleotides in parental (P) vs. tamoxifen-resistant (TAMR) MB134 cells. E Changes in the levels of purine (ATP and ADP, dGTP, GDP) and F pyrimidine (Cytosine, UMP) nucleotides in parental (P) vs. tamoxifen-resistant (TAMR) SUM44 cells. G Expression levels of PRPS1, H PAICS, and I DHODH in MB134 and SUM44 cell pairs as analyzed from RNA-seq data. (FPKM: Fragments Per Kilobase Per Million reads). J Representative picture of pCADS1859 (pCAD) levels in parental and TAMR cells and K in control (pLKO) vs. shASS1 derivatives of MB134 and SUM44 cell pairs. Bar diagrams show the average of more than one independent experiment (n = 2). ****p < 0.0001, ***p ≤ 0.001, **P ≤ 0.01, *p < 0.05.
Using the transcriptomics data, we next investigated if expression of additional genes involved in purine and pyrimidine synthesis pathways is altered in TAMR cells. We observed significant upregulation of PRPS1 (phosphoribosyl pyrophosphate synthetase 1) in MB134TAMR (p = 0.0008) and SUM44TAMR cells (p = 0.017) when compared to the respective parental cells (Fig. 5G). Phosphoribosyl pyrophosphate is essential for both the de novo and salvage pathways of purine and pyrimidine biosynthesis. Additionally, we found PAICS (phosphoribosylaminoimidazole carboxylase and phosphoribosylaminoimidazolesuccincarboxamide synthase) converting carboxyaminoimidazole ribonucleotide (CAIR) to N-Succinocarboxyamide-5-aminoimidazole ribonucleotide (SAICAR), an intermediate of purine biosynthesis, to be significantly upregulated in both MB134TAMR (p = 0.015) and SUM44TAMR cells (p = 0.01) (Fig. 5H). Furthermore, there is significant increase in DHODH (dihydroorotase dehydrogenase) converting dihydroorotate to orotate, a pyrimidine biosynthesis intermediate in both MB134TAMR (p = 0.015) and SUM44TAMR cells (p = 0.01) (Fig. 5I). ADSS2 (adenylosuccinate synthase 2), a crucial enzyme for converting IMP to AMP is upregulated significantly in MB134TAMR cells (p = 0.036) but not in SUM44TAMR cells (Supplementary Fig. S6A). Collectively, multiple enzymes in the nucleotide biosynthesis pathways are upregulated in the TAMR cells.
CAD (Carbamoyl-phosphate synthase 2, Aspartate transcarbamoylase, Dihydroorotase), a key trifunctional enzyme, utilizes aspartate as substrate and executes the first three steps of pyrimidine biosynthesis. Phosphorylation at Ser1859 leads to activation of CAD. To this end, we have evaluated pCADS1859 level in parental and TAMR cells, where a 1.8-fold increase in pCAD was observed in MB134TAMR compared to MB134 cells (Fig. 5J, p = 0.0003). SUM44TAMR cells showed a trend towards an increase in pCAD, compared to SUM44 cells. When analyzed in ASS1 knockdown cells, a significant increase in pCADS1859 levels was observed in both MB134-shASS1 (1.3-fold, p = 0.003) and SUM44-shASS1 (11-fold, p = 0.036) cells compared to the control cells (Fig. 5K). A similar increase in pCADS1859 was also observed in the second ASS1 knocked down cells (shASS1a), and an increase in pCAD expression was observed in ASS1 shRNA cells compared to parental cells (Supplementary Fig. S6B). This suggests a potential link between ASS1 depletion and elevated pCAD expression, further supporting the role of ASS1 in regulating cellular pathways.
In conclusion, multiple cellular pathways are affected in the course of acquiring resistance to anti-estrogen, which promotes the proliferation of resistant cells.
Therapeutic targeting of ASS1 methylation and nucleotide biosynthesis to overcome tamoxifen resistance
Our data demonstrated methylation-mediated silencing of ASS1 that correlates with poor outcome in endocrine-treated ILC patients. We rationalized that increased expression of ASS1 by promoter demethylation will improve the efficacy of tamoxifen. To this end, TAMR ILC cells were pre-treated with 5 µM dAzaC for 120 h; untreated cells were used as controls. Subsequently, MTT assays were performed with both dAzaC pre-treated and untreated cells, exposing them to increasing concentrations of tamoxifen. Our data showed significantly higher inhibition of dAzaC pre-treated MB134TAMR when treated with 7.5 and 10 µM tamoxifen when compared to the effects on dAzaC-un-treated cells (p = 0.04 and 0.03, respectively, Fig. 6A). Similarly, SUM44TAMR cells were significantly more sensitive to 10 µM tamoxifen when compared with untreated cells (p = 0.05, Fig. 6B), suggesting this to be a potential therapeutic combination for ILC patients with acquired resistance to endocrine therapy.
A MB134TAMR and B SUM44TAMR cells were pre-treated with 5 μM dAzaC for 120 h. Untreated (vehicle) cells were used as controls. Viability of dAzaC-treated and control cells in the presence of indicated doses of tamoxifen was compared after an additional 5 days of treatment. C Comparison of cell viability after treatment of MB134TAMR and D SUM44TAMR cells with 10 μM Farudodstat (FR) alone and in combination with 15 μM tamoxifen for 5 days. Data is representative of three independent experiments conducted in triplicate for each treatment condition. E Schematic diagram showing how methylation-mediated silencing of ASS1 could lead to augmentation of purine and pyrimidine biosynthesis pathway in tamoxifen-resistant ILC cells, where the enzymes that use aspartate as substrate are highlighted. Statistical significance indicated as *p < 0.05.
Based on the observation that multiple pyrimidine biosynthesis intermediates are deregulated in TAMR ILC cells, we next examined if inhibition of de novo pyrimidine biosynthesis is an additional avenue to improve tamoxifen efficacy in endocrine-resistant ILC. Farudodstat (ASLAN003) is an FDA-approved inhibitor of DHODH, a rate-limiting enzyme for de novo pyrimidine biosynthesis. Our data showed increased DHODH expression in TAMR cells (Fig. 5I). To test the combinatorial effect of tamoxifen and farudodstat, TAMR cells were treated with farudodstat alone or in combination with tamoxifen for 120 h. Combined treatment of MB134TAMR cells with 15 μM tamoxifen and 7.5 μM farudodstat led to a 71% inhibition of cell viability. In comparison, treatment with 15 µM tamoxifen alone resulted in a 47% reduction, and 7.5 µM farudodstat alone led to a 26% reduction in cell viability. These results indicate a synergistic effect of the combined treatment, as reflected in the combination index (CI) of 0.85931 (p = 0.02, Fig. 6C). In SUM44TAMR cells, the combination resulted in synergistic inhibition as well, where a 58% inhibition in cell viability was observed (CI = 0.84613), compared to 37% and 32% inhibition by tamoxifen alone and farudodstat alone respectively (p = 0.05, Fig. 6D). This data suggests that combined targeting of nucleic acid biosynthesis and estrogen signaling could be a potential therapeutic option for ILC patients with acquired resistance to tamoxifen.
Discussion
One of the cornerstones in treating patients with ER + ILC is endocrine therapy [13, 28]. In general, ILC tumors have lower response rates to chemotherapy because of a low proliferation index. Resistance to endocrine therapy poses a major challenge in managing the disease effectively. Up to 40% of ER+ breast cancer patients’ tumors may develop tamoxifen resistance during the initial phase of treatment, with an additional 25% developing resistance over time [29]. Although the mechanisms underlying endocrine resistance have been studied extensively in ER + IDC (reviewed by Osborne et al. [30]), these two subtypes of breast cancer are distinct in terms of histo-morphology, disease progression, recurrence, and outcome, underscoring the importance of studying endocrine resistance specifically in ILC. This is the first study, to our knowledge, where a multi-omics approach was used to compare tamoxifen-resistant ILC cell lines with their parental counterpart and identify aberrations in amino acid and nucleotide biosynthesis pathways in the resistant cells. In these cells, acquired resistance to tamoxifen resulted in downregulation of ASS1, a key enzyme at the intersection of these pathways, and correlates with poor overall survival of ILC patients, specifically those who received endocrine therapy.
Our recent review highlights the studies that investigated the mechanisms of endocrine resistance in ILC [13]. Reduced expression of ERα, increased expression of estrogen-related receptor γ (ERRγ) [31], activation of AP1-dependent transcription [31, 32], frequent mutation of PTEN and PIK3CA [33], activation of SREBP1 driving lipid and cholesterol metabolism specifically in resistance to aromatase inhibitors [34, 35], and the involvement of WNT4 in estrogen-induced growth [36] have been associated with endocrine resistance in ILC. Additionally, mutations in FOXA1, a pioneer factor for ER-mediated transcription, confer endocrine resistance by increasing FOXA1 expression and activity [37].
The major challenges in studying ILC are a lack of established and authentic cell lines along with a slow growth rate of the tumor reflected in the mouse models of ILC, particularly in orthotopic models [38]. A recent study has systematically analyzed several ILC/ILC-like cell lines and identified additional cell lines harboring key molecular features of ILC [39]. These cell lines are promising for future studies. Currently, the two most used and universally accepted cell lines to study ILC are MDA-MB134-VI and SUM44PE, confirming the relevance to ILC biology and used in this study. Both these cell lines are ER+ and lack E-cadherin, harboring the most common features of ILC tumors. SUM44PE was isolated from a patient refractile to endocrine therapy and is therefore de novo resistant to endocrine therapy [40], whereas MB134 cells were isolated from the pleural fluid of a patient diagnosed with papillary mammary carcinoma, later classified as luminal subtype [38, 41]. MB134TAMR cells generated in our lab models acquired anti-estrogen resistance. Increased tolerance of the SUM44TAMR cells to tamoxifen is not, therefore, expected to fully mimic the characteristics observed in MB134TAMR cells. This poses an additional challenge and limits the ability to study and validate the mechanisms underlying the development of anti-estrogen resistance in ILC patients. However, long-term exposure of the two ILC cell lines to tamoxifen, the classic estrogen receptor modulator, to generate TAMR cells and to estrogen deprivation to generate LTED cells, blocking estrogen signaling, led to increased tamoxifen resistance. Importantly, in all these cell lines (TAMR and LTED), methylation-mediated downregulation of ASS1 suggests the role of estrogen signaling in protecting ASS1 promoter methylation. Importantly, ASS1 is not methylated and silenced in SUM44 parental cells, as shown in our studies, suggesting a different mechanism of de novo resistance to anti-estrogen in this patient.
ASS1, the rate-limiting enzyme for the biosynthesis of arginine, catalyzes the conversion of L-citrulline and aspartate to Argininosuccinate [42]. Downregulation of ASS1 results in the availability of aspartate for purine and pyrimidine biosynthesis, facilitating cell proliferation (Fig. 6E). Zhou et al. used Spinosyn A and its derivative LM-21 to augment ASS1 enzymatic activity, which led to the inhibition of cancer cells by blocking pyrimidine biosynthesis [43]. Our study showed enrichment of purine metabolism in the TAMR cells and in the ASS1 knockdown cells, suggesting that ASS1 could be both a biomarker as well as a therapeutic target in tamoxifen-resistant ILC. Use of decitabine, a demethylating agent, augments ASS1 expression and enhances tamoxifen efficacy in our study. Decitabine is clinically approved to treat myelodysplastic syndrome [44], but demonstrated minimal efficacy as monotherapy in solid tumors [45,46,47]. However, combination therapy with targeted agents and chemotherapeutic agents has shown some promise [48], including a recently completed window of opportunity study [49]. Further studies are needed to see if prior treatment with decitabine can overcome tamoxifen resistance in ILC patients.
Association of low ASS1 expression with poor overall survival has been reported in multiple cancers, including bladder [50], myxofibrosarcoma [51], and breast cancer [52], although the number of breast cancer patients included was limited (n = 149) and all subtypes were analyzed. However, analysis of 1980 breast cancer patients from the METABRIC dataset in our study revealed a significant correlation of high ASS1 with poor overall survival. Importantly, subtype-specific analyses focusing on ILC have not been reported before. Correlation of low ASS1 expression with poor OS in ILC patients, only if treated with endocrine therapy as revealed in our study, highlights the potential of ASS1 as a biomarker for endocrine resistance in ILC. We cannot disregard the possibility that such a correlation also exists for endocrine-resistant IDC patients. Further studies are warranted to establish this relationship in IDC, but beyond the scope of this study. Importantly, ASS1 loss has also been implicated in chemotherapeutic resistance in different tumors, including non-small cell lung cancer, ovarian cancer, and hepatocellular carcinoma [51, 53,54,55,56,57,58], suggesting ASS1 to be a vulnerable metabolic hub for the development of therapy resistance.
Our study shows elevated phosphorylation of CAD, a key enzyme in pyrimidine biosynthesis, in both TAMR and shASS1 cells. This further reinforces the notion that metabolic rewiring of existing pathways is a mechanism that cancer cells use to develop treatment resistance. Similar metabolic alteration was reported by Rabinovich et al., showing reduced ASS1 activity in cancer facilitates pyrimidine synthesis by activating CAD [59]. Our transcriptomics data further revealed heightened expression of several key genes involved in nucleotide biosynthesis pathways, suggesting that the acquisition of drug resistance is a multipronged adjustment by the cancer cells for maximum benefit under the adversity of drug treatment. It is therefore likely that we could improve the efficacy of tamoxifen in TAMR cells by targeting nucleotide biosynthesis. As proof of concept, we used Farudodstat to inhibit DHODH and observed a synergistic effect when combined with tamoxifen. This combination therapy could be a potential treatment option for TAM-resistant ILC, warranting further investigation in the clinical setting.
Some limitations of our study warrant acknowledgment. First, our investigation is constrained by the availability of only two ILC cell lines; however, as noted above, these are globally accepted as robust ILC models. Correlation of our findings with patient data partly addresses this limitation. The observed variability in experimental outcomes between these two cell lines may stem from their origin, as discussed previously. In addition, metabolomic and transcriptomic studies provide a snapshot of the metabolic and gene expression state of the cells at the time of harvest. Although seeded at the same density, the inherent difference in rate of cell growth between the lines in this study poses a challenge in capturing the identical metabolic state for all the lines. This is reflected in the dissimilarities in pathway enrichment and metabolic intermediate levels observed in different cell pairs. However, the three pathways and ASS1 alteration, highlighted in this study, are common among the two ILC cell lines and could be a potential predictive marker in ILC patients.
In conclusion, our study highlights ASS1 as a potential biomarker for tamoxifen response and overall survival in ILC patients treated with endocrine therapy. Methylation-mediated downregulation of ASS1 provides an opportunity for clinical intervention of endocrine-resistant ILC patients with demethylating agents, such as Decitabine, and needs to be explored further. Additionally, therapeutic interventions targeting nucleotide biosynthesis pathways show promise in overcoming tamoxifen resistance. Upregulation of purine and pyrimidine biosynthesis pathway enzymes in TAMR cells underscores the importance of metabolic adaptations in resistance. Further research into the role of estrogen in protecting ASS1 promoter methylation and therapeutic implications is expected to enhance treatment strategies of this understudied subtype of breast cancer.
Materials and methods
Cell lines
ILC cell lines MDA-MB134-VI (MB134) (ATCC, USA) and SUM44PE (SUM44) (Asterand, USA) were used to develop the tamoxifen-resistant (TAMR) cells by continuously exposing them to 100–500 nM of 4-hydroxy tamoxifen (4-OHT) for over 6 months. Parental and TAMR MB134 cells were grown in a 1:1 ratio of Dulbecco’s modified Eagle’s medium (DMEM; Gibco, USA) and Leibovitz’s L-15 medium (Gibco, USA), supplemented with 10% fetal bovine serum (FBS) and penicillin-streptomycin. Parental and TAMR SUM44 cell lines were cultured in Ham’s F-12 (Gibco, USA) supplemented with 1 g/L bovine serum albumin, 5 mM ethanolamine, 10 mM HEPES, 1 µg/mL hydrocortisone, 5 µg/mL insulin, 50 nM sodium selenite, 5 µg/ mL apo-transferrin, and 10 nM triodo-L-thyronine. MB134TAMR and SUM44TAMR cells were maintained in media containing 100 nM and 500 nM 4-OHT, respectively. MB134-LTED (Long-Term Estrogen Deprived) and SUM44-LTED cells are generous gifts from Dr. Steffi Oesterreich (University of Pittsburgh), routinely maintained in IMEM + 10% CS-FBS (Charcoal-Stripped FBS) and penicillin-streptomycin [36]. All cell lines were maintained at 37 °C in a humidified 5% CO2 incubator. All cell lines tested were Mycoplasma-free before the experiments.
RNA isolation and sequencing
Total RNA was extracted from exponentially growing cells using Trizol (Invitrogen, USA) following the manufacturer’s protocol. The TAMR cells were grown in tamoxifen-free media for 72 h before harvest. RNA from three biological replicates of each cell line was subjected to RNA-seq (Novogene, USA). Data processing and pathway analysis were performed by Novogene, and the KEGG (Kyoto Encyclopedia of Genes and Genomes) pathway database, GO (Gene Ontology) database, and Reactome Pathway database were used for data analysis.
Polar metabolite extraction
Exponentially growing cells at a density of 1 × 106 in quadruplets were seeded and incubated for 48 h prior to harvesting for metabolite extraction. To ensure robust data normalization and account for variations in cell growth, the raw signal intensity from the spectral data was normalized to the total protein content of each individual cell pellet. Polar metabolites extraction was performed using a cold methanol extraction method as previously described [60, 61]. Briefly, the cells were washed with cold phosphate-buffered saline (PBS), followed by the addition of 250 μL of methanol (LC–MS grade). Internal standards containing 13C and 15N-labeled amino acids mix (1.2 mg/mL) were introduced to the samples in a volume of 50 μL. The cells were homogenized for 2 min and incubated at −20 °C for 20 min. The resulting homogenate was centrifuged to pellet the debris, and 150 μL of the supernatant was transferred to an LC–MS vial for further analysis. Additionally, a pooled quality control (QC) sample was created by combining an equal volume of all supernatants into a separate vial and mixed thoroughly using a vortex.
LC–MS/MS system
Untargeted metabolomics was performed to uncover the metabolic alterations responsible for the drug-resistant phenotype using our established workflow [61]. The LC–MS/MS analyses were performed on a Vanquish ultra high-performance liquid chromatography (UHPLC) system (Thermo Scientific, Waltham, MA, USA) coupled to a Qexactive™ Hybrid Quadrupole-Orbitrap™ Mass Spectrometer (Thermo Scientific, Waltham, MA, USA). A sample volume of 5 μL was injected onto an Xbridge BEH Amide XP Column, 130 Å (150 mm × 2.1 mm ID, particle size 2.5 μm) (Waters Corporation, Milford, MA, USA). The column oven was maintained at 40 °C. Mobile phase A consisted of a mixture of 5 mM NH4Ac in Acetonitrile/H2O (10:90, v/v) containing 0.1% Acetic acid. Mobile phase B consisted of 5 mM NH4Ac in Acetonitrile/H2O (90:10, v/v) containing 0.1% Acetic acid. The mobile phases were delivered at a flow rate of 0.3 mL/min for a 20-min run with the following stepwise gradient for solvent B: firstly 70%; 0–5 min 30%; 5–9 min 30%; 9–11 min 70%. A divert valve was used to direct the flow to waste during the final 5 min of the run. The Qexactive™ was equipped with an electrospray ionization source (ESI) that was operated in both negative and positive ion modes to encompass a broader range of metabolite detection. The ESI source setting and the compound-dependent scan conditions were optimized for full scan MS mode and ranged between 150 and 2000 m/z. The ion spray voltage was set at 4 kV with a capillary temperature of 320 °C. Sheath gas rate was set to 10 arbitrary units. Scans of 1 ms were performed at 35,000 units resolution. A QC sample followed by a blank injection was introduced after every 10 biological sample injections. The pooled samples were leveraged for the top 10 MS/MS analyses, employing dynamic exclusion to identify compounds during the analysis.
Growth kinetics
Exponentially growing cells (30,000/well) were seeded in triplicate in 24-well plates. Subsequently, at 0, 24-, 48-, 72-, and 96-h post-seeding, cells were trypsinized and counted using a cell counter (LUNA-II, Logos Biosystem). Fold change in growth was calculated with the cell number at the 0 h time point as 1.
Generation of ASS1 knockdown cells
For shRNA-mediated knockdown of ASS1, lentivirus coding for ASS1 shRNA in pLKO.1 backbone vector were purchased from Sigma (TRCN0000045554, sequence: GCCTGAATTCTACAACCGGTT and TRCN0000045553, sequence: CCATCCTTTACCATGCTCATT). Exponentially growing MB134 and SUM44 cells (300,000/well) were seeded in 6-well plates. Overnight cultures were infected with 5-10 μL of viral particles in fresh medium containing 10 μg/mL polybrene. The cells were then incubated overnight, followed by replacement of the virus-containing media with fresh complete medium after 16 h of incubation. Cells were expanded, and transduced cells were selected using puromycin. The efficiency of viral infection in SUM44PE and MB134 cells was assessed using the EVOS M7000 GFP-imaging system. Knockdown of ASS1 was validated by qRT-PCR and western blot analysis. Similar experiments were conducted with the empty vector pLKO.1 to generate the control cells.
Quantitative RT-PCR analysis
DNase-treated total RNA was used to synthesize cDNA using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems). qRT-PCR was performed in triplicate using a 96-well StepOne Real-Time PCR System. 36B4 was used as a housekeeping gene. Primer sequences are: ASS1-F: GCTGAAGGAACAAGGCTATGACG and ASS1-R: GCCAGATGAACTCCTCCACAAAC.
36B4-F: GGTTGTAGATGCTGCCATTGTC and 36B4-R: GCCCGAGAAGACCTCCTTTTTC.
Western blot analysis
Whole cell lysates in radioimmunoprecipitation assay (RIPA) buffer (50 mM Tris-HCl pH 7.4, 150 mM NaCl, 1% NP-40, 0.1% SDS; Sigma–Aldrich), supplemented with protease and phosphatase inhibitors (Sigma), were resolved on SDS polyacrylamide gels. Following electrophoresis, proteins were transferred onto 0.45 µM PVDF membranes. Nonspecific binding was blocked by incubation with blocking buffer (Rockland) for 60 min at room temperature. The membranes were probed for ASS1 [Cell Signaling Technology (CST), 70720], GAPDH (CST, 2118), β-actin [CST, 3700], ERα (Abcam, ab32063), HER2 (CST, 2242), and Phosphor-CAD (Ser1859) (CST,12662). ASS1 and GAPDH were detected using IR800CW dye-tagged IgG secondary antibody (LI COR, 926-32211). Phosphorylated proteins (pCAD) were detected using peroxidase-conjugated anti-rabbit secondary antibody (CST, 7074) and enhanced chemiluminescence western blot detection reagents (Pierce, Thermo Scientific). The Odyssey CLx and Fc systems (LI-COR Biosciences, USA) were used for western blot imaging. All original western blot images are provided in Supplementary File2.
Methylation-specific PCR
Computational analysis using ‘CpG Island Finder’ (CpG Islands (https://bioinformatics.org)) was performed to locate CpG islands on gene promoters. DNA (200–500 ng) extracted from exponentially growing cells was subjected to bisulfite conversion using the EZ DNA methylation kit (Zymo Research Corporation, USA). Treatment of genomic DNA with sodium bisulfite converts unmethylated cytosine residues to uracil, while methylated cytosine residues remain unchanged. The methylation status of the ASS1 promoter was determined using methylation-specific PCR (MSPCR). The bisulfite-converted DNA (1–4 µL) was used for PCR reactions with primers specific for either methylated (F: GTCGGTATCGGATAGAAGTGAGTAC, R: ATAACTCAAAAACGAAAAATAACCG) or unmethylated sequences (F: TTGGTATTGGATAGAAGTGAGTATGA, R: AACTCAAAAACAAAAAATAACCACA)[56]. PCR conditions were as follows: 8 cycles of 95 °C for 2 min, 61 °C for 30 s, and 72 °C for 30 s, followed by 32 cycles of 95 °C for 30 s, 61 °C for 30 s, and 72 °C for 30 s, with a final extension at 72 °C for 5 min. PCR products were electrophoresed in 2% agarose gels and visualized using a transilluminator.
Cell viability assay
To assess cell viability and drug effect, we have used (i) the MTT assay kit (Roche) and (ii) the automated cell counting method. The drugs included 5 µM of 5-aza-2′ deoxycytidine (dAzaC, Sigma), also known as Decitabine, 4-hydroxy tamoxifen (0–25 µM, Cayman Chemical), and a pyrimidine biosynthesis inhibitor, Farudodstat (7.5–20 µM, Cayman Chemical). For MTT assay, 15,000 cells were seeded per well in triplicate in a 96-well plate, and overnight cultures were treated with drugs for 120 h. This was followed by the addition of MTT reagent and solubilizing agent following the manufacturer’s protocol. Absorbance of the solubilized formazan was read at 595 nm using a spectrophotometer. For cell counting assays, cells were seeded at a density of 50,000 cells per well in a 24-well plate. The following day, cells were treated with the drugs as indicated and incubated for 120 h. Cells in triplicate wells were trypsinized, suspended in 1× PBS, stained with 0.4% trypan blue solution at a 1:1 ratio, and counted using a cell counter. All experiments were performed in biological triplicates, and statistical significance was determined using a t-test. CompuSyn 1.0 (https://compusyn.software. informer.com/) was used to analyze the combinatorial effect of two drugs. Combination index (CI) value = 1, <1, and >1 indicate additive, synergistic, and antagonistic effects, respectively.
Cell migration assay
In vitro cell migration assays were conducted using 24-well Transwell chambers (Corning, USA) coated with collagen (50 μg/mL) on the exterior of the inserts for 60 min at 37 °C. For the migration assay, 500,000 cells in serum-free media were seeded onto the inserts. A chemotactic gradient was established by adding 0.6 mL of complete growth medium containing 10% FBS in the lower chamber. Cells were allowed to migrate for 72 h or for 120 h. At the end of the specified time of migration, the unmigrated cells in the inserts were removed using a cotton swab, and the migrated cells were fixed in methanol and stained with 0.5% crystal violet solution. The area occupied by migrated cells was quantified using ImageJ software.
Patient dataset analysis
Human breast cancer patient data was obtained from The Cancer Genome Atlas Firehose BRCA cohort (TCGA_BRCA), and the METABRIC invasive breast carcinoma cohort was obtained from the cBioPortal webpage. Analysis of METABRIC patient data was conducted in R 4.2.2 utilizing dplyr 1.0.10, tibble 3.1.8, ggplot2 3.4.0, and survival 3.5.8 packages to import, subset, and analyze relevant patient data [62]. The Kmplotter webtool was used to analyze the Kmplotter meta-cohort (Kmplotter.com) [63].
Statistical analysis
Three independent replicates of all the experiments were conducted. Western blot experiments were independently repeated using cell lysates from three biological replicates, and data expressed as the mean ± standard deviation (SD). Statistical analyses between the two groups were performed using Student’s t-test. One-way ANOVA was used for multiple group comparisons. The percentage of cell viability and IC50 value were calculated using GraphPad Prism. Differences in survival of patients from the METABRIC cohort and the KM plotter meta-cohort were determined via the log-rank test. A p-value < 0.05 was considered statistically significant.
Metabolomic data processing and statistical analysis
Initial screening of the spectral peaks was performed using the Quan browser module of Xcalibur version 4.0 (Thermo Fisher Scientific, Waltham, MA, USA). The MS data were searched against our in-house database containing experimentally obtained MS/MS spectra of 171 authentic analytical standards using Compound Discoverer software (Thermo Scientific, San Jose, CA, USA). The raw data was normalized to the protein content per replicate. Subsequently, the spectra underwent filtration to diminish redundancy and ensure instrument reproducibility. Any metabolite exhibiting a coefficient of variation exceeding 20% was eliminated before subsequent analysis. Statistical analyses, including univariate T-test, were conducted using the online resource MetaboAnalyst 5.0. Partial Least Squares Discriminant Analysis (PLS-DA) was employed to interpret the metabolic variances between the sensitive and resistant cell lines. VIP (Variables Important in Projection) plots were generated to visualize the key metabolites contributing to the deregulated metabolic processes. Overall metabolite data was subjected to quantitative enrichment analysis to pinpoint the deregulated metabolic processes within the cell pairs. A Venn diagram was generated to show the distinguishable gene expression profiles among samples and summarize the mutually deregulated pathways across both metabolomics and transcriptomics datasets. The gene-metabolite interaction networks were constructed by integrating annotated metabolites or genes with comprehensive interaction data from the Search Tool for Interactions of Chemicals (STITCH) [64]. This tool utilizes interaction data from peer-reviewed literature to assess node importance within the network based on degree centrality and betweenness centrality. Degree centrality is determined by the number of connections a node has with others, while betweenness centrality calculates the number of direct routes passing through the node. These measures help identify metabolic hubs within the network.
Data availability
The RNAseq data generated during the current study is available at https://www.ncbi.nlm.nih.gov/geo/ and the accession number is GSE 301605. The metabolomics data generated during the current study is available at MassIVE database (https://massive.ucsd.edu/) and ID is MassIVE MSV000096128.
References
Thomas M, Kelly ED, Abraham J, Kruse M. Invasive lobular breast cancer: a review of pathogenesis, diagnosis, management, and future directions of early stage disease. Semin Oncol. 2019;46:121–32.
McCart Reed AE, Kalinowski L, Simpson PT, Lakhani SR. Invasive lobular carcinoma of the breast: the increasing importance of this special subtype. Breast Cancer Res. 2021;23:6.
Arpino G, Bardou VJ, Clark GM, Elledge RM. Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res. 2004;6:R149–56.
Li CI, Uribe DJ, Daling JR. Clinical characteristics of different histologic types of breast cancer. Br J Cancer. 2005;93:1046–52.
McCart Reed AE, Kutasovic JR, Lakhani SR, Simpson PT. Invasive lobular carcinoma of the breast: morphology, biomarkers and ‘omics. Breast Cancer Res. 2015;17:12.
[Available from: https://seer.cancer.gov/data/.
Li CI, Anderson BO, Daling JR, Moe RE. Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA. 2003;289:1421–4.
Pestalozzi BC, Zahrieh D, Mallon E, Gusterson BA, Price KN, Gelber RD, et al. Distinct clinical and prognostic features of infiltrating lobular carcinoma of the breast: combined results of 15 International Breast Cancer Study Group clinical trials. J Clin Oncol. 2008;26:3006–14.
Oceguera-Basurto P, Topete A, Oceguera-Villanueva A, Rivas-Carrillo J, Paz-Davalos M, Quintero-Ramos A, et al. Selective estrogen receptor modulators in the prevention of breast cancer in premenopausal women: a review. Transl Cancer Res. 2020;9:4444–56.
Damodaran S, O’Sullivan CC, Elkhanany A, Anderson IC, Barve M, Blau S, et al. Open-label, phase II, multicenter study of lasofoxifene plus abemaciclib for treating women with metastatic ER+/HER2- breast cancer and an ESR1 mutation after disease progression on prior therapies: ELAINE 2. Ann Oncol. 2023;34:1131–40.
Goetz MP, Bagegni NA, Batist G, Brufsky A, Cristofanilli MA, Damodaran S, et al. Lasofoxifene versus fulvestrant for ER+/HER2- metastatic breast cancer with an ESR1 mutation: results from the randomized, phase II ELAINE 1 trial. Ann Oncol. 2023;34:1141–51.
Tsuji J, Li T, Grinshpun A, Coorens T, Russo D, Anderson L, et al. Clinical efficacy and whole-exome sequencing of liquid biopsies in a phase IB/II study of bazedoxifene and palbociclib in advanced hormone receptor-positive breast cancer. Clin Cancer Res. 2022;28:5066–78.
Pramod N, Nigam A, Basree M, Mawalkar R, Mehra S, Shinde N, et al. Comprehensive review of molecular mechanisms and clinical features of invasive lobular cancer. Oncologist. 2021;26:e943–e53.
Regan MM, Price KN, Giobbie-Hurder A, Thurlimann B, Gelber RD, International Breast Cancer Study G, Group BIGC. Interpreting Breast International Group (BIG) 1-98: a randomized, double-blind, phase III trial comparing letrozole and tamoxifen as adjuvant endocrine therapy for postmenopausal women with hormone receptor-positive, early breast cancer. Breast Cancer Res. 2011;13:209.
Musgrove EA, Sutherland RL. Biological determinants of endocrine resistance in breast cancer. Nat Rev Cancer. 2009;9:631–43.
Miller TE, Ghoshal K, Ramaswamy B, Roy S, Datta J, Shapiro CL, et al. MicroRNA-221/222 confers tamoxifen resistance in breast cancer by targeting p27Kip1. J Biol Chem. 2008;283:29897–903.
Mishra A, Srivastava A, Pateriya A, Tomar MS, Mishra AK, Shrivastava A. Metabolic reprograming confers tamoxifen resistance in breast cancer. Chem Biol Interact. 2021;347:109602.
Yoo HC, Han JM. Amino acid metabolism in cancer drug resistance. Cells. 2022;11. 140–67.
Fendt SM, Frezza C, Erez A. Targeting metabolic plasticity and flexibility dynamics for cancer therapy. Cancer Discov. 2020;10:1797–807.
Tan Y, Li J, Zhao G, Huang KC, Cardenas H, Wang Y, et al. Metabolic reprogramming from glycolysis to fatty acid uptake and beta-oxidation in platinum-resistant cancer cells. Nat Commun. 2022;13:4554.
Robey RB, Weisz J, Kuemmerle NB, Salzberg AC, Berg A, Brown DG, et al. Metabolic reprogramming and dysregulated metabolism: cause, consequence and/or enabler of environmental carcinogenesis?. Carcinogenesis. 2015;36 Suppl 1:S203–31.
Santos JR, Waitzberg DL, da Silva IDCG, Junior TCT, Barros LRC, Canuto GAB, et al. Distinct pattern of one-carbon metabolism, a nutrient-sensitive pathway, in invasive breast cancer: a metabolomic study. Oncotarget. 2020;11:1637–52.
Worley B, Powers R. Multivariate analysis in metabolomics. Curr Metab. 2013;1:92–107.
Ding K, Chen L, Levine K, Sikora M, Tasdemir N, Dabbs D, et al. Estrogen regulation and functional role of FGFR4 in estrogen receptor positive breast cancer. bioRxiv [Preprint]. 2024. Available from: https://doi.org/10.1101/2024.03.18.585626.
Hatzis C, Pusztai L, Valero V, Booser DJ, Esserman L, Lluch A, et al. A genomic predictor of response and survival following taxane-anthracycline chemotherapy for invasive breast cancer. JAMA. 2011;305:1873–81.
Ding Q, Li R, Wang Q, Yu L, Zi F. A pan-cancer analysis of the role of argininosuccinate synthase 1 in human tumors. Front Oncol. 2023;13:1049147.
Wei Z, Liu X, Cheng C, Yu W, Yi P. Metabolism of amino acids in cancer. Front Cell Dev Biol. 2020;8:603837.
Mouabbi JA, Hassan A, Lim B, Hortobagyi GN, Tripathy D, Layman RM. Invasive lobular carcinoma: an understudied emergent subtype of breast cancer. Breast Cancer Res Treat. 2022;193:253–64.
Chang M. Tamoxifen resistance in breast cancer. Biomol Ther. 2012;20:256–67.
Osborne CK, Schiff R. Mechanisms of endocrine resistance in breast cancer. Annu Rev Med. 2011;62:233–47.
Zhou Y, Yau C, Gray JW, Chew K, Dairkee SH, Moore DH, et al. Enhanced NF kappa B and AP-1 transcriptional activity associated with antiestrogen resistant breast cancer. BMC Cancer. 2007;7:59.
Schiff R, Reddy P, Ahotupa M, Coronado-Heinsohn E, Grim M, Hilsenbeck SG, et al. Oxidative stress and AP-1 activity in tamoxifen-resistant breast tumors in vivo. J Natl Cancer Inst. 2000;92:1926–34.
Ciriello G, Gatza ML, Beck AH, Wilkerson MD, Rhie SK, Pastore A, et al. Comprehensive molecular portraits of invasive lobular breast cancer. Cell. 2015;163:506–19.
Stires H, Heckler MM, Fu X, Li Z, Grasso CS, Quist MJ, et al. Integrated molecular analysis of tamoxifen-resistant invasive lobular breast cancer cells identifies MAPK and GRM/mGluR signaling as therapeutic vulnerabilities. Mol Cell Endocrinol. 2018;471:105–17.
Du T, Sikora MJ, Levine KM, Tasdemir N, Riggins RB, Wendell SG, et al. Key regulators of lipid metabolism drive endocrine resistance in invasive lobular breast cancer. Breast Cancer Res. 2018;20:106.
Sikora MJ, Jacobsen BM, Levine K, Chen J, Davidson NE, Lee AV, et al. WNT4 mediates estrogen receptor signaling and endocrine resistance in invasive lobular carcinoma cell lines. Breast Cancer Res. 2016;18:92.
Fu X, Jeselsohn R, Pereira R, Hollingsworth EF, Creighton CJ, Li F, et al. FOXA1 overexpression mediates endocrine resistance by altering the ER transcriptome and IL-8 expression in ER-positive breast cancer. Proc Natl Acad Sci USA. 2016;113:E6600–E9.
Sflomos G, Schipper K, Koorman T, Fitzpatrick A, Oesterreich S, Lee AV, et al. Atlas of lobular breast cancer models: challenges and strategic directions. Cancers. 2021;13.5396–430.
Shah OS, Chen F, Wedn A, Kashiparekh A, Knapick B, Chen J, et al. Multi-omic characterization of ILC and ILC-like cell lines as part of ILC cell line encyclopedia (ICLE) defines new models to study potential biomarkers and explore therapeutic opportunities. bioRxiv [Preprint]. 2023. Available from: https://doi.org/10.1101/2023.09.26.559548.
Cheng GJ, Leung EY, Singleton DC. Breast cancer models for studying mechanisms of resistance to endocrine therapy. Explor Target Antitumor Ther. 2022;3:297–320.
Ethier SP, Mahacek ML, Gullick WJ, Frank TS, Weber BL. Differential isolation of normal luminal mammary epithelial cells and breast cancer cells from primary and metastatic sites using selective media. Cancer Res. 1993;53:627–35.
Yang JS, Wang CC, Qiu JD, Ren B, You L. Arginine metabolism: a potential target in pancreatic cancer therapy. Chin Med J. 2020;134:28–37.
Zou Z, Hu X, Luo T, Ming Z, Chen X, Xia L, et al. Naturally-occurring spinosyn A and its derivatives function as argininosuccinate synthase activator and tumor inhibitor. Nat Commun. 2021;12:2263.
Greenberg PL, Stone RM, Al-Kali A, Bennett JM, Borate U, Brunner AM, et al. NCCN Guidelines(R) Insights: Myelodysplastic Syndromes, Version 3.2022. J Natl Compr Canc Netw. 2022;20:106–17.
Harrer DC, Schenkel C, Berking C, Herr W, Abken H, Dorrie J, et al. Decitabine-mediated upregulation of CSPG4 in ovarian carcinoma cells enables targeting by CSPG4-specific CAR-T cells. Cancers. 2022;14:5033–46.
Taib N, Merhi M, Inchakalody V, Mestiri S, Hydrose S, Makni-Maalej K, et al. Treatment with decitabine induces the expression of stemness markers, PD-L1 and NY-ESO-1 in colorectal cancer: potential for combined chemoimmunotherapy. J Transl Med. 2023;21:235.
Xu M, Song B, Yang X, Li N. The combination of decitabine and aspirin inhibits tumor growth and metastasis in non-small cell lung cancer. J Int Med Res. 2022;50:3000605221112024.
Hu C, Liu X, Zeng Y, Liu J, Wu F. DNA methyltransferase inhibitors combination therapy for the treatment of solid tumor: mechanism and clinical application. Clin Epigenetics. 2021;13:166.
Bear H, Deng X, Bandyopadhyay D, Idowu M, Kmieciak M, Williams M, et al. Abstract PO1-18-04: Neoadjuvant pembrolizumab + decitabine followed by standard neoadjuvant chemotherapy for locally advanced HER2- breast cancer (NCT02957968). Cancer Res. 2024;84 Suppl 9:PO1-18-04.
Allen MD, Luong P, Hudson C, Leyton J, Delage B, Ghazaly E, et al. Prognostic and therapeutic impact of argininosuccinate synthetase 1 control in bladder cancer as monitored longitudinally by PET imaging. Cancer Res. 2014;74:896–907.
Huang HY, Wu WR, Wang YH, Wang JW, Fang FM, Tsai JW, et al. ASS1 as a novel tumor suppressor gene in myxofibrosarcomas: aberrant loss via epigenetic DNA methylation confers aggressive phenotypes, negative prognostic impact, and therapeutic relevance. Clin Cancer Res. 2013;19:2861–72.
Qiu F, Chen YR, Liu X, Chu CY, Shen LJ, Xu J, et al. Arginine starvation impairs mitochondrial respiratory function in ASS1-deficient breast cancer cells. Sci Signal. 2014;7:ra31.
Long Y, Tsai WB, Chang JT, Estecio M, Wangpaichitr M, Savaraj N, et al. Cisplatin-induced synthetic lethality to arginine-starvation therapy by transcriptional suppression of ASS1 is regulated by DEC1, HIF-1α, and c-Myc transcription network and is independent of ASS1 promoter DNA methylation. Oncotarget. 2016;7:82658–70.
Sun N, Zhao X. Argininosuccinate synthase 1, arginine deprivation therapy and cancer management. Front Pharm. 2022;13:935553.
Nicholson LJ, Smith PR, Hiller L, Szlosarek PW, Kimberley C, Sehouli J, et al. Epigenetic silencing of argininosuccinate synthetase confers resistance to platinum-induced cell death but collateral sensitivity to arginine auxotrophy in ovarian cancer. Int J Cancer. 2009;125:1454–63.
Syed N, Langer J, Janczar K, Singh P, Lo Nigro C, Lattanzio L, et al. Epigenetic status of argininosuccinate synthetase and argininosuccinate lyase modulates autophagy and cell death in glioblastoma. Cell Death Dis. 2013;4:e458.
Delage B, Luong P, Maharaj L, O’Riain C, Syed N, Crook T, et al. Promoter methylation of argininosuccinate synthetase-1 sensitises lymphomas to arginine deiminase treatment, autophagy and caspase-dependent apoptosis. Cell Death Dis. 2012;3:e342.
Wei SH, Chen CM, Strathdee G, Harnsomburana J, Shyu CR, Rahmatpanah F, et al. Methylation microarray analysis of late-stage ovarian carcinomas distinguishes progression-free survival in patients and identifies candidate epigenetic markers. Clin Cancer Res. 2002;8:2246–52.
Rabinovich S, Adler L, Yizhak K, Sarver A, Silberman A, Agron S, et al. Diversion of aspartate in ASS1-deficient tumours fosters de novo pyrimidine synthesis. Nature. 2015;527:379–83.
Choueiry F, Zhu J. Secondary electrospray ionization-high resolution mass spectrometry (SESI-HRMS) fingerprinting enabled treatment monitoring of pulmonary carcinoma cells in real time. Anal Chim Acta. 2022;1189:339230.
Choueiry F, Singh S, Sircar A, Laliotis G, Sun X, Chavdoula E, et al. Integration of metabolomics and gene expression profiling elucidates IL4I1 as modulator of ibrutinib resistance in ABC-diffuse large B cell lymphoma. Cancers. 2021;13:2146–67.
Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature. 2012;486:346–52.
Győrffy B. Survival analysis across the entire transcriptome identifies biomarkers with the highest prognostic power in breast cancer. Comput Struct Biotechnol J. 2021;19:4101–9.
Kuhn M, von Mering C, Campillos M, Jensen LJ, Bork P. STITCH: interaction networks of chemicals and proteins. Nucleic Acids Res. 2008;36:D684–8. (Database issue).
Acknowledgements
We are grateful for the philanthropic support of Helen and Brad Anderson of Columbus, Ohio, towards this research, and grateful to Steffi Oesterreich, Ph.D., of the University of Pittsburgh for providing the ILC-LTED cell lines.
Funding
Research reported in this publication was partially supported by Pelotonia Undergraduate Research Fellowship (to NP and AK), Pelotonia Graduate Fellowship (to FC), and by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number R35GM133510 (to JZ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
AG and FC: Experimental design, methodology, investigation, and writing the original draft. JR: Bioinformatic analysis of patient data, Writing, and Review. NP, AK, ES: Investigation. STS: Supervision of bioinformatics analysis and Review. DGS: Supervision and Editing. JZ: Resources, Data curation, Editing. BR: Funding acquisition, supervision, editing, and project administration. SM: conceptualization, supervision, data interpretation, writing, review, and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics
This study was conducted using a publicly available database and human invasive lobular carcinoma (ILC) cell lines. Since this research did not use either patients, patient-derived materials, or animals, ethics approval was not required. All cell lines used were obtained from accredited sources (ATCC) and handled according to standard laboratory safety and ethical guidelines.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by Dr Satoshi Inoue
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gupta, A., Choueiry, F., Reardon, J. et al. Invasive lobular carcinoma: integrated multi-omics analysis reveals silencing of Argininosuccinate synthase and upregulation of nucleotide biosynthesis in tamoxifen resistance. Cell Death Dis 16, 514 (2025). https://doi.org/10.1038/s41419-025-07788-6
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41419-025-07788-6