Abstract
The increasing prevalence of night shift work (NSW) in our current professional landscape has raised significant public health concerns, particularly regarding its potential role in breast cancer (BC) development among women. Recognized by the International Agency for Research on Cancer (IARC) as a probable human carcinogen, NSW is believed to contribute to carcinogenesis primarily through circadian disruption induced by exposure to light at night. This review explores three key areas: (1) the biological mechanisms potentially linking NSW to BC, including melatonin suppression, oxidative stress, immune dysregulation, chronic inflammation, clock gene alterations, epigenetic modifications, telomere shortening, estrogen signaling disruption, vitamin D deficiency, and gut microbiome imbalance; (2) the emergence of novel putative biomarkers with might be relevant to early detection and precision risk analysis; and (3) the latest epidemiological evidence from case-control and cohort studies evaluating BC risk in female night shift workers, while considering the heterogeneity caused by exposure misclassification and other confounding factors. Altogether, these insights underscore the importance of integrating mechanistic, molecular, and epidemiological data, not only to deepen our understanding of the strength and nature of the relationship between NSW and BC, but also to support a precision medicine framework. This integrated approach is essential for improving individual risk stratification, guiding occupational health policies, and developing targeted preventive strategies for high-risk workers.
Similar content being viewed by others
Introduction
In industrialized societies, the demand for around-the-clock productivity has led to the widespread adoption of novel workplace dynamics, such as night shift work (NSW), across essential sectors including healthcare, transportation, manufacturing, and security1. This shift in labor patterns, although vital to the functioning of our 24 h global economy, has introduced substantial public health concerns, especially for women2. Indeed, a growing body of evidence suggests a potential association between long-term NSW and an increased risk of developing breast cancer (BC), a hypothesis with far-reaching implications for occupational medicine and cancer prevention3. BC remains the most commonly diagnosed malignancy and the leading cause of cancer-related mortality among women worldwide4. The contribution of occupational factors to this burden could translate into a significant number of preventable cases, making the elucidation of this association a priority for the occupational medicine sector5.
Since 2019, the International Agency for Research on Cancer (IARC) has classified NSW as “probably carcinogenic to humans” (i.e., Group 2 A carcinogen), based on strong mechanistic evidence and suggestive epidemiological data6. This decision reflects increasing recognition of circadian disruption as a biologically plausible contributor to cancer development7. Hence, several epidemiological studies demonstrated an elevated incidence of BC among women exposed to long-term or rotating night shifts (NS). However, these findings have often been inconsistent and limited by challenges in exposure classification, retrospective design, and/or inadequate control of confounding factors1. Pivotally, BC is a prototypical multifactorial disease influenced by a complex interplay of genetic, hormonal, reproductive, environmental, and lifestyle factors8. Hence, isolating the specific contribution of NSW within this context is inherently difficult9. Many factors, such as age, menopausal status, hormonal therapy, lactation, family history, and high-penetrance germline mutations (e.g., BRCA1/2), all shape individual risk10. Moreover, gene-environment interactions, often mediated by epigenetic modifications, may further modulate susceptibility to carcinogenic effects of NSW, complicating causal inference11.
At the mechanistic level, the hypothesized link between NSW and BC is grounded in the concept of circadian disruption12. Circadian rhythms are endogenously generated 24 h cycles in physiology and behavior that are orchestrated by the suprachiasmatic nucleus (SCN) of the hypothalamus, commonly referred to as the central clock13. These rhythms regulate a wide range of biological processes including hormonal secretion, immune function, DNA repair, metabolism, and cell cycle progression14. Synchronization of the central clock with the external environment relies on time cues known as zeitgebers (derived from the German “time-givers”)15. The most dominant zeitgeber is the light-dark cycle, although other factors such as feeding times, temperature changes, and social cues also contribute16. NSW disturbs this alignment by exposing individuals to artificial light at night (LAN), in turn altering both sleep-wake and feeding rhythms. This misalignment, often termed circadian desynchrony, may have far-reaching effects on hormonal and metabolic homeostasis17.
One of the most critical pathways implicated in the NSW-BC axis involves the suppression of nocturnal melatonin secretion18. Melatonin, a neuro-hormone produced by the pineal gland in darkness, possesses potent oncostatic properties19. It regulates cell proliferation, promotes apoptosis in malignant cells, scavenges reactive oxygen species, and, importantly, it modulates estrogen receptor (ER) expression and activity20. Its suppression through LAN exposure is hypothesized to facilitate estrogen-dependent carcinogenesis21. Preclinical studies in rodent models have shown that LAN exposure, increases oxidative DNA damage, disrupts estrogen signaling and accelerates mammary tumor growth22. These effects that can be partially reversed by exogenous melatonin administration23. Altogether, these findings support the so-called melatonin-estrogen hypothesis of breast carcinogenesis24.
In addition to melatonin-related mechanisms, there is growing interest in uncovering the role played by circadian clock genes (such as CLOCK, BMAL1, PER1/2/3, CRY1/2, and NPAS2), which not only govern circadian timing but also regulate processes central to tumorigenesis, including cell cycle control, DNA damage response, metabolism, and immune regulation25. Alterations either in the expression or in the epigenetic regulation of these genes have been observed in BC and are increasingly linked to exposure to chronic NSW26. For instance, reduced expression of PER1 and CRY1 has been associated with higher tumor grade and poor prognosis27.
Epidemiological efforts are likewise evolving. While earlier studies were limited by crude exposure assessments and lack of chronobiological context (e.g., individual chronotype, sleep quality), newer cohorts are integrating objective measurements such as actigraphy, light sensors, and sleep diaries28. Concurrently, genetic and epigenetic profiling is being incorporated into large-scale prospective studies to further clarify gene-environment interactions, identify biologically vulnerable subgroups, and build individualized risk models29. Some of these investigations are also testing interventional strategies, such as melatonin supplementation or circadian-friendly lighting systems, to mitigate biological disruptions in NS workers30.
Recent studies have begun to identify novel molecular biomarkers capable of capturing early biological effects of NSW exposure31. Among the most promising markers there are: urinary melatonin metabolites (such as 6-sulfatoxymelatonin or aMT6s), salivary or serum cortisol profiles, DNA methylation signatures in clock and tumor suppressor genes, telomere elongation patterns, and altered circulating microRNAs (miRNAs) levels32,33. These novel biomarkers may eventually provide precision tools for risk stratification, early detection, and intervention among NSW-exposed individuals, but further validation in longitudinal cohort studies is essential34.
Despite considerable progress, multiple challenges remain. For instance, the absence of standardized definitions for NSW across studies, the difficulty in quantifying long-term exposure retrospectively, and the often-subtle nature of biological changes, all hinder the establishment of causality and the development of occupational exposure limits35. Nevertheless, the convergence of mechanistic, epidemiological, and biomarker-based evidence suggests that the link between NSW and BC is biologically plausible and clinically relevant1. In this context, moving from risk description to precision risk prediction represents both a scientific and ethical imperative11.
This review aims to report the most recent and significant advances in our understanding of the relationship between NSW and BC, with a particular focus on female occupational exposure. By integrating mechanistic evidence, biomarker discoveries, and emerging data from human studies, it will be examined how chronic circadian disruption may drive breast carcinogenesis, how novel molecular tools could refine individual risk stratification, and, finally, how these insights might reshape regulatory frameworks and preventive strategies17. Although NSW is currently as a Group 2 A carcinogen, this assessment is primarily based on mechanistic evidence and limited epidemiological data1. By critically reviewing recent scientific developments, the final goal is to assess whether new findings might reinforce this classification or offer alternative perspectives that may refine or challenge it. In fact, as we are living the era of precision medicine, there is a pressing need to identify high-risk workers, establish robust exposure-effect relationships, and develop targeted interventions to mitigate occupational cancer risk36.
Literature search and outcomes
A keyword search was carried out in PubMed, Web of Science, and Scopus databases. Keywords were organized into major thematic groups to ensure systematic coverage of all relevant aspects. Boolean operators (“AND,” “OR”) were used to combine terms across groups (Supplementary Table 1). In addition, a MEDLINE search using Medical Subject Headings (MeSH) was conducted. Each MeSH term was combined with relevant subheadings and qualifiers to refine the search (Supplementary Table 2).
The search was limited to peer-reviewed articles in English. Inclusion criteria were: (1) original research or review articles examining the association between NSW and BC in women; (2) studies addressing biological mechanisms, epidemiological associations, or biomarker discovery; (3) observational studies (cohort, case-control, cross-sectional) or experimental/preclinical evidence relevant to NSW-BC pathways. Exclusion criteria included: (1) preprints, editorials, commentaries, or conference abstracts without peer review; (2) articles without full-text availability; (3) studies not directly relevant to the predefined thematic topics.
As shown in the flow diagram (Supplementary Fig. 1), the initial database search identified 2494 records. After removing 1799 duplicates, 695 records remained for screening. Of these, 384 articles were excluded due to non-English language, unavailable full text, preprints, or lack of relevance. Ultimately, 312 records were included in the final review. Among these, 151 were used for general review across all sections, while 161 peer-reviewed studies met the inclusion criteria and were retained for qualitative analysis. Within this subset, 127 studies were discussed in the section on mechanistic studies in worker cohorts, while 34 studies were analyzed in the section focusing on worker populations assessing BC risk.
Night shift work-related breast carcinogenesis: mechanistic pathways and biomarker discovery
The etiopathogenesis of BC in the context of NSW is increasingly understood through mechanistic studies that explore the biological consequences of circadian disruption37. Experimental models have been instrumental in elucidating how perturbations in circadian rhythms may foster a pro-tumorigenic environment, particularly through hormonal, immune, genetic, and epigenetic pathways38. Furthermore, human evidence strengthened the current conclusions39.
A substantial body of research conducted in animals has consistently demonstrated that the disruption of the normal light-dark cycle may significantly increase cancer incidence, tumor growth, and progression40,41. In particular, it was observed that either phase shifts in the light-dark schedule or manipulated photoperiods may promote the initiation and advancement of mammary tumors42,43,44.
In detail, over six decades of research have progressively deepened our understanding of the role of LAN and circadian disruption in BC development. Foundational rodent studies in the 1960s, were among the first to correlate either constant light exposure or surgical pinealectomy (which disrupts melatonin production) in heightening mammary tumor risk, highlighting the central role of the pineal gland in circadian-driven hormonal regulation45,46. Subsequently, research from the 1980s and 1990s consistently found that suppression of melatonin via continuous light exposure increased susceptibility to chemically induced mammary tumors, while exogenous melatonin conferred protective effects47,48,49,50,51. The 2000s marked a mechanistic leap, as it was demonstrated that suppression of nocturnal melatonin through LAN enhanced BC cellular metabolism and growth in breast cancer xenografts, providing compelling evidence of a link between circadian biology and tumor progression52,53,54. Additional studies confirmed that constant light exposure accelerated tumorigenesis in chemically induced mammary cancer models44,55.
More recent work has expanded these insights. For instance, It was demonstrated that circadian disruption induced by jet lag or shifted light cycles not only accelerates tumor development but also disrupts endocrine, metabolic, and immune pathways that are central to breast carcinogenesis 40,56. Furthermore, emerging evidence reveals that circadian misalignment promotes metastasis by enhancing tumor stemness and modifying the tumor immune microenvironment, while also impairing the efficacy of cancer therapies such as cisplatin57,58. Also, it was shown that dietary quercetin mitigates the metastasis-promoting effects of disrupted light-dark cycles, suggesting that holistic dietary or chrono-modulated interventions may offer therapeutic benefit in circadian-compromised oncologic contexts59.
Taken together, the results underscore circadian rhythm disruption as a significant and modifiable environmental risk factor in BC development and progression. Importantly, the majority of these experimental findings have been further corroborated in human NS workers, with clear differences compared to day workers observed across multiple biological mechanisms (including oxidative stress, immune dysfunction, inflammation, melatonin disruption, clock gene alterations, epigenetic changes, telomere attrition, and hormonal imbalances). These key aspects are summarized in Fig. 1 and thoroughly discussed in the sections below.
The diagram illustrates the transition from a healthy breast to breast cancer, driven by chronic exposure to night shift work. Key biological mechanisms implicated in this process are reported. Selected elements adapted from Servier Medical Art (https://smart.servier.com, last accessed on 09 November 2025), licensed under Creative Commons Attribution 4.0 International License (CC BY 4.0; https://creativecommons.org/licenses/by/4.0/, last accessed on 09 November 2025).
Oxidative stress
Multiple preclinical findings have demonstrated that LAN exposure induces oxidative stress responses, leading to the accumulation of reactive oxygen species (ROS), DNA damage, and altered expression of oxidative stress-related genes60,61,62. In turn, these oxidative insults contribute to genomic instability and may act as an early driver of BC development63.
In line with the preclinical evidence, a number of clinical observations in NS and rotating shift workers across various populations and settings consistently suggest that NSW is associated with elevated oxidative stress and DNA damage, along with alterations in antioxidant defense systems64. For a summary of the worker findings, see Table 1. In particular, urinary 8-hydroxy-2’-deoxyguanosine (8-OHdG), a marker of oxidative DNA damage, has been found higher in NS workers compared to day shift (DS) workers, although its levels may vary depending on timing relative to work and sleep periods65,66,67,68. Consistently, a recent long-term cohort study in hospital NS workers using a ‘1-1-3’ rotating schedule reported significantly increased serum and urinary levels of 8-OHdG during the NS period, which remained elevated even one month after returning to DS, indicating persistent oxidative DNA damage induced by chronic NSW69. Also, the expression of the DNA repair enzyme OGG1 is often reduced in NS workers, with increased DNA strand breaks and lowered repair-genes expression measured in blood mononuclear cells from NS physicians compared to DS ones70,71.
Other blood markers such as superoxide dismutase (SOD), catalase (CAT), and malondialdehyde (MDA) are frequently found elevated in NS workers, indicating enhanced oxidative stress72,73. Similarly, total oxidative status (TOS), oxidative stress index (OSI), and urinary 8-isoprostane levels (a non-enzymatic peroxidation product of arachidonic acid) tend to increase after extended or continuous NSW, with concurrent decreases or alterations in total antioxidant capacity (TAC) and total antioxidant status (TAS), highlighting an imbalance in favor of oxidative damage74,75,76,77. Moreover, a recent randomized crossover study in healthy women demonstrated that prolonged mild sleep restriction markedly increased endothelial oxidative stress without activating compensatory antioxidant responses, due to reduced expression of DCUN1D3 gene, a regulator of the Nrf2-mediated antioxidant pathway, thereby suggesting a mechanistic link between insufficient sleep and vascular oxidative injury78. Finally, some antioxidant enzymes like glutathione peroxidase (GSH-Px) appear upregulated in rotating NS workers, possibly as a compensatory mechanism79.
However, findings are not uniformly consistent across all populations and biomarkers. Certain studies, such as those involving control room operators and refinery workers, report no significant differences in antioxidant enzymes (i.e., CAT and TTG), TAC, or lipid peroxidation markers (i.e., MDA) in correlation with NSW, although a borderline increase in OSI was noted in rotating NS healthcare workers80,81,82. Similarly, a recent study among Turkish nurses found no significant differences in oxidative stress parameters (TOS, TAS, cortisol, epinephrine, and norepinephrine) between day and NS workers, although higher perceived stress and anxiety sensitivity were associated with increased TOS and cortisol levels, suggesting that psychological stress may contribute to oxidative imbalance even in the absence of direct shift-related biochemical changes83. This variability might reflect differences in study designs, populations, sample types, or covariate controls, which often included age, sex, (body mass index) BMI, smoking, alcohol consumption, sleep duration, and additional work-related factors. In addition, a retrospective study in men seeking fertility assessment found that NS workers exhibited significantly higher systemic oxidative stress (measured by reactive oxygen metabolites species) compared to day workers. In in the NS group, antioxidant supplementation over three months led to a greater reduction in oxidative stress and improved semen quality, suggesting a potential benefit of targeted antioxidant therapy in mitigating NSW-related oxidative damage and infertility issues84.
Overall, the majority of evidence indicates that NSW significantly contribute to increased oxidative stress and DNA damage, along with diminished DNA repair capacity and altered antioxidant defenses, potentially underlying the elevated health risks, predisposing to several chronic diseases including cancer, observed in NS-working populations64,69,85,86. Intriguingly, melatonin supplementation improves oxidative DNA capacity (measured as urinary excretion of 8-OHdG) in NS workers, suggestive of a possible preventive intervention30.
Immune system impairment
Closely linked to oxidative stress is the deregulation of immune functions. Both preclinical and clinical studies have revealed that circadian misalignment compromises immune surveillance, reducing the capacity of the innate and adaptive immune systems to detect and eliminate emerging tumor cells63.
Experimental studies in rodents and other small mammals consistently demonstrate that disruptions to normal light-dark cycles (e.g., via phase shifts, continuous light or darkness, or dim LAN) can impair various components of the immune system, including natural killer (NK) cell activity, cytokine production, balance in white blood cell populations, and immune responses to pathogens, tumors, or injury87. For instance, repeated light-dark cycles reduced NK cell cytotoxicity and increased lung tumor burden in rats, while alternating light-dark cycles durations impaired both delayed-type hypersensitivity (DTH) responses and phagocytosis88,89. Always in rats, continuous light exposure led to diminished humoral responses and interleukin-2 (IL-2) secretion, as well as persistent disruption of circadian leukocyte rhythms and decreased number and activation of NK cells90,91. However, certain light-deprived conditions may enhance some immune parameters. For example, it has been proven that extended continuous darkness increased circulating T and B lymphocytes in rats92.
In diurnal animals like the Nile grass rat, dim LAN paradoxically enhanced immune markers including plasma IgG and DTH, whereas in nocturnal rodents, such as Siberian hamsters and C57BL/6 mice, dim light exposure and phase shifts typically led to immune suppression, delayed wound healing, reduced febrile responses to lipopolysaccharide (LPS), and diminished bactericidal activity93,94,95,96.
Additionally, in mice, phase shifts or LAN exposure altered cytokine expression and increased interleukin-6 (IL-6) levels, both systemically and following LPS stimulation97,98. Interestingly, it was recently found that chronic shift lag induces NK cells aging and impairs immunosurveillance99. Overall, the findings strongly support the conclusion that chronic or acute disruptions of circadian light-dark patterns impair immune competence, particularly innate immunity, cytokine signaling, with potential effects on BC development100,101,102.
Cross-sectional studies examining immune function in NS workers confirmed functional impairments in immune cell activity, even when total lymphocyte counts remain unchanged. For a summary of the worker findings, see Table 2. Independent studies across countries, including the USA, Japan, Germany, and Italy, reported no significant differences in total lymphocyte counts between DS and NS workers103,104,105,106. However, more detailed measures of immune competence reveal NSW-related suppression. For instance, several observations consistently proven that T-cell and lymphocyte proliferative responses were significantly reduced in NS workers compared to DS ones107,108,109,110. This reduced proliferation may indicate a diminished ability to trigger effective immune responses, including antitumor surveillance111. Supporting these findings, a large cross-sectional analysis from the Lifelines Cohort (11,000 individuals) demonstrated that NS workers exhibited significantly higher counts of leukocytes, monocytes, lymphocytes, and basophil granulocytes compared to non-shift workers, suggesting that frequent or consecutive NSW may acutely stimulate immune cell mobilization and contribute to systemic inflammation112.
In line with this, a study in rotating shift workers from the automotive industry found that NSW significantly reduced plasma concentrations of multiple immune markers, including pro- and anti-inflammatory cytokines (TNF-α, IL-2R, IL-1RA, IL-4, IL-12, IL-17), chemokines (IP-10, MIP-1α, MIP-1β, RANTES), and growth factors (EGF, FGF, VEGF), indicating a broad suppression of immune pathways linked to circadian disruption and higher susceptibility to infection and cancer113. Of particular relevance to cancer, NK cell activity, which plays a central role in recognizing and destroying tumor cells, was found to be significantly decreased in NS workers compared to DS114. This suppression of NK function has been hypothesized as a mechanistic link between NSW and increased cancer risk, especially for hormone-sensitive cancers such as BC115,116. Although these studies did not directly measure cancer incidence, the consistent finding of impaired NK cytotoxicity in NS workers supports the experimental evidence that links circadian disruption to reduced anti-tumor immunity107. Collectively, these findings align with broader epidemiological data suggesting that long-term NSW may contribute to BS risk, in part via suppressed immune surveillance mechanisms11.
Given the effects on immune health, NSW and sleep disruption can affect vaccine efficacy. Following meningococcal vaccination, it was observed that NS workers exhibit reduced deep and REM sleep, elevated inflammatory cytokines (TNF-α, IL-6), and diminished humoral immune responses. These immune deficits were also associated with altered circadian rhythms, reduced CD4 + T cells, and lower prolactin levels117. In a large hospital cohort, it was further investigated the impact of NSW on hepatitis B virus (HBV) vaccine response. NS workers showed reduced serum protection rates; however, after adjusting for demographic and occupational variables, NSW was no longer significantly associated with anti-HBs titers. This suggests that while NSW may influence immune status, its effects may be confounded by other risk factors118. Also, NS workers exhibited greater social jet lag, shorter sleep, and disrupted diurnal patterns in immune biomarkers such as IL-6, lymphocytes, and T-helper cells, thereby reducing vaccine efficacy119.
In the COVICAT study, which assessed antibody responses to COVID-19 vaccines in a general population cohort, all participants reporting short sleep duration had significantly reduced IgM levels. These results suggest sleep quantity, rather than NSW alone, may play a more direct role in modulating humoral immune responses120. In contrast, in a study aimed to characterize immune responses to mRNA COVID-19 vaccines among NS workers, despite significantly reduced sleep duration in NSW post-vaccination, no differences were observed in antibody titers compared to day workers. Notably, NS workers demonstrated stronger SARS-CoV-2-specific T-cell responses, and sleep metrics were not significantly associated with vaccine immunogenicity, suggesting that primary immune responses may be resilient to short-term sleep loss in healthy individuals121. Recent evidence further supports this link, showing that NS workers had a significantly higher risk of testing positive for SARS-CoV-2 compared to DS workers, suggesting that circadian disruption and sleep loss may increase susceptibility to infectious diseases through impaired immune regulation122. Consistent with these findings, a study of 1335 Norwegian nurses reported that NSW was associated with a higher prevalence of self-reported common cold, pneumonia/bronchitis, sinusitis, and gastrointestinal infections, highlighting the role of disrupted sleep and circadian misalignment in increasing susceptibility to infections123.
Inflammation
Together with immune deregulation, both LAN and NSW have also been associated with chronic low-grade inflammation, a recognized hallmark of cancer, including BC, as evidenced by elevated levels of pro-inflammatory cytokines and inflammatory markers in both animal models exposed to LAN and NS workers124 (Fig. 2).
Schematic representation of immune cell subsets affected by circadian disruption in night shift work. Each box depicts a cell type with altered functions and secreted molecules, including cytokines. Monocytes/macrophages: M2-like polarization. Basophils: acute mobilization. Neutrophils: systemic activation. CD8⁺/CD4⁺ T cells: reduced proliferation and activity. Treg cells: enhanced immunosuppression. NK cells: decreased cytotoxicity. Dendritic cells: impaired antigen presentation. B cells: diminished humoral response. These alterations promote chronic low-grade inflammation and reduced antitumor immune surveillance in long-term night shift work exposure. Selected elements adapted from Servier Medical Art (https://smart.servier.com, last accessed on 09 November 2025), licensed under Creative Commons Attribution 4.0 International License (CC BY 4.0; https://creativecommons.org/licenses/by/4.0/, last accessed on 09 November 2025).
Experimental studies conducted in animals over the past two decades consistently demonstrate that disruptions in the light-dark schedule induce inflammatory responses across a range of biological systems, with several findings suggesting potential relevance to BC. For instance, it was shown that repeated light-dark shifts in male C57BL/6 mice exacerbated colonic inflammation and tissue damage, pointing to heightened systemic inflammatory responses125. Further studies in Per2Luc knock-in mice revealed that chronic light-dark disruption elevated pro-inflammatory cytokines (e.g., IL1β, IL6, GM-CSF) and impaired host resilience to endotoxin challenge126. Also, it was confirmed persistent IL6 elevation, which is a pro-inflammatory cytokine strongly linked to BC progression127,128. Always in mice, long-term light-dark shifts compromised intestinal integrity and amplified alcohol-induced endotoxemia and hepatic inflammation, highlighting the involvement of the gut-liver-immune axis in circadian disruption129.
Complementary findings reported that mice exposed to LAN increased expression of IL6, IL1β, and TNFα, again highlighting mechanisms of inflammation with known cancer associations93,130,131. This was confirmed in rats, where continuous light significantly upregulated Stat3, IL1α, and IL17rα, gene products associated with pro-inflammatory immune regulation and BC oncogenesis132. Also, it was proven that light-induced circadian disruption primed a heightened pro-inflammatory TNFα response to LPS challenge, while immune imbalance, with increases in pro-inflammatory M1 macrophages and reductions in regulatory T cells, suggesting compromised anti-tumor immune surveillance133,134. A recent study further demonstrated that circadian regulation of mitochondrial function governs time-of-day-dependent activation of the NLRP3 inflammasome in macrophages, with peak inflammatory responses occurring when mitochondrial membrane potential is highest135. Collectively, these findings provide compelling experimental evidence that circadian disruption promotes chronic inflammation and associated immune system dysregulation136. In particular, the upregulation of IL6, IL1β, and Stat3, along with alterations in immune cell populations such as MDSCs and regulatory T cells, and inflammasome suggest plausible mechanistic links to BC pathogenesis137.
Several studies in workers further confirmed that NSW is associated with inflammatory alterations that are mechanistically relevant to BC pathogenesis. For a summary of the worker findings, see Table 3. These include elevated levels of c-reactive protein (CRP), IL-6, and increased monocyte counts, suggesting that circadian disruption through NSW may promote a pro-inflammatory and pro-tumorigenic immune environment138. In several independent studies it was observed elevated leukocyte counts in NS workers compared to DS workers, indicative of increased systemic inflammation139,140. Also, significantly lower TNF-α and IL-1β levels were measured in NS nurses compared to DS, and increased leukocyte counts and CRP levels were found in blood of Finnish airline workers engaged in rotating NS106,141.
Furthermore, significantly higher leukocyte counts and CRP levels were reported in both current and former NS workers, highlighting the long-term inflammatory effects of NSW142. Similarly, significantly increased IL-6 and LPS-binding protein levels were observed in US NS workers, indicating time-dependent immune activation143. In Italian nurses exposed to NSW elevated monocyte counts and CRP were reported. These findings are especially relevant to BC due to the involvement of chronic inflammation and monocyte-derived macrophages in tumor development144. A crossover study in Iranian NS workers demonstrated that night work significantly elevated pro-inflammatory markers, including IL-6, CRP, white blood cells, neutrophils, lymphocytes, and platelets, compared to DS workers, supporting a link between circadian disruption and triggering of systemic inflammation145. A transcriptomic study in healthcare NS workers demonstrated that a single NS can activate innate immune and inflammatory pathways, including Toll-like receptor signaling and cytokines such as IL-6 and IL-1β. Gene expression changes also involved pathways linked to autoimmune diseases, cancer, and major depressive disorder, indicating that even brief circadian disruption can trigger systemic inflammatory responses with potential long-term health consequences146.
Recent studies have continued to reinforce these associations. For instance, in healthcare workers, NSW was associated with elevated low-grade systemic inflammation, evidenced by higher leukocytes, TNF-α, IL-10, and LBP levels. Endotoxin tests further showed that long-term exposure impaired TNF-α reactivity, suggesting cumulative NSW increases inflammation-related disease risk, including cancer31. Furthermore, a UK Biobank study of over 350,000 adults found that poor sleep quality, extreme sleep durations, and permanent NSW were linked to higher blood pressure and elevated pro-inflammatory markers, including CRP and leukocyte counts. Although largely independent of age and sex, these effects were partially mediated by BMI147. Higher IL-6 levels were measured in NS workers compared to DS, implicating NSW in immune dysregulation148. Another study in contrast not report significant differences associated with NSW, possibly because of methodological limitations, such as the use of salivary cytokine measurements149.
Additionally, a 7-year prospective study found that while NSW alone was not significantly associated with chronic pain or CRP levels, the combination of NSW and moderately elevated CRP was associated with an increased risk of chronic pain and pro-inflammatory background150. A large cross-sectional study in electronics manufacturing workers further showed that NSW was associated with significantly elevated serum CRP levels, suggesting systemic inflammation and potential cardiovascular disease risk151. Consistently, NS healthcare workers were shown to have significantly higher levels of pro-inflammatory markers (i.e., CRP and TLC) than DS workers, with NSW, age, and BMI identified as independent predictors of elevated CRP152. Long-term NS workers exhibited significantly higher CRP-albumin and neutrophil-lymphocyte ratios compared to DS workers, supporting the presence of chronic low-grade inflammation associated with circadian rhythm disruption124.
A recent metabolomics study found that male NSW exhibited higher glycoprotein acetyls (GlycA), which is a marker of chronic low-grade inflammation, along with elevated triglycerides and fatty acids, indicating a potential sex-specific link between NSW, systemic inflammation, and metabolic deregulation153. Similarly, a UK Biobank study of 240,000 workers showed that long-term NSW increased the risk of irritable bowel syndrome (IBS), with higher shift frequency and duration predicting greater incidence154. A follow-up cohort study further demonstrated that this association is partly mediated by low-grade systemic inflammation, highlighting inflammation as a mechanistic link between chronic NSW and IBS risk155. Low grade inflammation in NS workers is also associated to other pathologies as demonstrated by a case-control study in psoriatic patients subjected to NSW, which showed higher disease severity and elevated IL-8 levels compared to DS workers. In these subjects, long-term NSW was also associated with higher BMI and hormonal changes, confirming that circadian disruption may exacerbate chronic inflammatory-linked conditions156. Collectively, these findings strongly suggest that exposure to NSW, induces systemic low-grade inflammation, likely through circadian disruption, and may contribute to the development of chronic diseases, including BC, highlighting the importance of occupational health strategies to mitigate these risks.
Disruption of melatonin chronobiology
As discussed above, a central mechanism that might trigger BC development, involves the suppression of melatonin synthesis by LAN157. Melatonin, secreted by the pineal gland in response to darkness, plays a key role in maintaining circadian homeostasis and exhibits broad oncostatic properties19. These include inhibition of tumor cell proliferation, promotion of apoptosis, suppression of angiogenesis, regulation of estrogen receptor expression, and modulation of immune activity158.
Results in rodent models have shown that exposure to LAN accelerates mammary tumor development, increases estrogenic activity, and reduces circulating melatonin levels159. In particular, the disruption of melatonin chronobiology due to alterations in the light-dark schedule can significantly affect tumor etiopathology, by altering cell proliferation, cell death, and nutrient supply160.
Across multiple experimental systems, primarily involving rodent models with implanted breast or liver tumors, the exposure to abnormal lighting conditions (e.g., continuous light, dim LAN, or intermittent light during the dark phase) consistently led to suppressed melatonin production and enhanced tumor growth dynamics161. For instance, in athymic nude rats with MCF-7 breast cancer xenografts, continuous light exposure significantly increased tumor growth and uptake of linoleic acid, which was metabolized into a mitogenic compound52. In a related study, rats exposed to varying intensities of nocturnal light showed dose-dependent melatonin suppression and increased tumor cell proliferation when perfused with blood collected from humans after nighttime light exposure. This effect was reversed by a melatonin receptor antagonist, indicating that melatonin directly mediated tumor-suppressive effects via MT1/MT2 receptors signaling54. Similarly, dim light during the dark phase accelerated tumor onset and growth in tamoxifen-treated breast cancer xenografts, alongside reduced melatonin levels162. However, not all studies supported a direct link between melatonin suppression and tumorigenesis. For example, in F344/N rats exposed to brief light pulses during the night following Neuromedin U treatment, melatonin levels were reduced, but no significant changes in mammary tumor development were observed163.
Numerous animal studies demonstrate that the administration of melatonin, alone or in combination with other agents, exerts significant anti-cancer effects in various animal models. Melatonin alone consistently reduces tumor growth, cell proliferation, and angiogenesis, as evidenced by decreased VEGF expression and micro-vessel density in xenograft and murine adenocarcinoma models161,164. It also promotes apoptosis through upregulation of p53-dependent pathways and cell cycle arrest at G1 phase, mediated by modulation of key downstream targets, such as FoxO1, miR-215, miR-96, CD44, survivin, and VEGF, thereby limiting tumor survival and metastasis165.
Intriguingly, when combined with other compounds, the anticancer efficacy of melatonin is enhanced synergistically. For example, its combination with thymoquinone induces extensive tumor necrosis, increases apoptosis, suppresses angiogenesis, and activates a T helper 1 (TH1) immune response, resulting in significant tumor size reduction and improved cure rates without liver toxicity166. Similarly, co-administration of melatonin with polyunsaturated fatty acids from walnuts modulates COX and LOX enzymatic activities, enhancing apoptosis, tumor immune infiltration, and survival in mammary adenocarcinoma167. Furthermore, melatonin combined with a ketogenic diet overcomes drug resistance to cisplatin and vincristine in BC-bearing mice by inducing apoptosis, inhibiting angiogenesis, lowering blood glucose, increasing ketone bodies, and downregulating resistance genes, achieving cure rates up to 70%168. Additional studies highlight the role of melatonin in enhancing the antitumor efficacy of chemotherapeutic agents administered at suboptimal circadian times, stabilizing tumors without added toxicity169.
Collectively, these preclinical findings demonstrate that melatonin bears multifaceted anticancer properties, ranging from direct tumor suppression and apoptosis induction to immune modulation and overcoming chemotherapy resistance. Hence this neuro-hormone may be positioning as a promising adjuvant in BC therapy. Importantly, these findings strongly support the “melatonin-estrogen hypothesis”, suggesting that melatonin suppression might facilitate estrogen-driven breast carcinogenesis170.
A substantial body of clinical evidence accumulated over the past two decades, consistently demonstrates that NSW is able to significantly suppress endogenous melatonin secretion, as measured through urinary and salivary metabolites, primarily aMT6s and 6-hydroxymelatonin sulfate (6-OHMS)171. For a summary of the worker findings, see Table 4. Early investigations in diverse occupational groups, including oil rig workers, telecommunications employees, and nurses, utilized 24-hour urine collections to compare melatonin output between DSW and NSW, often revealing reduced melatonin levels during NS or rotating shift schedules172,173,174. Similarly, a recent cross-sectional study in healthy nurses found that NS workers had significantly lower plasma melatonin levels compared to DS workers, alongside trends toward altered leptin, ghrelin, and metabolic parameters, supporting the role of circadian disruption in predisposing to metabolic syndrome, which is a risk factor for BC development175.
Large cross-sectional studies among healthcare professionals have repeatedly confirmed these findings. For instance, in premenopausal nurses it was reported a significant inverse relationship between the number of NS worked and urinary melatonin metabolite levels176. Similar reductions were observed across various workers cohorts, including manufacturing workers and healthcare workers. Importantly, these studies controlled for important covariates such as age, BMI, smoking, chronotype, and timing of sample collection, reinforcing the robustness of this association177,178,179,180,181,182.
Further, controlled clinical studies simulating NSW provide causal evidence that melatonin secretion diminishes rapidly upon night work exposure and remains suppressed with continued circadian disruption183. A study on hospital workers found that NS workers exhibited significantly greater social jetlag and correspondingly lower urinary aMT6s levels on workdays than days off. This reduction correlated with increased circadian misalignment184. Additionally, different lighting patterns on eight adults working night overtime were tested. Lower circadian stimulus increased melatonin and sleepiness, improving sleep quality, whereas higher stimulus suppressed melatonin but caused more morning sleepiness, suggesting that careful lighting design can reduce circadian disruption and enhance safety during NSW185.
Interestingly, the magnitude of melatonin suppression appears to correlate with both the frequency and duration of NS exposure186,187. For instance, in hospital nurses following a clockwise rapidly rotating shift schedule, salivary melatonin levels were maintained across DS and NS, indicating preservation of the normal circadian phase despite NSW188.
Recent researches have further examined the effects of melatonin supplementation and circadian factors on NS workers. A randomized, double-blind, placebo-controlled trial with shift workers suffering from sleep disorders demonstrated that 5 mg melatonin taken before sleep over four weeks significantly improved sleep quality and cognitive performance, with notable reductions in fatigue and good tolerability, supporting the role of melatonin in managing NSW-related sleep issues189. More recently, a randomized placebo-controlled trial on NS workers assessed melatonin supplementation before day sleep for four weeks, showing a significant increase in urinary 8-OHdG, biomarker of oxidative DNA damage repair, during day sleep30. Interestingly, a recent clinical trial in climacteric women working fixed shifts found that low-dose exogenous melatonin administered for three months did not significantly alter dietary intake or body composition, although postmenopausal participants showed modest reductions in fat mass, suggesting that physiological melatonin doses may have limited impact on metabolic outcomes in NS workers190.
Collectively, these studies underscore the potential role of the neuro-hormone melatonin in mitigating circadian disruption and improving physiological and cognitive outcomes in NS workers, emphasizing the importance of implementing chronobiological strategies in occupational health191. However, despite these promising findings, it remains unclear how chronic melatonin supplementation affects long-term health outcomes in shift workers. Melatonin is popular for its sleep-regulating effects, and short-term use appears safe, but further research is needed to evaluate its broader impacts, including cardiovascular health, before it can be considered a “wonder pill” for NS workers192. Furthermore, while most findings indicate lower melatonin levels during NS compared to DS, some variability arises due to factors such as seasonality and specific shift schedules173,193. Nevertheless, the majority of data supports that NSW disrupts normal circadian melatonin rhythms, which may underlie increased health risks, including BC, associated with chronic circadian misalignment. This highlights the urgent need for identification of effective targeted strategies to protect shift workers from the adverse biological effects of circadian disruption194. Supporting the genetic basis of these associations, a recent hospital-based case-control study in Korean women identified variants in the melatonin receptor gene MTNR1A that were linked to BC risk, with certain polymorphisms interacting with NSW to further elevate susceptibility, highlighting a gene-environment interplay in circadian disruption-mediated breast carcinogenesis195. Additionally, recent evidence suggests that melatonin secretion patterns in NS workers are associated with differential DNA methylation in melatonin receptor gene MTNR1A and other circadian genes, potentially linking altered melatonin rhythms to increased cancer susceptibility196.
Intriguingly, growing evidence suggests that circadian rhythm disruption plays a critical role not only in BC progression but also in therapeutic response, with particular implications for melatonin as a therapeutic target. A recent study revealed that triple-negative breast cancer (TNBC) exhibits the most severe circadian rhythm disruption among all subtypes, marked by loss of rhythmic gene expression, metabolic reprogramming, and an immunosuppressive microenvironment. Notably, TNBC tumors with high-circadian rhythm disruption score were associated with decreased melatonin biosynthesis and increased tryptophan metabolism, associating melatonin suppression with immune evasion and poor relapse-free survival197. These findings align with preclinical data showing that circadian disruption enhances TNBC tumor growth and impairs the time-dependent efficacy of cisplatin therapy, suggesting that both intact circadian signaling and melatonin rhythms are crucial for optimizing chemotherapeutic outcomes58.
Meanwhile, in luminal A tumors, circadian rhythms remain partially intact but reprogrammed. Paradoxically, stronger tumor-intrinsic circadian rhythmicity was associated with worse five-year survival, mediated by rhythmic expression of epithelial-to-mesenchymal transition (EMT)-related genes and enhanced metastatic potential27. On the therapeutic side, a recent clinical study on BC survivors found that chronotype-tailored light therapy, which can modulate melatonin production, significantly reduced fatigue and improved sleep quality198. Altogether, these studies suggest that both melatonin and treatments aimed to remodulate circadian homeostasis hold promise not only in enhancing treatment efficacy and quality of life, but also in potentially counteracting immunosuppressive and pro-metastatic mechanisms driven by circadian disruption in BC patients.
Clock genes alterations
In addition to melatonin-dependent mechanisms, recent research has highlighted the importance of core circadian clock genes (e.g., CLOCK, BMAL1, PER1/2/3, CRY1/2, and NPAS2) in the regulation of pathways central to tumor biology199. These genes govern cell cycle checkpoints, DNA damage repair, metabolic regulation, and apoptosis. Experimental disruption of these genes in cellular and animal models has been shown to enhance genomic instability and promote malignant transformation. For example, knockdown of PER1 or CRY2 in mammary epithelial cells impairs cell cycle control and facilitates oncogenic behavior, while mouse models with mutations or deletions in circadian genes develop spontaneous tumors or exhibit heightened sensitivity to mammary carcinogens200.
Experimental studies investigating clock gene disruption and carcinogenesis have demonstrated several mechanisms relevant to BC risk. For instance, disruption of circadian rhythms by repeated advances in the light-dark schedule in rodent models consistently altered expression of core clock genes such as Per2 and Bmal1, leading to impaired immune function, including reduced NK cell cytotoxicity and decreased expression of cytolytic factors like IFNγ, perforin, and granzyme B. This immunosuppression was linked to increased tumor incidence88. In Wistar rats, shifts in light exposure altered peripheral clock gene expression and increased inflammatory markers and estrogen receptor expression in white adipose tissue, suggesting that circadian disruption may enhance estrogen-mediated pathways, which are known to be involved in breast carcinogenesis201.
Mice exposed to altered light-dark cycles also exhibited disrupted Per2 rhythms alongside chronic inflammation characterized by elevated IL-1β, IL-6, and TNF-α, and changes in macrophage populations favoring pro-inflammatory phenotypes126,202. Moreover, advanced light-dark schedules in genetically predisposed mice (e.g., K-ras/p53 mutants) led to enhanced tumor growth and cell proliferation with increased oncogene c-Myc expression, while clock gene knockouts have tumor suppressive effects203. Altogether, these experimental data reveal that circadian disruption affects multiple BC-related hallmarks including immunosuppression, chronic inflammation, altered hormone receptor expression, and dysregulated cell proliferation204.
Studies examining clock gene sequence, expression and methylation in NS workers reveal notable disruptions linked to BC-related pathways. For a summary of the worker findings, see Table 5. Several cross-sectional studies among nurses and healthcare workers consistently found that NSW alters the expression of key clock genes in blood mononuclear cells. For example, NS nurses in Poland showed increased PER1 expression, especially after ≥15 years of NSW205. Italian nurses on rotating NS had higher expression of BMAL1, CLOCK, NPAS2, PER1, PER2, and REV-ERBα but lower expression of PER3, CRY1, and CRY2 than DS nurses206. Similar findings of increased PER2 expression in short-term rotating NS were observed in American hospital residents207. Conversely, some studies reported decreased amplitude of PER1 expression following NSW schedules, indicating complex effects depending on shift duration and design208. Consistent with these studies, a recent study in healthy NS workers demonstrated that moderate alcohol consumption further altered peripheral clock gene amplitude in CLOCK, BMAL1, PER1, CRY1, and CRY2, and it was associated with increased colonic permeability, highlighting the compounding effects of environmental circadian disruption and lifestyle factors on peripheral clock gene regulation143.
Further supporting these findings, a recent study on Japanese male workers demonstrated that clock gene expression rhythms in beard hair follicle cells varied with shift work type. Specifically, PER3 expression was significantly reduced and circadian rhythmicity disrupted in workers on multiple consecutive NS compared to those on a single NS or daytime shifts209. Additional molecular evidence indicates NSW induces a state of circadian misalignment marked by upregulation of key clock genes including BMAL1, CLOCK, PER1, PER2, and PER3. This dysregulation correlates with elevated night-time blood pressure and disrupted nocturnal dipping patterns, linking circadian gene dynamics also to cardiovascular risk in shift workers210. Importantly, the EuRhythDia study explored the effects of timed light therapy on circadian and metabolic regulation in rotating NS workers. While 12 weeks of bright light exposure did not produce measurable improvements in sleep quality, glucose metabolism, or inflammatory markers, it significantly altered clock gene expression in peripheral blood mononuclear cells (PBMCs, specifically decreasing REV-ERBα levels and increasing the REV-ERBα/BMAL1 ratio). These gene expression changes partially persisted after the intervention, suggesting that light therapy can modulate molecular circadian rhythms in NS workers, underscoring the potential use of circadian gene markers as early indicators of intervention efficacy in occupational chrono-medicine211. A recent clinical study further confirmed that NSW disrupts 24-hour rhythms of PER2, PER3, BMAL1, and ESR2 in PBMCs, impairs the inverse correlation between PER2 and BMAL1, and alters PER1 and ESR1 expression patterns, highlighting a misalignment in the peripheral circadian network associated with NSW schedules212. Altogether, these findings highlight the broader systemic impact of circadian disruption induced by NSW, which encompasses cancer susceptibility, metabolic disorders, and cardiovascular dysfunction.
Regarding epigenetic modifications, methylation patterns of clock genes differ between NS and DS workers, with potential implications for BC risk. Female healthcare workers showed significant hypomethylation of multiple clock genes including CLOCK, PER1, PER2, PER3, and NPAS2 in NS workers, which may reflect altered gene regulation213. Genome-wide methylation comparisons between 65 DS and 59 NS healthcare workers revealed 21 loci in circadian genes, including PER3 and CSNK1E, to be significantly hypomethylated among NSW, highlighting potential epigenetic mechanisms underlying shift work-associated disease risk214. Similarly, a study focusing on CLOCK-related circadian regulators in nurses, found that hypermethylation in BMAL1 gene bodies was associated with working ≥3 consecutive NS per week, suggesting possible epigenetic silencing affecting CLOCK transcriptional activity. Also, prolonged NSW ( ≥ 10 years) correlated with hypomethylation in NR1D1, and hypermethylation of CSNK1E, a kinase regulating PER proteins downstream of CLOCK215. In line with these findings, a Danish pilot study demonstrated promoter hypomethylation of CLOCK and hypermethylation of CRY2 in peripheral blood DNA, potentially mediating the relationship between NSW and BC susceptibility216. Complementing these targeted analyses, a recent epigenome-wide association study demonstrated sex-specific DNA methylation changes and epigenetic age acceleration, including the differential methylation in both CRY2 and RORA, linking NSW to epigenetic alterations in circadian regulators33. Additionally, melatonin secretion patterns in NS workers were associated with differential methylation of key circadian genes, including RORA, MTNR1A, and PER3, suggesting a potential link between circadian disruption, epigenetic regulation, and cancer risk196.
Moreover, genetic studies among Korean women revealed significant associations between circadian gene variants and BC risk. The CLOCK gene variant rs11133373 was linked to increased BC risk, while the MTNR1A gene variant rs2119882 was associated with reduced risk. Crucially, interactions between NSW and specific polymorphisms in CRY2 and RORA further elevated BC risk, underscoring the complex interplay of genetic susceptibility and environmental circadian disruption in BC etiology195. Beyond cancer-related effect, it was also observed within a cohort of steelworkers that the presence of CLOCK rs1801260 and MTNR1A rs2119882 polymorphisms combined with rotating NSW, significantly increased the risk of type 2 diabetes217. Additionally, a study on healthcare workers investigated CLOCK, BMAL1, and PER1 polymorphisms in relation to hypertension, finding that the CLOCK rs1801260 GG and BMAL1 rs11022775 TT genotypes were associated with a reduced risk of hypertension, whereas PER1 rs2735611 showed no significant association, highlighting how circadian gene variants may influence cardiovascular outcomes in NS workers218.
Collectively, these data demonstrate that NSW disrupts both the expression and methylation status of core circadian clock genes involved in BC etiology, such as PER1, PER2, BMAL1, and CLOCK (Fig. 3). These molecular alterations likely affect circadian regulation of hormone receptor pathways, cell cycle control, and DNA repair, potentially contributing to increased BC susceptibility observed in epidemiological studies26. Additionally, specific polymorphisms in clock genes may affect individual vulnerability to circadian disruption, thereby influencing the extent to which NSW impacts BC risk and related molecular pathways219. The integration of genetic, epigenetic, and gene expression data across diverse populations and models may provide a more comprehensive understanding of the molecular mechanisms linking circadian disruption with cancer and other NSW-related health risks.
Schematic representation of the core circadian clock feedback loops showing how night shift work alters clock gene expression and DNA methylation. A The CLOCK-BMAL1 complex activates PER and CRY transcription via E-box elements. B ROR and REV-ERB regulate BMAL1 expression through RRE sites. Red arrows indicate changes in gene expression, while red “M” denotes altered DNA methylation in clock genes, both associated with night shift work.
Epigenetic changes
Growing evidence from both experimental models and human studies reveals that circadian disruption caused by altered light-dark cycles and NSW may lead to diverse epigenetic alterations. For a summary of the worker findings, see Table 6. For instance, changes in DNA methylation patterns, histone modifications, as well as circulating miRNA expression alterations may affect critical biological pathways, thereby influencing health outcomes in NS workers220. In experimental studies exploring the epigenetic effects of disrupted light-dark cycles, various types of epigenetic alterations (e.g., DNA methylation, histone modifications, and miRNA expression) have been observed across different animal models. In detail, it was observed that repeated 3 h phase advances in the light-dark cycle over several days increased DNMT1 protein levels in rat liver221. Furthermore, exposure to dim light during the dark phase in rats with MCF-7 tumors induced Stat3 gene expression via promoter methylation of ARHI222. Histone modifications were also reported. In particular, rapid trimethylation of histone H3 at lysine 4 (H3K4me3) was observed in mouse livers after weekly 6-hour light-dark phase advances223.
Additionally, miRNA alterations have been found as well, as it were shown decreased miR-127 and miR-146-b levels in rat mammary tissues following both acute and prolonged light-dark alterations221. Subsequently, it was observed that altered lighting (i.e., abrupt light-dark shifts and light intensity changes) in Syrian hamsters modulated expression of miR-132, miR-212, and their target MeCP2 in SCN tissue224. Finally, increased liver expression of several Rev-erbα-targeting miRNAs (miR-140-5p, miR-185-5p, miR-326-5p, and miR-328-5p) in mice exposed to continuous light for 8 weeks were also reported225. These findings collectively demonstrate that circadian disruption via altered light exposure can induce diverse epigenetic responses depending on tissue, timing, and species.
Multiple studies have investigated the effects of NSW on DNA methylation patterns in blood cells, revealing a range of epigenetic alterations associated with circadian disruption, immune regulation, and aging. These changes can be categorized broadly into global/repetitive element methylation, gene-specific methylation, miRNA methylation, epigenetic clock genes alterations (see above), and methylation of immune- and retroviral-related elements204.
Early cross-sectional research in Italian chemical plant workers found no significant differences in methylation of repetitive elements such as Alu and LINE-1, or in inflammatory genes like TNFα and IFNγ, despite exposure to NSW226. Similarly, no significant changes in LINE-1 and Alu methylation among female nurses was observed, although several gene-specific hypomethylation effects to the estrogen receptor gene ESR1 (associated with heightened estrogen sensitivity), to the tumor suppressor genes TP53 and BRCA1 (indicating possible disruption in cell cycle regulation and DNA repair mechanisms) were reported. These findings suggest that repetitive element methylation may be less sensitive or not consistently altered by NS exposure compared to specific gene methylation227. Indeed, significant gene-level methylation changes have been consistently reported in various cohorts. For example, it was demonstrated hypermethylation in multiple CpG sites in NS workers216. Additionally, always in NS workers it was observed hypermethylation in 48 CpGs across 29 miRNAs, as well as 20 hyper- and 30 hypo-methylated CpGs within 56 imprinted genes228,229. In line with these findings, overall lower DNA methylation was reported in NS healthcare workers compared to DS workers in an American cohort, upon adjustments for confounders such as immune cell composition214. Contrariwise, no methylation differences specific to BRCA1/BRCA2 gene promoters were observed among rotating NS nurses230.
More recent work linked long-term NS work ( ≥ 10 years) to significant hypomethylation in 85 CpG sites, including loci in ZFHX3, a gene involved in circadian rhythm regulation and tumor suppression, and ATXN7, associated with transcriptional control and cancer susceptibility231. The same group demonstrated that NSW is associated with biological age acceleration, indicating an average age advancement of over three years in women with ≥10 years of NSW231. These findings were further corroborated within the Lifelines Cohort, where results showed sex- and duration-specific DNA methylation changes in women exposed to intermediate-term NSW (10-16 years), enriched in pathways related to circadian regulation and cellular senescence. Notably, short-term NS workers (2-6 years) of both sexes exhibited increased epigenetic age acceleration, possibly reflecting early biological stress with adaptation over time33.
Among the earliest specific findings, a total of 50 loci corresponding to 31 miRNA promoters were found differentially methylated in NS workers compared to DS workers, including the circadian miR-219228. In line with these results, also the promoter of miR-34b, a miRNA relevant in BC susceptibility and involved in tumor suppression and cell cycle control, was found hyper-methylated in women exposed to NSW compared to non-exposed controls232.
Going deeply into mechanistic advances, it was demonstrated that altered melatonin secretion patterns in NS workers correlate with DNA methylation changes in circadian genes. In particular, it was observed increased methylation in the gene body of RORA clock gene and decreased methylation in the promoter of MTNR1A melatonin receptor gene196. Supporting these findings, a recent study in female healthcare workers demonstrated that NSW parameters, including current status, duration, and intensity, were associated with differential methylation in key circadian genes such as CSNK1E, NR1D1, and ARNTL215. These epigenetic modifications suggest a mechanistic link between melatonin disruption, NSW features, circadian gene regulation, and potential BC risk233.
Additionally, NSW affects methylation of immune-modulatory genes and human endogenous retroviral elements such as ERVFRD-1, HERV-L, and HERV-P, indicating combined effects of circadian and metabolic stressors on immune epigenetic regulation234. Interestingly, DNA methylation dynamics vary during recovery from shift work disorder (SWD). It was found that vacation periods reversed hypomethylation accumulated during NSW, particularly in genes involved in glutamatergic neurotransmission and immune pathways, including CREB1, CAMK2B, and GRIN2C, highlighting the plasticity of epigenetic landscape in response to circadian stress and recovery235.
Overall, the body of research indicates that NSW induces complex, multi-level epigenetic changes encompassing miRNAs, circadian and tumor suppressor genes, melatonin-related genes, immune regulators, and endogenous retroviral elements. These methylation alterations are often duration- and sex-dependent and relate to accelerated biological aging, disrupted circadian regulation, immune dysfunction, and potentially increased BC risk. However, the heterogeneity in study designs, populations, and covariates underscores the need for larger, longitudinal, and mechanistically focused investigations to fully elucidate the epigenetic consequences of NSW exposure and deriving health issues.
Telomere shortening
Shorter telomere length is associated with a higher risk of BC recurrence, suggesting its potential as a prognostic biomarker for disease-free and recurrence-free survival236. In this context, the relationship between NSW and telomere length has been examined in several human studies with mixed results. For a summary of the worker findings, see Table 7. Large cross-sectional analyses from the USA, including the Sister Study with 608 women and the Nurses Health Study (NHS) with over 2400 nurses, found no significant association between the duration of rotating NSW and telomere length after adjusting for multiple covariates such as age, BMI, smoking, and stress. These findings suggest that moderate or shorter-term exposure to NSW may not substantially affect telomere length237,238. In contrast, evidence from a Norwegian nested case-control study involving hospital nurses demonstrated statistically significant telomere shortening associated with long-term NS ( ≥ 6 consecutive nights, for ≥5 years). This indicates that extended exposure to consecutive NS may accelerate telomere erosion, consistent with the hypothesis that chronic circadian disruption can promote cellular aging239. Complementary with these findings, it was also demonstrated a non-linear association between NS duration and telomere length among female hospital nurses. In this study, it was observed that telomere length increased with NSW exposure up to about 12 years, but then significantly decreased with longer exposures ( ≥ 12 years). This biphasic pattern could reflect initial compensatory telomere maintenance or cellular stress responses in early years of NS work, followed by accelerated telomere shortening as cumulative damage and circadian disruption intensify over time227.
Supporting these results, a recent cross-sectional study of hospital workers reported that leukocyte telomere length was positively associated with plasma PTX3 levels, suggesting that efficient regulation of inflammatory processes may protect telomeres from attrition, even in NS workers144. Also, evidence from a population-based study indicates that obstructive sleep apnea is consistently associated with accelerated epigenetic ageing, while the impact of insomnia and sleep deprivation appears to be modulated by the duration of NSW schedule, highlighting a complex interplay between sleep disturbances, NSW, and biological aging240. Consistent with these observations, a study in older workers reported that current NS workers had significantly shorter telomeres than non-shift workers, while former NS workers showed partial recovery of telomere length with increasing time since cessation, suggesting that NS-induced telomere attrition may be at least partially reversible241.
Collectively, these data imply that the impact of NSW on telomere length may depend on the duration and intensity of exposure, with short to moderate durations having a limited effect, but long-term or consecutive NS contributing to telomere shortening and potentially premature cellular aging. This progressive telomere shortening in long-term NS workers could partially explain the observed increases in age-related diseases and cancer risk in this population. However, discrepancies across studies highlight the need for robust longitudinal research with precise exposure assessment and consideration of specific confounders, such as lifestyle and chronotype.
Other factors
Vitamin D deficiency has also emerged as a potential contributor to the elevated BC risk observed in NS workers. For a summary of the worker findings, see Table 8. Reduced sunlight exposure due to altered sleep-wake patterns and nighttime work schedules can lead to suboptimal cutaneous synthesis of vitamin D, a hormone with well-documented anti-proliferative, pro-apoptotic, and immunomodulatory effects in breast tissue242. Observational studies have reported lower serum vitamin D levels among NS workers188,243,244,245,246. Furthermore, results in NS workers support a role for vitamin D in regulating circadian gene expression, while also interacting with estrogen pathways, inflammatory signaling, and sleep quality247,248. Also, evidence from male rotating shift workers indicates that vitamin D deficiency is associated with a higher risk of obstructive sleep apnea, highlighting another potential health consequence of low vitamin D in shift-working populations249. These findings suggest that vitamin D deficiency may act as both a consequence and a mediator of circadian misalignment, potentially compounding the carcinogenic effects of LAN exposure and reinforcing the need to consider vitamin D status in risk stratification and prevention strategies for NSW-exposed individuals250.
In addition, over the past decade, numerous cross-sectional studies have investigated the effects of NSW work on several other hormonal levels among female healthcare workers, revealing complex and sometimes contradictory patterns251. For a summary of the worker findings, see Table 9. Early research from the American NHS I found increased estradiol but not estrone, among postmenopausal women with prolonged rotating NS exposure, along with a modest inverse correlation between follicular estradiol and melatonin metabolite levels, suggesting circadian regulation of estrogen synthesis176,252. Similarly, within Japanese nurses with NSW history, it was reported elevated estrone in postmenopausal253. In Italian premenopausal nurses on rapid forward-rotating NS, it was also observed significantly higher 17-β-estradiol, especially among those who skipped naps during shifts180,206.
Contrastingly, a Canadian study found no clear estrogen associations in nurses working NS, while in American nurses it was documented elevated estrogen, LH, and FSH levels following daytime sleep after NSW254,255. In Spanish female healthcare workers was found an association between rotating NS and increased estradiol, as well as progesterone, modulated by menstrual phase, whereas in Greek hospital NS workers elevated progesterone and androgens, but not estrogen, were confirmed256,257. These findings were further refined by findings demonstrating that estradiol increased with years of NSW only in postmenopausal mid-ages female nurses who show a morning chronotype, highlighting chronotype as a possible modulating factor258.
More recent investigations evidenced how women working whole NS exhibit suppressed estradiol levels compared to DS workers, coinciding with disrupted sleep and melatonin rhythms, while half-NS did not significantly affect estradiol synthesis259. At the molecular level, healthy DS nurses showed robust circadian oscillations of the estrogen receptor gene ESR2 in PBMCs, peaking in the morning. However, this rhythm was lost in NS nurses, indicating that NSW disrupts normal temporal regulation of estrogen receptor expression and may contribute to altered estrogen signaling212. Finally, in a cohort of female hospital workers, rapid rotating NS was linked to increased serum release of stress-related steroids-corticosterone, 11-deoxycortisol, DHEA, and androstenedione, whereas estradiol levels were slightly decreased, and salivary estradiol remained unchanged, suggesting a complex and multifaceted influence of NSW on estrogen regulation188.
Together, these findings underscore that NSW alters estrogenic activity in women, primarily through elevated estradiol in certain populations, with stronger effects in postmenopausal women and modulation by chronotype and circadian disruption251. However, the suppression of estradiol observed in whole-NS workers and the loss of estrogen receptor rhythmicity highlight the nuanced and context-dependent nature of endocrine disruption caused by shift work251. This complexity suggests that altered estrogen signaling may represent a key mechanistic pathway linking NSW to BC risk and warrants further investigation considering individual circadian profiles and shift patterns.
Although beyond the primary scope of this review, it is worth mentioning that emerging evidence highlights the gut microbiome as a potential mediator of circadian disruption-associated breast carcinogenesis, with studies indicating that NSW can alter microbial composition and diurnal rhythmicity, thereby modulating systemic inflammation, estrogen metabolism, and immune function, all of which are relevant to BC risk260.
Precision biomarkers for women exposed to night shift work
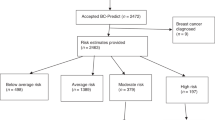
Emerging evidence underscores the urgent need to incorporate novel biomarkers to identify women who are particularly susceptible to the adverse effects of NSW, especially those at increased risk of developing BC or who already exhibit early biological signs of exposure-related harm261. Historically, most biomonitoring in NSW contexts has relied either on the detection of melatonin synthesis suppression or general markers of inflammation or biological signs of sleep disturbance262,263,264. In light of the recent mechanistic findings, a more refined panel of biomarkers might be proposed to enhance early risk stratification, prevention, and personalized interventions in occupational health (Fig. 4)265.
The figure illustrates key sample types (blood, urine, saliva, stool, biopsy) and associated biomarkers, including indicators of oxidative stress, inflammation, immune function, endocrine disruption, circadian-relevant gene alterations (including clock genes and melatonin pathway genes), and gut microbiota imbalance. Selected elements adapted from Servier Medical Art (https://smart.servier.com, last accessed on 09 November 2025), licensed under Creative Commons Attribution 4.0 International License (CC BY 4.0; https://creativecommons.org/licenses/by/4.0/, last accessed on 09 November 2025).
For instance, oxidative stress is a well-documented mediator of LAN-induced carcinogenesis. Specific biomarkers like 8-OHdG and 8-isoprostane are validated indicators of oxidative DNA and lipid damage, respectively, and are consistently elevated in blood from female NS workers266. Additional markers such as SOD, CAT, MDA, TOS, and TAC/TAS support a comprehensive profile of oxidative burden86. Longitudinal monitoring of these biomarkers may help identify individuals with persistent redox imbalance and stratify risk by exposure duration and chronotype.
Also, chronic circadian misalignment leads to immune suppression and low-grade systemic inflammation, both of which contribute to impaired tumor immunosurveillance146. In addition to elevated CRP, IL-6, and TNF-α, shift workers show altered immune profiles such as a reduced CD4 + /CD8 + T-cell ratio, increased monocyte counts, and impaired NK cell cytotoxicity. Measuring these markers may help detect early immune dysregulation in at-risk women262.
Melatonin remains a cornerstone biomarker of circadian health267. Decrease of urinary aMT6s and 6-OHMS is associated with increased BC risk and is easily measured via non-invasive urine assays268. Disruption of MT1 and MT2 melatonin receptors, implicated in antiproliferative signaling, has also been reported in LAN-exposed tissues269. These markers, measured for example in peripheral blood cells, could provide a dynamic measure of melatonin pathway disruption over time.
Furthermore, dysregulation of core clock genes such as CLOCK, BMAL1, PER1/2, CRY1/2, and NPAS2, both at the transcriptional and post-translational levels, is consistently observed in PBMC samples of shift workers and may serve as early predictors of disrupted cell cycle control, DNA repair, and apoptosis. Specific polymorphisms, such as CLOCK rs11133373, PER3 VNTR, and MTNR1A rs2119882, have been associated with differential susceptibility to circadian misalignment and cancer risk270, hence they can be used for risk stratification purposes.
Recent findings reveal that NSW disrupts the gut microbiota’s diurnal oscillations, impairing estrogen metabolism via altered expression of bacterial β-glucuronidase and contributing to systemic inflammation271. Markers of microbial dysbiosis, such as shifts in the Firmicutes/Bacteroidetes ratio, reduction in butyrate-producing species, and increased LPS levels, may serve as early indicators of circadian-gut axis dysfunction260.
Concurrent deficiencies in vitamin D, likely due to reduced sunlight exposure, and fluctuations in estradiol, progesterone, and DHEAS, especially among premenopausal women and extreme chronotypes, further exacerbate endocrine disruption272. The detection of all these parameters through non-invasive or minimally-invasive measurements could help risk stratification among female NS workers.
To date, occupational health assessments for NS workers, particularly women, have underutilized mechanistic biomarkers capable of detecting early and personalized signs of biological disruption273. The integration of specific, validated markers will enable early detection of high-risk individuals, dynamic monitoring of exposure effects, and, finally, the development of chrono-medicine-dictated interventions aimed at prevention, mitigation, and tailored policy-making274. By integrating biomarker profiles with genetic susceptibility and exposure history, future studies may develop predictive models that could implement targeted surveillance and preventive interventions tailored to the unique biological impact of occupational circadian disruption273.
Correlation between night shift work and breast cancer risk in female workers
The potential association between NSW and BC risk has been extensively investigated over the past three decades through population-based case-control and large prospective cohort studies1. While several studies suggest that chronic circadian disruption from NSW may modestly elevate BC risk, findings have been heterogeneous and at times conflicting, reflecting variation in study design, exposure definitions, and adjustment for reproductive and lifestyle factors (Tables 10–11).
This section summarizes the evolution of epidemiologic evidence, from 1996 to the present time275. The epidemiologic literature before 2019 presented mixed evidence linking NSW to BC. Two major authoritative assessments synthesized these findings: the U.S. National Toxicology Program (NTP) and the IARC276,277. Both concluded that human evidence for the carcinogenicity of NSW was limited. In detail, the NTP determined there was strong, though not sufficient, evidence for persistent NSW (long-term, frequent, or beginning at an early age), supported by mechanistic data on circadian disruption, while IARC classified NSW as probably carcinogenic to humans (Group 2 A) based on limited human and sufficient animal evidence276,277.
As summarized in Table 10, individual studies reported variable results. For instance, early case-control analyses yielded both positive and inverse associations, while more recent pooled analyses suggested only borderline increased risk278,279,280. Occupational cohorts of Norwegian and Danish nurses and militaries, as well as the Swedish Work, Lipids and Fibrinogen (WOLF) cohort indicated higher BC risk with ≥20-30 years of NSW281,282,283,284,285,286,287. Additionally, two Chinese cohort studies found that NSW was associated with increased risk of BC, along with a dose-response relationship per cumulative hour-year of exposure288,289. Whereas large prospective cohorts, such as the Shanghai Women’s Cohort, the UK Million Women Study, the Swedish twin cohort, and the Dutch National Cohort reported null associations290,291,292,293,294.
The NHS II observed elevated risk with ≥20 years of NSW, while NHS I and payroll-based cohorts were mixed or null295,296,297,298. Intriguingly, risk appeared greater among premenopausal women, as well as for estrogen receptor-positive BC cases280,296. Genetic susceptibility has also been explored, reporting a possible interaction between CLOCK gene polymorphism and NSW299. Nonetheless, multiple sources of bias likely influenced results, including exposure misclassification (es., current shift status used as proxy for lifetime exposure), survivor bias and left truncation in cohorts, and incomplete control for reproductive or behavioral confounders276. Heterogeneous NSW definitions (i.e., rotating versus permanent schedules, varying duration thresholds) further limited comparability among studies277.
Since 2020, several clinical studies have further evaluated the association between NSW and BC risk using improved exposure characterization and analytical designs. Among the twelve studies identified, six were included in the 2022 systematic review and meta-analysis by Hong et al. while six more recent investigations (published after that review) are newly discussed in the present work138. Definitions of NSW differed among studies but generally involved working during night hours for specified durations or frequencies, commonly ≥10 years or ≥10 NS per month. Data collection methods ranged from structured interviews and questionnaires to registry-based employment records and JEM. The studies were variably adjusted for potential confounders including age, reproductive history, smoking status, BMI, breastfeeding, socioeconomic status, and family history of BC (Table 11).
Case-control studies from Mexico, Korea, Poland, China, and Spain reported significant associations between long-term NSW and BC risk. In Mexican women, Bustamante-Montes et al. found markedly increased risk for ≥10 years of NSW (OR = 8.58, 95% CI 2.19–33.8), with early menarche amplifying risk and breastfeeding conferring protection300. Korean data linked NSW with circadian gene variants in CLOCK, CRY2, and RORA, while Polish studies demonstrated dose-response correlations and higher risks for backward-rotation schedules (OR = 3.31)195,301,302. Similar positive findings emerged among Chinese healthcare workers and Spanish nurses303,304.
By contrast, cohort studies reported more shaded results. Among Norwegian offshore petroleum workers, NSW was not associated with BC (HR = 0.87, 95% CI 0.52–1.46)305. The U.S. Sister Study observed a modest risk with short-term NSW (HR = 1.12, 95% CI 1.00–1.26) but none for long-term exposure306. The Canadian Census Health and Environment Cohort also found no increased risk (HR = 0.94, 95% CI 0.90–0.99), although exposure estimates relied on job-exposure matrices lacking behavioral detail307.
Nordic registry studies provided mixed evidence. In Finnish public-sector employees, risk doubled among women ≥50 years with ≥10 years of NSW (OR = 2.05, 95% CI 1.04–4.01)308. The Swedish Healthcare Worker study identified elevated postmenopausal BC risk with ≥8 years of NSW (HR = 4.33, 95% CI 1.45–10.57), although based on few cases309. The Older Finnish Twin Cohort found increased BC risk (HR = 1.58, 95% CI 1.16–2.15), particularly in younger women (born 1950–1957; HR = 2.08, 95% CI 1.32–3.28). Whereas, direct co-twin comparisons suggested effects independent of shared genetics or environment310.
Overall, the novel body of evidence on exposed workers supports an association between NSW and increased BC risk, with risk magnitude influenced by duration, shift rotation patterns, and genetic susceptibility. Several studies, particularly from Poland, Mexico, Korea, and Spain, report ORs ranging from approximately 2 to over 8, with stronger associations for long-term NSW ( ≥ 10 years) and specific genetic polymorphisms in clock genes and melatonin receptors genes. Indeed, protective factors such as breastfeeding also emerged in some studies195,300,303,304. Conversely, large prospective cohorts and population-based studies, like for the past population studies, present more nuanced findings, with some reporting no association, possibly due to “healthy worker effects”, differential exposure misclassification, or lack of detailed shift characteristics. Importantly, the impact of shift intensity, timing, and chronotype remains underexplored306,308,309.
Common limitations include the reliance on self-reported NSW exposure, potential recall bias, small sample sizes in case-control studies resulting in wide confidence intervals, and incomplete adjustment for confounders such as alcohol intake, hormone therapy, and other lifestyle factors. Also, some cohort studies lacked detailed exposure intensity and duration data or were unable to evaluate cumulative effects over extended periods273. The heterogeneity in study designs, populations, and NSW definitions complicates direct comparisons. Genetic and sociodemographic differences may limit generalizability. Additionally, the “healthy worker effect” and other biases may attenuate observed associations in prospective designs306,311. Based on these limitations, future research should integrate detailed exposure metrics, genetic profiling, and chronotype assessments to better clarify mechanisms and identify high-risk subgroups.
Several ongoing investigations will clarify these relationships. The Italian Night-shift Work and Breast Cancer study (NCT06786949) is prospectively examining healthcare workers, integrating biospecimens for circadian-related epigenetic markers. In Canada, Improving Cancer-Related Outcomes in Shift Workers (NCT02609373) evaluated sleep-behavior interventions to reduce circadian disruption. Mechanistic studies such as the U.S. Sleep, Circadian Hormonal Dysregulation, and Breast Cancer Survival (NCT00519168) and the French Awareness About Breast Cancer Screening (NCT03777397) are linking epidemiologic findings with biological and behavioral pathways.
Collectively, current research reinforces a multifactorial relationship between NSW and BC risk. Evidence increasingly supports an elevated risk associated with persistent, intensive NSW, particularly when initiated early in life or combined with genetic susceptibility. Across the broader epidemiologic record, analysis of human cohort studies conducted between 1996 and the present shows that more than half (53%) reported a positive association between NSW and BC risk, with an apparent increase from 50% before 2019 to 58% after 2019. However, this difference was not statistically significant (χ² = 1.45, p = 0.694; Supplementary Fig. 2). Despite growing evidence, variability in exposure assessment and potential biases continue to limit causal inference, emphasizing the need for integrative molecular-epidemiologic approaches to better identify vulnerable subgroups and refine quantitative risk estimates.
Conclusions
In conclusion, the complex relationship between NSW and BC is increasingly supported by mechanistic, preclinical and clinical evidence, underscoring its relevance for occupational medicine and public health312. Disruption of circadian rhythms through exposure to LAN appears to trigger a cascade of biological effects, ranging from melatonin suppression and oxidative stress to immune dysregulation, telomere shortening, and epigenetic alterations. Such effects may contribute to BC etiopathology275. The identification of novel biomarkers, such as melatonin metabolites, oxidative catabolites, DNA methylation patterns, and circulating miRNAs, represents a critical step toward developing reliable tools for early detection and individualized risk stratification2.
From an occupational medicine perspective, these findings highlight the urgent need to better define and monitor exposure to NSW, improve workplace lighting policies, and consider individual susceptibility factors such as chronotype and genetic predisposition. Incorporating biomarker-based screening and precision risk models into occupational health protocols could enhance preventive efforts and enable timely interventions. Ultimately, integrating mechanistic insights with robust epidemiological data is essential to establish evidence-based guidelines and regulatory frameworks that effectively protect vulnerable workers and reduce the long-term burden of work-related BC.
Data availability
No datasets were generated or analysed during the current study.
References
Ward, E. M. et al. Carcinogenicity of night shift work. Lancet Oncol. 20, 1058–1059 (2019).
Briguglio, G. et al. Women’s health and night shift work: Potential targets for future strategies in breast cancer (Review). Biomed. Rep. 15, 98 (2021).
Leonardi, G. C. et al. Correlation of the risk of breast cancer and disruption of the circadian rhythm (Review). Oncol. Rep. 28, 418–428 (2012).
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca. Cancer J. Clin. 74, 229–263 (2024).
Fenga, C. Occupational exposure and risk of breast cancer. Biomed. Rep. 4, 282–292 (2016).
Burki, T. K. Night shift work and breast cancer. Lancet Oncol. 20, e352 (2019).
Pahwa, M., Labrèche, F. & Demers, P. A. Night shift work and breast cancer risk: what do the meta-analyses tell us? Scand. J. Work. Environ. Health 44, 432–435 (2018).
Obeagu, E. I. & Obeagu, G. U. Breast cancer: A review of risk factors and diagnosis. Med. (Baltim.) 103, e36905 (2024).
Lingas, E. C. A Narrative Review of the Carcinogenic Effect of Night Shift and the Potential Protective Role of Melatonin. Cureus (2023) https://doi.org/10.7759/cureus.43326.
Manna, E. D. F. et al. Hereditary Breast Cancer: Comprehensive Risk Assessment and Prevention Strategies. Genes (Basel) 16, 82 (2025).
Hansen, J. & Pedersen, J. E. Night shift work and breast cancer risk – 2023 update of epidemiologic evidence. J. Natl Cancer Cent. 5, 94–103 (2025).
Blakeman, V., Williams, J. L., Meng, Q.-J. & Streuli, C. H. Circadian clocks and breast cancer. Breast Cancer Res 18, 89 (2016).
Mieda, M. The central circadian clock of the suprachiasmatic nucleus as an ensemble of multiple oscillatory neurons. Neurosci. Res. 156, 24–31 (2020).
Arendt, J. Shift work: coping with the biological clock. Occup. Med. (Chic. Ill.). 60, 10–20 (2010).
Heyde, I. & Oster, H. Differentiating external zeitgeber impact on peripheral circadian clock resetting. Sci. Rep. 9, 20114 (2019).
Otsuki, R. et al. Decrease in Social Zeitgebers Is Associated With Worsened Delayed Sleep-Wake Phase Disorder: Findings During the Pandemic in Japan. Front. Psychiatry 13, 898600 (2022).
Garde, A. H. et al. How to schedule night shift work in order to reduce health and safety risks. Scand. J. Work. Environ. Health 46, 557–569 (2020).
Razavi, P. et al. Shift Work, Chronotype, and Melatonin Rhythm in Nurses. Cancer Epidemiol. Biomark. Prev. 28, 1177–1186 (2019).
Targhazeh, N. et al. Oncostatic activities of melatonin: Roles in cell cycle, apoptosis, and autophagy. Biochimie 202, 34–48 (2022).
Mehrzadi, S., Pourhanifeh, M. H., Mirzaei, A., Moradian, F. & Hosseinzadeh, A. An updated review of mechanistic potentials of melatonin against cancer: pivotal roles in angiogenesis, apoptosis, autophagy, endoplasmic reticulum stress and oxidative stress. Cancer Cell Int 21, 188 (2021).
Van der Merwe, M., Engelbrecht, A.-M., Africander, D., Strauss, L. & du Plessis, M. Illuminating the Tug-of-War between Estrogen and Melatonin in Estrogen Receptor Positive Breast Cancer Progression. (2023) https://doi.org/10.2139/ssrn.4525704.
Jones, R. R. Exposure to artificial light at night and risk of cancer: where do we go from here? Br. J. Cancer 124, 1467–1468 (2021).
Moroni, I. et al. Pharmacokinetics of exogenous melatonin in relation to formulation, and effects on sleep: A systematic review. Sleep. Med. Rev. 57, 101431 (2021).
Sánchez-Barceló, E. J. et al. Melatonin–estrogen interactions in breast cancer. J. Pineal Res. 38, 217–222 (2005).
Cadenas, C. et al. Loss of circadian clock gene expression is associated with tumor progression in breast cancer. Cell Cycle 13, 3282–3291 (2014).
Vivarelli, S., Spatari, G., Costa, C., Giambò, F. & Fenga, C. Computational Analyses Reveal Deregulated Clock Genes Associated with Breast Cancer Development in Night Shift Workers. Int. J. Mol. Sci. 25, 8659 (2024).
Li, S.-Y. et al. Tumor circadian clock strength influences metastatic potential and predicts patient prognosis in luminal A breast cancer. Proc. Natl. Acad. Sci. 121, e2311854121 (2024).
Chang, W.-P. & Peng, Y.-X. Meta-analysis of differences in sleep quality based on actigraphs between day and night shift workers and the moderating effect of age. J. Occup. Health 63, e12262 (2021).
Silva, I. & Costa, D. Consequences of Shift Work and Night Work: A Literature Review. Healthcare 11, 1410 (2023).
Zanif, U. et al. Melatonin supplementation and oxidative DNA damage repair capacity among night shift workers: a randomised placebo-controlled trial. Occup. Environ. Med. 82, 1–6 (2025).
Atwater, A.Q. & Castanon-Cervantes, O. Uncovering Novel Biomarkers of Inflammation as Potential Screening Targets of Disease Risk in Healthcare Shift Workers: A Pilot Study. Int. J. Nurs. Heal. Care Res. 6, 1466 (2023).
Peplonska, B. et al. Night shift work characteristics and 6-sulfatoxymelatonin (MT6s) in rotating night shift nurses and midwives. Occup. Environ. Med. 69, 339–346 (2012).
Wackers, P., Dollé, M. E. T., van Oostrom, C. T. M. & van Kerkhof, L. W. M. Exploration of genome-wide DNA methylation profiles in night shift workers. Epigenetics 18, 2152637 (2023).
Vivarelli, S. et al. Salivary Biomarkers Analysis and Neurobehavioral Assessment in Nurses Working Rotation Shifts: A Pilot Study. Int. J. Environ. Res. Public Health 20, 5376 (2023).
Garde, A. H. et al. How do different definitions of night shift affect the exposure assessment of night work? Chronobiol. Int. 33, 595–598 (2016).
Chen, Y.-M., Hsiao, T.-H., Lin, C.-H. & Fann, Y. C. Unlocking precision medicine: clinical applications of integrating health records, genetics, and immunology through artificial intelligence. J. Biomed. Sci. 32, 16 (2025).
Schrader, L. A., Ronnekleiv-Kelly, S. M., Hogenesch, J. B., Bradfield, C. A. & Malecki, K. M. C. Circadian disruption, clock genes, and metabolic health. J. Clin. Invest. 134, e170998 (2024).
Rahmati, H. et al. Basic research on circadian disruption using animal and human organoid models: a review. Biol. Rhythm Res. 56, 305–326 (2025).
Biological Implications of Circadian Disruption. (Cambridge University Press, 2023). https://doi.org/10.1017/9781009057646.
Van Dycke, K. C. G. et al. Chronically Alternating Light Cycles Increase Breast Cancer Risk in Mice. Curr. Biol. 25, 1932–1937 (2015).
Bukalev, A. V., Vinogradova, I. A., Zabezhinskii, M. A., Semenchenko, A. V. & Anisimov, V. N. Light pollution increases morbidity and mortality rate from different causes in female rats. Adv. Gerontol. 3, 180–188 (2013).
Anisimov, V. N. et al. Effect of exposure to light-at-night on life span and spontaneous carcinogenesis in female CBA mice. Int. J. Cancer 111, 475–479 (2004).
Baturin, D. A. et al. The effect of light regimen and melatonin on the development of spontaneous mammary tumors in HER-2/neu transgenic mice is related to a downregulation of HER-2/neu gene expression. Neuro Endocrinol. Lett. 22, 441–447 (2001).
Cos, S. et al. Exposure to light-at-night increases the growth of DMBA-induced mammary adenocarcinomas in rats. Cancer Lett. 235, 266–271 (2006).
Hamilton, T. Influence of environmental light and melatonin upon mammary tumour induction. J. Br. Surg. 56, 764–766 (1969).
Clemens, J. A., Welsch, C. W. & Meites, J. Effects of Hypothalamic Lesions on Incidence and Growth of Mammary Tumors in Carcinogen-Treated Rats. Exp. Biol. Med. 127, 969–972 (1968).
Kothari, L. S., Shah, P. N. & Mhatre, M. C. Effect of continuous light on the incidence of 9,10-dimethyl-1,2-benzanthracene induced mammary tumors in female Holtzman rats. Cancer Lett. 16, 313–317 (1982).
Kothari, L. S., Shah, P. N. & Mhatre, M. C. Pineal ablation in varying photoperiods and the incidence of 9,10-dimethyl-1,2-benzanthracene induced mammary cancer in rats. Cancer Lett. 22, 99–102 (1984).
Shah, P. N., Mhatre, M. C. & Kothari, L. S. Effect of melatonin on mammary carcinogenesis in intact and pinealectomized rats in varying photoperiods. Cancer Res 44, 3403–3407 (1984).
Mhatre, M. C., Shah, P. N. & Juneja, H. S. Effect of varying photoperiods on mammary morphology, DNA synthesis, and hormone profile in female rats. J. Natl Cancer Inst. 72, 1411–1416 (1984).
Subramanian, A. & Kothari, L. Suppressive effect by melatonin on different phases of 9,10-dimethyl-1,2-benzanthracene (DMBA)-induced rat mammary gland carcinogenesis. Anticancer. Drugs 2, 297–304 (1991).
Blask, D. E., Dauchy, R. T., Sauer, L. A., Krause, J. A. & Brainard, G. C. Growth and Fatty Acid Metabolism of Human Breast Cancer (MCF-7) Xenografts in Nude Rats: Impact of Constant Light-Induced Nocturnal Melatonin Suppression. Breast Cancer Res. Treat. 79, 313–320 (2003).
Blask, D. E. et al. Melatonin-Depleted Blood from Premenopausal Women Exposed to Light at Night Stimulates Growth of Human Breast Cancer Xenografts in Nude Rats. Cancer Res 65, 11174–11184 (2005).
Blask, D. E. et al. Light Exposure at Night Disrupts Host/Cancer Circadian Regulatory Dynamics: Impact on the Warburg Effect, Lipid Signaling and Tumor Growth Prevention. PLoS One 9, e102776 (2014).
Anderson, L. E., Morris, J. E., Sasser, L. B. & Stevens, R. G. Effect of constant light on DMBA mammary tumorigenesis in rats. Cancer Lett. 148, 121–126 (2000).
Lee, Y. et al. G1/S cell cycle regulators mediate effects of circadian dysregulation on tumor growth and provide targets for timed anticancer treatment. PLOS Biol. 17, e3000228 (2019).
Hadadi, E. et al. Chronic circadian disruption modulates breast cancer stemness and immune microenvironment to drive metastasis in mice. Nat. Commun. 11, 3193 (2020).
Koritala, B. S. C., Porter, K. I., Sarkar, S. & Gaddameedhi, S. Circadian disruption and cisplatin chronotherapy for mammary carcinoma. Toxicol. Appl. Pharmacol. 436, 115863 (2022).
Numata, M. et al. Metastasis of Breast Cancer Promoted by Circadian Rhythm Disruption due to Light/Dark Shift and its Prevention by Dietary Quercetin in Mice. J. Circadian Rhythms 19, 2 (2021).
Kishi, T. & Sunagawa, K. Experimental ‘jet lag’ causes sympathoexcitation via oxidative stress through AT1 receptor in the brainstem. in 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society 1969–1972 (IEEE, 2011). https://doi.org/10.1109/IEMBS.2011.6090555.
Temneanu, R. O. et al. The relevance of circadian rhythms disruption on pulmonary SOD expression in rat. Rom. J. Morphol. Embryol. 53, 789–793 (2012).
Grosbellet, E. et al. Circadian desynchronization triggers premature cellular aging in a diurnal rodent. FASEB J. 29, 4794–4803 (2015).
Zhao, B., Nepovimova, E. & Wu, Q. The role of circadian rhythm regulator PERs in oxidative stress, immunity, and cancer development. Cell Commun. Signal. 23, 30 (2025).
Gibson, M. A systematic review of the relationship between night shift work and oxidative stress. Chronobiol. Int. 39, 285–298 (2022).
Bhatti, P. et al. Oxidative DNA damage during sleep periods among nightshift workers. Occup. Environ. Med. 73, 537–544 (2016).
Bhatti, P. et al. Oxidative DNA damage during night shift work. Occup. Environ. Med. 74, 680–683 (2017).
Ishihara, I. et al. Effect of Work Conditions and Work Environments on the Formation of 8-OH-dG in Nurses and Non-Nurse Female Workers. J. UOEH 30, 293–308 (2008).
Kasai, H. et al. Life Style and Urinary 8-Hydroxydeoxyguanosine, a Marker of Oxidative DNA Damage: Effects of Exercise, Working Conditions, Meat Intake, Body Mass Index, and Smoking. Jpn. J. Cancer Res 92, 9–15 (2001).
Zou, Y. et al. Nightshift work can induce oxidative DNA damage: a pilot study. BMC Public Health 23, 891 (2023).
Manzella, N. et al. Circadian Modulation of 8-Oxoguanine DNA Damage Repair. Sci. Rep. 5, 13752 (2015).
Cheung, V., Yuen, V. M., Wong, G. T. C. & Choi, S. W. The effect of sleep deprivation and disruption on DNA damage and health of doctors. Anaesthesia 74, 434–440 (2019).
Casado, Á et al. Relationship between oxidative and occupational stress and aging in nurses of an intensive care unit. Age (Omaha) 30, 229–236 (2008).
Casado, Á et al. Determination of oxidative and occupational stress in palliative care workers. cclm 49, 471–477 (2011).
Buyukhatipoglu, H. et al. Oxidative Stress Increased in Healthcare Workers Working 24-Hour On-Call Shifts. Am. J. Med. Sci. 340, 462–467 (2010).
Ulas, T. et al. The effect of day and night shifts on oxidative stress and anxiety symptoms of the nurses. Eur. Rev. Med. Pharmacol. Sci. 16, 594–599 (2012).
Nagata, C. et al. Sleep duration, nightshift work, and the timing of meals and urinary levels of 8-isoprostane and 6-sulfatoxymelatonin in Japanese women. Chronobiol. Int. 34, 1187–1196 (2017).
Sharifian, A., Farahani, S., Pasalar, P., Gharavi, M. & Aminian, O. Shift work as an oxidative stressor. J. Circadian Rhythms 3, 15 (2005).
Shah, R. et al. Mild sleep restriction increases endothelial oxidative stress in female persons. Sci. Rep. 13, 15360 (2023).
Gromadzińska, J. et al. Relationship between intensity of night shift work and antioxidant status in blood of nurses. Int. Arch. Occup. Environ. Health 86, 923–930 (2013).
Khajehnasiri, F. et al. Oxidative Stress and Depression among Male Shift Workers in Shahid Tondgouyan Refinery. Iran. J. Psychiatry 9, 76–82 (2014).
Özdemir, P. G. et al. The influence of shift work on cognitive functions and oxidative stress. Psychiatry Res 210, 1219–1225 (2013).
Kazemi, R., Hemmatjo, R. & Mokarami, H. The effect of a blue enriched white light on salivary antioxidant capacity and melatonin among night shift workers: a field study. Ann. Occup. Environ. Med. 30, 61 (2018).
Ozyurek, P., Cevik, C., Kilic, I. & Aslan, A. Effects of Day and Night Shifts on Stress, Anxiety, Quality of Life, and Oxidative Stress Parameters in Nurses. Florence Nightingale J. Nurs. 29, 81–92 (2021).
Boeri, L. et al. Oxidative Stress and Semen Quality Among Night- and Day-Shift Workers: A Cross-Sectional Study. Antioxidants 14, 802 (2025).
Teixeira, K. R. C. et al. Night workers have lower levels of antioxidant defenses and higher levels of oxidative stress damage when compared to day workers. Sci. Rep. 9, 4455 (2019).
Makris, K. C., Heibati, B. & Narui, S. Z. Chrono-modulated effects of external stressors on oxidative stress and damage in humans: A scoping review on night shift work. Environ. Int. 178, 108048 (2023).
Sletten, T. L. et al. Health consequences of circadian disruption. Sleep 43, zsz194 (2020).
Logan, R. W. et al. Chronic Shift-Lag Alters the Circadian Clock of NK Cells and Promotes Lung Cancer Growth in Rats. J. Immunol. 188, 2583–2591 (2012).
Li, J. C. & Xu, F. Influences of Light-Dark Shifting on the Immune System, Tumor Growth and Life Span of Rats, Mice and Fruit Flies as well as on the Counteraction of Melatonin. Neurosignals 6, 77–89 (1997).
Valdés-Tovar, M., Escobar, C., Solís-Chagoyán, H., Asai, M. & Benítez-King, G. Constant light suppresses production of Met-enkephalin-containing peptides in cultured splenic macrophages and impairs primary immune response in rats. Chronobiol. Int. 32, 164–177 (2015).
Deprés-Brummer, P., Bourin, P., Pages, N., Metzger, G. & Lévi, F. Persistent T lymphocyte rhythms despite suppressed circadian clock outputs in rats. Am. J. Physiol. 273, R1891–R1899 (1997).
Mikolajczak, P., Wiktorowicz, K., Okulicz-Kozaryn, I., Kostrzewa, A. & Kaminska, E. Analysis of the distribution of peripheral blood lymphocyte subsets associated with chronic ethanol treatment in rats with a disturbed circadian cycle. Drug Alcohol Depend. 60, 303–309 (2000).
Fonken, L. K., Weil, Z. M. & Nelson, R. J. Mice exposed to dim light at night exaggerate inflammatory responses to lipopolysaccharide. Brain. Behav. Immun. 34, 159–163 (2013).
Walker, W. H., Meléndez-Fernández, O. H. & Nelson, R. J. Prior exposure to dim light at night impairs dermal wound healing in female C57BL/6 mice. Arch. Dermatol. Res. 311, 573–576 (2019).
Cable, E. J., Onishi, K. G. & Prendergast, B. J. Circadian rhythms accelerate wound healing in female Siberian hamsters. Physiol. Behav. 171, 165–174 (2017).
Prendergast, B. J. et al. Circadian Disruption Alters the Effects of Lipopolysaccharide Treatment on Circadian and Ultradian Locomotor Activity and Body Temperature Rhythms of Female Siberian Hamsters. J. Biol. Rhythms 30, 543–556 (2015).
Adams, K. L., Castanon-Cervantes, O., Evans, J. A. & Davidson, A. J. Environmental Circadian Disruption Elevates the IL-6 Response to Lipopolysaccharide in Blood. J. Biol. Rhythms 28, 272–277 (2013).
Phillips, D. J., Savenkova, M. I. & Karatsoreos, I. N. Environmental disruption of the circadian clock leads to altered sleep and immune responses in mouse. Brain. Behav. Immun. 47, 14–23 (2015).
Zeng, X., Liang, C. & Yao, J. Chronic shift-lag promotes NK cell ageing and impairs immunosurveillance in mice by decreasing the expression of CD122. J. Cell. Mol. Med. 24, 14583–14595 (2020).
Zhang, Z. et al. Circadian clock: a regulator of the immunity in cancer. Cell Commun. Signal. 19, 37 (2021).
Zeng, Y., Guo, Z., Wu, M., Chen, F. & Chen, L. Circadian rhythm regulates the function of immune cells and participates in the development of tumors. Cell Death Discov. 10, 199 (2024).
Yan, Y. et al. Circadian rhythms and breast cancer: unraveling the biological clock’s role in tumor microenvironment and ageing. Front. Immunol. 15, 1444426 (2024).
Buss, M. R., Wirth, M. D. & Burch, J. B. Association of shiftwork and leukocytes among national health and nutrition examination survey respondents. Chronobiol. Int. 35, 435–439 (2018).
Okamoto, H. et al. An Occupational Health Study of Emergency Physicians in Japan: Health Assessment by Immune Variables (CD4, CD8, CD56, and NK Cell Activity) at the Beginning of Work. J. Occup. Health 50, 136–146 (2008).
van Mark, A. et al. The impact of shift work induced chronic circadian disruption on IL-6 and TNF-α immune responses. J. Occup. Med. Toxicol. 5, 18 (2010).
Copertaro, A. et al. Influence of Shift-work on Selected Immune Variables in Nurses. Ind. Health 49, 597–604 (2011).
Loef, B. et al. Immunological effects of shift work in healthcare workers. Sci. Rep. 9, 18220 (2019).
Cermakian, N., Nobis, C. C. & Labrecque, N. Circadian control of antigen-specific T cell responses. ChronoPhysiology Ther. ume 6, 65–74 (2016).
Bollinger, T. et al. Sleep-dependent activity of T cells and regulatory T cells. Clin. Exp. Immunol. 155, 231–238 (2009).
Dimitrov, S. et al. Gαs-coupled receptor signaling and sleep regulate integrin activation of human antigen-specific T cells. J. Exp. Med. 216, 517–526 (2019).
Kos, K. & de Visser, K. E. The Multifaceted Role of Regulatory T Cells in Breast Cancer. Annu. Rev. Cancer Biol. 5, 291–310 (2021).
Streng, A. A. et al. Night shift work characteristics are associated with several elevated metabolic risk factors and immune cell counts in a cross-sectional study. Sci. Rep. 12, 2022 (2022).
Harding, B. N. et al. Disruption of cellular immune response among male rotating night shift workers in Spain– The HORMONIT study. Front. Immunol. 13, 776917 (2022).
Nagai, M. et al. Effects of Fatigue on Immune Function in Nurses Performing Shift Work. J. Occup. Health 53, 312–319 (2011).
N’da Marcelin, H. et al. Circulating natural killer cells and their association with breast cancer and its clinico-pathological characteristics. Ecancermedicalscience 17, 1567 (2023).
Razeghian, E. et al. The role of the natural killer (NK) cell modulation in breast cancer incidence and progress. Mol. Biol. Rep. 49, 10935–10948 (2022).
Ruiz, F. S. et al. Night shift work and immune response to the meningococcal conjugate vaccine in healthy workers: a proof of concept study. Sleep. Med 75, 263–275 (2020).
Coppeta, L. et al. Night Shift Work Is Associated with Reduced Rate of Humoral Response Following Vaccination for HBV. Int. J. Environ. Res. Public Health 19, 8834 (2022).
Faraut, B. et al. Immune disruptions and night shift work in hospital healthcare professionals: The intricate effects of social jet-lag and sleep debt. Front. Immunol. 13, 939829 (2022).
Papantoniou, K. et al. O-205 Night shift work and sleep deprivation in relation to vaccine induced SARS-CoV-2 antibody responses in a general population cohort (COVICAT study). in Abstracts A67.1-A67 (BMJ Publishing Group Ltd, 2023). https://doi.org/10.1136/OEM-2023-EPICOH.164.
Brouwers, T. M. J. et al. The effect of sleep and shift work on the primary immune response to messenger RNA-based COVID-19 vaccination. J. Sleep Res. https://doi.org/10.1111/jsr.14431 (2024).
Loef, B. et al. Night-shift work is associated with increased susceptibility to SARS-CoV-2 infection. Chronobiol. Int. 39, 1100–1109 (2022).
Hartveit et al. Night work and sleep debt are associated with infections among Norwegian nurses. Chronobiol. Int. 42, 309–318 (2025).
Hasanlı, Y. S. Assessment of inflammatory status in long-term night shift workers using the CRP-albumin ratio and neutrophil-lymphocyte ratio. Arch. Environ. Occup. Health 80, 17–21 (2025).
Preuss, F. et al. Adverse effects of chronic circadian desynchronization in animals in a “challenging” environment. Am. J. Physiol. Integr. Comp. Physiol. 295, R2034–R2040 (2008).
Castanon-Cervantes, O. et al. Dysregulation of Inflammatory Responses by Chronic Circadian Disruption. J. Immunol. 185, 5796–5805 (2010).
Brager, A. J. et al. Sleep Loss and the Inflammatory Response in Mice Under Chronic Environmental Circadian Disruption. PLoS One 8, e63752 (2013).
Chen, J. et al. IL-6: The Link Between Inflammation, Immunity and Breast Cancer. Front. Oncol. 12, 903800 (2022).
Summa, K. C. et al. Disruption of the Circadian Clock in Mice Increases Intestinal Permeability and Promotes Alcohol-Induced Hepatic Pathology and Inflammation. PLoS One 8, e67102 (2013).
Hand, L. E. et al. The circadian clock regulates inflammatory arthritis. FASEB J. 30, 3759–3770 (2016).
Wu, T. et al. Facilitated physiological adaptation to prolonged circadian disruption through dietary supplementation with essence of chicken. Chronobiol. Int. 32, 1458–1468 (2015).
Polidarová, L., Houdek, P. & Sumová, A. Chronic disruptions of circadian sleep regulation induce specific proinflammatory responses in the rat colon. Chronobiol. Int. 34, 1273–1287 (2017).
Guerrero-Vargas, N. N. et al. Circadian disruption promotes tumor growth by anabolic host metabolism; experimental evidence in a rat model. BMC Cancer 17, 625 (2017).
Khalyfa, A. et al. Exosomes and Metabolic Function in Mice Exposed to Alternating Dark-Light Cycles Mimicking Night Shift Work Schedules. Front. Physiol. 8, 882 (2017).
O’Siorain, J. R. et al. Time-of-day control of mitochondria regulates NLRP3 inflammasome activation in macrophages. FASEB J. 38, e70235 (2024).
Jerigova, V., Zeman, M. & Okuliarova, M. Circadian Disruption and Consequences on Innate Immunity and Inflammatory Response. Int. J. Mol. Sci. 23, 13722 (2022).
Fatima, N., Sonkar, G. K. & Singh, S. Circadian mechanism disruption is associated with dysregulation of inflammatory and immune responses: a systematic review. Beni-Suef Univ. J. Basic Appl. Sci. 11, 107 (2022).
Hong, J. et al. The relationship between night shift work and breast cancer incidence: A systematic review and meta-analysis of observational studies. Open Med 17, 712–731 (2022).
Nishitani, N. & Sakakibara, H. Subjective Poor Sleep and White Blood Cell Count in Male Japanese Workers. Ind. Health 45, 296–300 (2007).
Sookoian, S. et al. Effects of rotating shift work on biomarkers of metabolic syndrome and inflammation. J. Intern. Med. 261, 285–292 (2007).
Puttonen, S., Viitasalo, K. & Härmä, M. Effect of Shiftwork on Systemic Markers of Inflammation. Chronobiol. Int. 28, 528–535 (2011).
Kim, S.-W. et al. Night shift work and inflammatory markers in male workers aged 20–39 in a display manufacturing company. Ann. Occup. Environ. Med. 28, 48 (2016).
Swanson, G. R. et al. Night workers with circadian misalignment are susceptible to alcohol-induced intestinal hyperpermeability with social drinking. Am. J. Physiol. Liver Physiol. 311, G192–G201 (2016).
Pavanello, S. et al. Inflammatory Long Pentraxin 3 is Associated with Leukocyte Telomere Length in Night-Shift Workers. Front. Immunol. 8, 516 (2017).
Khosro, S., Alireza, S., Omid, A. & Forough, S. Night work and inflammatory markers. Indian J. Occup. Environ. Med. 15, 38 (2011).
Nukiwa, R. et al. Changes in gene expression in healthcare workers during night shifts: implications for immune response and health risks. J. Intensive Care 13, 14 (2025).
Kanki, M. et al. Poor sleep and shift work associate with increased blood pressure and inflammation in UK Biobank participants. Nat. Commun. 14, 7096 (2023).
Amano, H., Fukuda, Y., Yokoo, T. & Yamaoka, K. Interleukin-6 Level among Shift and Night Workers in Japan: Cross-Sectional Analysis of the J-HOPE Study. J. Atheroscler. Thromb. 25, 1206–1214 (2018).
Reinhardt, ÉL., Fernandes, P. A. C. M., Markus, R. P. & Fischer, F. M. Night work effects on salivary cytokines TNF, IL-1β and IL-6. Chronobiol. Int. 36, 11–26 (2019).
Christensen, J. O. et al. Shift work, low-grade inflammation, and chronic pain: a 7-year prospective study. Int. Arch. Occup. Environ. Health 94, 1013–1022 (2021).
Woo, S.-J., Chae, C.-H. & Lim, J.-W. Association between shift work and inflammatory markers in workers at an electronics manufacturing company. Ann. Occup. Environ. Med. 34, e35 (2022).
Bahinipati, J. et al. Estimation of Pro-Inflammatory Markers In Night Shift Healthcare Workers And Identify Risk Factors Associated With It. Asia Pacific J. Heal. Manag. https://doi.org/10.24083/apjhm.v19i1.2599 (2024).
Bizzarri, D. et al. a Biomarker of Low-Grade Inflammation, Is Increased in Male Night Shift Workers. Metabolites 12, 1172 (2022).
Yao, Y. & Ma, J. Night shift work increases the risk of irritable bowel syndrome, which is mediated by inflammation. Eur. J. Public Health 34, ckae144.983 (2024).
Yao, Y. et al. Associations of Long-Term Night Shift Work With Incident Irritable Bowel Syndrome: A Population-Based Cohort Study. J. Gastroenterol. Hepatol. 40, 2231–2239 (2025).
Caldarola, G. et al. Evaluation of the Impact of Night Shift Work on Disease Severity in Psoriatic Patients: A Case-Control Study with Clinical, Hormonal, and Immunological Evaluation. Dermatology 240, 665–670 (2024).
Giudice, A. et al. The Effect of Light Exposure at Night (LAN) on Carcinogenesis via Decreased Nocturnal Melatonin Synthesis. Molecules 23, 1308 (2018).
Jin, Y., Choi, Y. J., Heo, K. & Park, S. J. Melatonin as an Oncostatic Molecule Based on Its Anti-Aromatase Role in Breast Cancer. Int. J. Mol. Sci. 22, 438 (2021).
Pardi, P. C. et al. Biological action of melatonin on target receptors in breast cancer. Rev. Assoc. Med. Bras. 70, e20231260 (2024).
Li, Y. et al. Melatonin for the prevention and treatment of cancer. Oncotarget 8, 39896–39921 (2017).
Karadas, A. K., Dilmac, S., Aytac, G. & Tanriover, G. Melatonin decreases metastasis, primary tumor growth and angiogenesis in a mice model of breast cancer. Hum. Exp. Toxicol. 40, 1545–1557 (2021).
Dauchy, R. T. et al. Circadian and Melatonin Disruption by Exposure to Light at Night Drives Intrinsic Resistance to Tamoxifen Therapy in Breast Cancer. Cancer Res 74, 4099–4110 (2014).
Travlos, G. S., Wilson, R. E., Murrell, J. A., Chignell, C. F. & Boorman, G. A. The Effect of Short Intermittent Light Exposures on the Melatonin Circadian Rhythm and NMU-Induced Breast Cancer in Female F344/N Rats. Toxicol. Pathol. 29, 126–136 (2001).
Jardim-Perassi, B. V. et al. Effect of Melatonin on Tumor Growth and Angiogenesis in Xenograft Model of Breast Cancer. PLoS One 9, e85311 (2014).
Oshiba, R. T., Touson, E., Elsherbini, Y. M. & Abdraboh, M. E. Melatonin: A regulator of the interplay between FoxO1, miR96, and miR215 signaling to diminish the growth, survival, and metastasis of murine adenocarcinoma. BioFactors 47, 740–753 (2021).
Odeh, L. H., Talib, W. H. & Basheti, I. A. Synergistic effect of thymoquinone and melatonin against breast cancer implanted in mice. J. Cancer Res. Ther. 14, S324–S330 (2018).
Garcia, C. P. et al. Synergistic anti-tumor effects of melatonin and PUFAs from walnuts in a murine mammary adenocarcinoma model. Nutrition 31, 570–577 (2015).
Talib, W. H. A ketogenic diet combined with melatonin overcomes cisplatin and vincristine drug resistance in breast carcinoma syngraft. Nutrition 72, 110659 (2020).
Panchenko, A. V. et al. Melatonin Administered before or after a Cytotoxic Drug Increases Mammary Cancer Stabilization Rates in HER2/Neu Mice. Chemotherapy 65, 42–50 (2020).
Grant, S. G., Melan, M. A., Latimer, J. J. & Witt-Enderby, P. A. Melatonin and breast cancer: cellular mechanisms, clinical studies and future perspectives. Expert Rev. Mol. Med. 11, e5 (2009).
Hunter, C. M. & Figueiro, M. G. Measuring Light at Night and Melatonin Levels in Shift Workers: A Review of the Literature. Biol. Res. Nurs. 19, 365–374 (2017).
Barnes, R., Deacon, S., Forbes, M. & Arendt, J. Adaptation of the 6-sulphatoxymelatonin rhythm in shiftworkers on offshore oil installations during a 2-week 12-h night shift. Neurosci. Lett. 241, 9–12 (1998).
Barnes, R., Forbes, M. & Arendt, J. Shift type and season affect adaptation of the 6-sulphatoxymelatonin rhythm in offshore oil rig workers. Neurosci. Lett. 252, 179–182 (1998).
Dumont, M., Lanctôt, V., Cadieux-Viau, R. & Paquet, J. Melatonin Production and Light Exposure of Rotating Night Workers. Chronobiol. Int. 29, 203–210 (2012).
Luz, C. S. S. et al. Dietary Intake and Body Composition of Fixed-Shift Workers During the Climacteric: An Intervention Study with Exogenous Melatonin. Obesities 5, 7 (2025).
Schernhammer, E. S., Kroenke, C. H., Dowsett, M., Folkerd, E. & Hankinson, S. E. Urinary 6-sulfatoxymelatonin levels and their correlations with lifestyle factors and steroid hormone levels. J. Pineal Res. 40, 116–124 (2006).
Burch, J. B., Yost, M. G., Johnson, W. & Allen, E. Melatonin, Sleep, and Shift Work Adaptation. J. Occup. Environ. Med. 47, 893–901 (2005).
Marie Hansen, Å, Helene Garde, A. & Hansen, J. Diurnal Urinary 6-Sulfatoxymelatonin Levels among Healthy Danish Nurses during Work and Leisure Time. Chronobiol. Int. 23, 1203–1215 (2006).
Grundy, A. et al. Light intensity exposure, sleep duration, physical activity, and biomarkers of melatonin among rotating shift nurses. Chronobiol. Int. 26, 1443–1461 (2009).
Bracci, M. et al. Rotating-shift nurses after a day off: peripheral clock gene expression, urinary melatonin, and serum 17-β-estradiol levels. Scand. J. Work. Environ. Health 40, 295–304 (2014).
Mirick, D. K. et al. Night Shift Work and Levels of 6-Sulfatoxymelatonin and Cortisol in Men. Cancer Epidemiol. Biomark. Prev. 22, 1079–1087 (2013).
Papantoniou, K. et al. Circadian Variation of Melatonin, Light Exposure, and Diurnal Preference in Day and Night Shift Workers of Both Sexes. Cancer Epidemiol. Biomark. Prev. 23, 1176–1186 (2014).
Dumont, M. & Paquet, J. Progressive decrease of melatonin production over consecutive days of simulated night work. Chronobiol. Int. 31, 1231–1238 (2014).
Vieira, R. P. O. et al. High social jetlag is correlated with nocturnal inhibition of melatonin production among night workers. Chronobiol. Int. 38, 1170–1176 (2021).
Wang, T., Shao, R. & Hao, L. Effects of Different Nocturnal Lighting Stimuli on Melatonin, Sleep and Cognitive Performance of Workers in Confined Spaces. Buildings 13, 2112 (2023).
Jensen, M. A., Hansen, ÅM., Kristiansen, J., Nabe-Nielsen, K. & Garde, A. H. Changes in the diurnal rhythms of cortisol, melatonin, and testosterone after 2, 4, and 7 consecutive night shifts in male police officers. Chronobiol. Int. 33, 1280–1292 (2016).
Leung, M. et al. Shift Work, Chronotype, and Melatonin Patterns among Female Hospital Employees on Day and Night Shifts. Cancer Epidemiol. Biomark. Prev. 25, 830–838 (2016).
Fustinoni, S. et al. Steroid hormones, vitamin D and melatonin in rapidly rotating shift female hospital workers. Toxicol. Lett. 403, 32–39 (2025).
Khanjani, S., Shamabadi, A., Akhondzadeh, S. & Malekirad, A. A. Melatonin for Sleep Quality and Occupational Cognitive Performance in Shift Workers with Low Sleep Quality: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. J. Clin. Pharm. Ther. 2024, (2024).
Söylemez, S., Çaycı Sivri, A. B., Şimşek, E., Polat, B. & Çakır, B. Melatonin, leptin, and ghrelin levels in nurses working night shifts. J. Surg. Med. https://doi.org/10.28982/josam.443902 (2018).
Cho, C.-H. & Lee, Y. The Chronobiologic-Based Practical Approach to Shift Work. Chronobiol. Med. 1, 103–106 (2019).
Xue, P., Nôga, D. A. & Benedict, C. Melatonin: is it really a cardiovascular wonder pill for shift workers? Lancet Diabetes Endocrinol. 12, 370–371 (2024).
Daugaard, S. et al. Night work, light exposure and melatonin on work days and days off. Chronobiol. Int. 34, 942–955 (2017).
Hohor, S. et al. Impaired Melatonin Secretion, Oxidative Stress and Metabolic Syndrome in Night Shift Work. Antioxidants 12, 959 (2023).
Pham, T.-T. et al. Night-shift work, circadian and melatonin pathway related genes and their interaction on breast cancer risk: evidence from a case-control study in Korean women. Sci. Rep. 9, 10982 (2019).
Ritonja, J. A. et al. Investigating the relationship between melatonin patterns and methylation in circadian genes among day shift and night shift workers. Occup. Environ. Med. 79, 673–680 (2022).
He, L., Sui, X., Xiao, Y., Ji, P. & Gong, Y. Circadian Rhythm Disruption in Triple-Negative Breast Cancer: Molecular Insights and Treatment Strategies. J. Pineal Res. 77, (2025).
Wu, H.-S., Gao, F., Yan, L. & Given, C. Evaluating chronotypically tailored light therapy for breast cancer survivors: Preliminary findings on fatigue and disrupted sleep. Chronobiol. Int. 39, 221–232 (2022).
Ortega-Campos, S. M., Verdugo-Sivianes, E. M., Amiama-Roig, A., Blanco, J. R. & Carnero, A. Interactions of circadian clock genes with the hallmarks of cancer. Biochim. Biophys. Acta - Rev. Cancer 1878, 188900 (2023).
Lee, Y. Roles of circadian clocks in cancer pathogenesis and treatment. Exp. Mol. Med. 53, 1529–1538 (2021).
Herrero, L. et al. Altered Circadian Rhythm and Metabolic Gene Profile in Rats Subjected to Advanced Light Phase Shifts. PLoS One 10, e0122570 (2015).
Kim, S.-M. et al. Shift work cycle-induced alterations of circadian rhythms potentiate the effects of high-fat diet on inflammation and metabolism. FASEB J. 32, 3085–3095 (2018).
Papagiannakopoulos, T. et al. Circadian Rhythm Disruption Promotes Lung Tumorigenesis. Cell Metab. 24, 324–331 (2016).
Li, X., Hu, Y. & Aslanbeigi, F. Genetic and epigenetic alterations in night shift nurses with breast cancer: a narrative review. Cancer Cell Int 25, 20 (2025).
Reszka, E. et al. Circadian gene expression in peripheral blood leukocytes of rotating night shift nurses. Scand. J. Work. Environ. Health 39, 187–194 (2013).
Bracci, M. et al. Influence of night-shift and napping at work on urinary melatonin, 17-β-estradiol and clock gene expression in pre-menopausal nurses. J. Biol. Regul. Homeost. Agents 27, 267–274 (2013).
Fang, M. Z. et al. Sleep interruption associated with house staff work schedules alters circadian gene expression. Sleep. Med 16, 1388–1394 (2015).
Kervezee, L., Cuesta, M., Cermakian, N. & Boivin, D. B. Simulated night shift work induces circadian misalignment of the human peripheral blood mononuclear cell transcriptome. Proc. Natl Acad. Sci. 115, 5540–5545 (2018).
Hattammaru, M. et al. The effect of night shift work on the expression of clock genes in beard hair follicle cells. Sleep. Med 56, 164–170 (2019).
Toffoli, B. et al. Preliminary Study on the Effect of a Night Shift on Blood Pressure and Clock Gene Expression. Int. J. Mol. Sci. 24, 9309 (2023).
Rizza, S. et al. Impact of light therapy on rotating night shift workers: the EuRhythDia study. Acta Diabetol. 59, 1589–1596 (2022).
Yang, Z. et al. Disruption of central and peripheral circadian clocks and circadian controlled estrogen receptor rhythms in night shift nurses in working environments. FASEB J. 38, (2024).
Samulin Erdem, J. et al. Mechanisms of Breast Cancer in Shift Workers: DNA Methylation in Five Core Circadian Genes in Nurses Working Night Shifts. J. Cancer 8, 2876–2884 (2017).
Bhatti, P. et al. Nightshift work and genome-wide DNA methylation. Chronobiol. Int. 32, 103–112 (2015).
Ritonja, J. A. et al. Exploring the impact of night shift work on methylation of circadian genes. Epigenetics 17, 1259–1268 (2022).
Zhu, Y. et al. Epigenetic Impact of Long-Term Shiftwork: Pilot Evidence From Circadian Genes and Whole-Genome Methylation Analysis. Chronobiol. Int. 28, 852–861 (2011).
Li, Q. et al. Association of rotating night shift work, CLOCK, MTNR1A, MTNR1B genes polymorphisms and their interactions with type 2 diabetes among steelworkers: a case–control study. BMC Genomics 24, 232 (2023).
Min, Q. et al. The correlation of shift work and CLOCK, BMAL1, and PER1 gene polymorphisms with hypertension in healthcare workers: A cross-sectional study. Med. (Baltim.) 103, e40148 (2024).
Fores-Martos, J. et al. Circadian PERformance in breast cancer: a germline and somatic genetic study of PER3VNTR polymorphisms and gene co-expression. npj Breast Cancer 7, 118 (2021).
Cox, K. H. & Takahashi, J. S. Circadian clock genes and the transcriptional architecture of the clock mechanism. J. Mol. Endocrinol. 63, R93–R102 (2019).
Kochan, D. Z. et al. Circadian disruption-induced microRNAome deregulation in rat mammary gland tissues. Oncoscience 2, 428–442 (2015).
Xiang, S. et al. Epigenetic inhibition of the tumor suppressor ARHI by light at night-induced circadian melatonin disruption mediates STAT3-driven paclitaxel resistance in breast cancer. J. Pineal Res. 67, (2019).
Grygoryev, D. et al. Rapid Response and Slow Recovery of the H3K4me3 Epigenomic Marker in the Liver after Light-mediated Phase Advances of the Circadian Clock. J. Biol. Rhythms 33, 363–375 (2018).
Mendoza-Viveros, L. et al. miR-132/212 Modulates Seasonal Adaptation and Dendritic Morphology of the Central Circadian Clock. Cell Rep. 19, 505–520 (2017).
Borck, P. C. et al. Nighttime light exposure enhances Rev-erbα-targeting microRNAs and contributes to hepatic steatosis. Metabolism 85, 250–258 (2018).
Bollati, V. et al. Epigenetic effects of shiftwork on blood DNA methylation. Chronobiol. Int. 27, 1093–1104 (2010).
Carugno, M. et al. Night Shift Work, DNA Methylation and Telomere Length: An Investigation on Hospital Female Nurses. Int. J. Environ. Res. Public Health 16, 2292 (2019).
Shi, F. et al. Aberrant DNA methylation of miR-219 promoter in long-term night shiftworkers. Environ. Mol. Mutagen. 54, 406–413 (2013).
Jacobs, D. I. et al. Methylation alterations at imprinted genes detected among long-term shiftworkers. Environ. Mol. Mutagen. 54, 141–146 (2013).
Peplonska, B. et al. Rotating night work, lifestyle factors, obesity and promoter methylation in BRCA1 and BRCA2 genes among nurses and midwives. PLoS One 12, e0178792 (2017).
White, A. J., Kresovich, J. K., Xu, Z., Sandler, D. P. & Taylor, J. A. Shift work, DNA methylation and epigenetic age. Int. J. Epidemiol. 48, 1536–1544 (2019).
Liu, R. et al. Aberrant methylation of miR-34b is associated with long-term shiftwork: a potential mechanism for increased breast cancer susceptibility. Cancer Causes Control 26, 171–178 (2015).
Li, D.-D., Zhou, T., Gao, J., Wu, G.-L. & Yang, G.-R. Circadian rhythms and breast cancer: from molecular level to therapeutic advancements. J. Cancer Res. Clin. Oncol. 150, 419 (2024).
Ferrari, L. et al. Association between night shift work and methylation of a subset of immune-related genes. Front. Public Heal. 10, (2023).
Lahtinen, A. et al. Differential DNA methylation in recovery from shift work disorder. Sci. Rep. 11, 2895 (2021).
Sasmita, D. M. A., Permana, K. G., Aryandono, T., Heriyanto, D. S. & Anwar, S. L. Shorter telomere length as a prognostic marker for survival and recurrence in breast cancer: a systematic review and meta-analysis. Explor. Target. Anti-tumor Ther. 6, (2025).
Parks, C. G. et al. Employment and work schedule are related to telomere length in women. Occup. Environ. Med. 68, 582–589 (2011).
Liang, G. et al. Associations between Rotating Night Shifts, Sleep Duration, and Telomere Length in Women. PLoS One 6, e23462 (2011).
Samulin Erdem, J. et al. Mechanisms of breast cancer risk in shift workers: association of telomere shortening with the duration and intensity of night work. Cancer Med 6, 1988–1997 (2017).
Autio, I. et al. Sleep disturbances, shift work, and epigenetic ageing in working-age adults: findings from the Young Finns study. Clin. Epigenetics 17, 55 (2025).
Ferrari, L. et al. Impact of night shift work on telomere length and epigenetic age in older workers. J. Occup. Med. Toxicol. 20, 31 (2025).
Lehnert, M. et al. Vitamin D supply in shift working nurses. Chronobiol. Int. 35, 724–729 (2018).
ITOH, H. et al. Association between Night-shift Work and Serum 25-hydroxyvitamin D Levels in Japanese Male Indoor Workers: A Cross-sectional Study. Ind. Health 49, 658–662 (2011).
Rizza, S. et al. Monthly fluctuations in 25-hydroxy-vitamin D levels in day and rotating night shift hospital workers. J. Endocrinol. Invest. 43, 1655–1660 (2020).
Kohl, I. S. et al. Association Between Shift Work and Vitamin D Levels in Brazilian Female Workers. Nutrients 17, 1201 (2025).
Yang, Z.-Y. et al. Exploring the Relationship between Serum Vitamin D and Shift Work. J. Med. Sci. 41, 179–185 (2021).
Alefishat, E. & Abu Farha, R. Determinants of vitamin D status among Jordanian employees: Focus on the night shift effect. Int. J. Occup. Med. Environ. Health 29, 859–870 (2016).
Park, H., Suh, B. & Lee, S.-J. Shift work and depressive symptoms: the mediating effect of vitamin D and sleep quality. Chronobiol. Int. 36, 689–697 (2019).
de Menezes Júnior, L. A. A. et al. Rotating shift workers with vitamin D deficiency have a higher risk of obstructive sleep apnea. Sleep. Breath. 27, 727–735 (2023).
Romano, A. et al. Shift work and serum 25-OH vitamin D status among factory workers in Northern Italy: Cross-sectional study. Chronobiol. Int. 32, 842–847 (2015).
Lee, C. Y., Moawad, K. & Pien, G. W. Impact of night shift work on women’s fertility, pregnancy and menopause. Front. Sleep 4, (2025).
Schernhammer, E. S. et al. Epidemiology of urinary melatonin in women and its relation to other hormones and night work. Cancer Epidemiol. Biomark. Prev. 13, 936–943 (2004).
Nagata, C. et al. Light Exposure at Night, Urinary 6-Sulfatoxymelatonin, and Serum Estrogens and Androgens in Postmenopausal Japanese Women. Cancer Epidemiol. Biomark. Prev. 17, 1418–1423 (2008).
Langley, A. R. et al. A cross-sectional study of breast cancer biomarkers among shift working nurses. BMJ Open 2, e000532 (2012).
Davis, S., Mirick, D. K., Chen, C. & Stanczyk, F. Z. Night Shift Work and Hormone Levels in Women. Cancer Epidemiol. Biomark. Prev. 21, 609–618 (2012).
Gómez-Acebo, I. et al. Association between exposure to rotating night shift versus day shift using levels of 6-sulfatoxymelatonin and cortisol and other sex hormones in women. Chronobiol. Int. 32, 128–135 (2015).
Papantoniou, K. et al. Increased and Mistimed Sex Hormone Production in Night Shift Workers. Cancer Epidemiol. Biomark. Prev. 24, 854–863 (2015).
Peplonska, B., Bukowska, A., Lie, J. A., Gromadzinska, J. & Zienolddiny, S. Night shift work and other determinants of estradiol, testosterone, and dehydroepiandrosterone sulfate among middle-aged nurses and midwives. Scand. J. Work. Environ. Health 42, 435–446 (2016).
Cakan, P. & Yildiz, S. Effects of Half- or Whole-Night Shifts on Physiological and Cognitive Parameters in Women. Am. J. Med. Sci. 360, 525–536 (2020).
Vivarelli, S., Marconi, A., Matera, S., Falzone, L. & Fenga, C. Night Shift Work, Circadian Disruption, and Gut Microbiome: Implications for Human Health. Crit. Rev. Oncog. https://doi.org/10.1615/CritRevOncog.2025059579 (2025).
Jiang, X. et al. Identifying Women at High Risk for Breast Cancer Using Data From the Electronic Health Record Compared With Self-Report. JCO Clin. Cancer Informatics 1–8 https://doi.org/10.1200/CCI.18.00072 (2019).
Bjorvatn, B. et al. The Association Between Shift Work and Immunological Biomarkers in Nurses. Front. Public Heal. 8, (2020).
Briguglio, G. et al. Salivary Biomarkers and Work-Related Stress in Night Shift Workers. Int. J. Environ. Res. Public Health 18, 3184 (2021).
Akour, A., Farha, R. A., Alefishat, E., Kasabri, V. & Bulatova, N. Insulin resistance and levels of cardiovascular biomarkers in night-shift workers. Atherosclerosis 315, e117–e118 (2020).
Van Dycke, K. C. G. et al. Biomarkers for Circadian Rhythm Disruption Independent of Time of Day. PLoS One 10, e0127075 (2015).
Sambiagio, N. et al. Rapid Liquid Chromatography—Tandem Mass Spectrometry Analysis of Two Urinary Oxidative Stress Biomarkers: 8-oxodG and 8-isoprostane. Antioxidants 10, 38 (2020).
Caumo, W. et al. Melatonin is a biomarker of circadian dysregulation and is correlated with major depression and fibromyalgia symptom severity. J. Pain. Res. ume 12, 545–556 (2019).
Mirick, D. K. & Davis, S. Melatonin as a Biomarker of Circadian Dysregulation. Cancer Epidemiol. Biomark. Prev. 17, 3306–3313 (2008).
Liu, J. et al. MT 1 and MT 2 Melatonin Receptors: A Therapeutic Perspective. Annu. Rev. Pharmacol. Toxicol. 56, 361–383 (2016).
Morgan, M. N. et al. The Cancer Clock Is (Not) Ticking: Links between Circadian Rhythms and Cancer. Clocks Sleep. 1, 435–458 (2019).
Mortaş, H., Bilici, S. & Karakan, T. The circadian disruption of night work alters gut microbiota consistent with elevated risk for future metabolic and gastrointestinal pathology. Chronobiol. Int. 37, 1067–1081 (2020).
Martelli, M., Salvio, G., Santarelli, L. & Bracci, M. Shift Work and Serum Vitamin D Levels: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 19, 8919 (2022).
van der Grinten, T. et al. Detailed assessment of night shift work aspects and potential mediators of its health effects: the contribution of field studies. Front. Public Heal. 13, (2025).
Münch, M. & Kramer, A. Timing matters: New tools for personalized chronomedicine and circadian health. Acta Physiol. 227, (2019).
McConway, K. Cancer and night shift work: what we still do not know and why. Lancet Oncol. 20, 1051–1052 (2019).
National Toxicology Program Cancer Hazard Assessment Report on Night Shift Work and Light at Night. https://doi.org/10.22427/NTP-CHR-NSWLAN.
Erren, T. C., Morfeld, P., Groß, J. V., Wild, U. & Lewis, P. IARC 2019: “Night shift work” is probably carcinogenic: What about disturbed chronobiology in all walks of life? J. Occup. Med. Toxicol. 14, 29 (2019).
Davis, S., Mirick, D. K. & Stevens, R. G. Night Shift Work, Light at Night, and Risk of Breast Cancer. JNCI J. Natl Cancer Inst. 93, 1557–1562 (2001).
O’Leary, E. S. et al. Shift Work, Light at Night, and Breast Cancer on Long Island, New York. Am. J. Epidemiol. 164, 358–366 (2006).
Cordina-Duverger, E. et al. Night shift work and breast cancer: a pooled analysis of population-based case–control studies with complete work history. Eur. J. Epidemiol. 33, 369–379 (2018).
Tynes, T., Hannevik, M., Andersen, A., Vistnes, A. I. & Haldorsen, T. Incidence of breast cancer in Norwegian female radio and telegraph operators. Cancer Causes Control 7, 197–204 (1996).
Lie, J.-A. S. & Roessink, J. & Kjærheim, K. Breast Cancer and Night Work among Norwegian Nurses. Cancer Causes Control 17, 39–44 (2006).
Lie, J.-A. S., Kjuus, H., Zienolddiny, S., Haugen, A. & Kjaerheim, K. Breast Cancer Among Nurses: Is the Intensity of Night Work Related to Hormone Receptor Status? Am. J. Epidemiol. 178, 110–117 (2013).
Lie, J.-A. S. et al. Night Work and Breast Cancer Risk Among Norwegian Nurses: Assessment by Different Exposure Metrics. Am. J. Epidemiol. 173, 1272–1279 (2011).
Hansen, J. & Stevens, R. G. Case–control study of shift-work and breast cancer risk in Danish nurses: Impact of shift systems. Eur. J. Cancer 48, 1722–1729 (2012).
Hansen, J. & Lassen, C. F. Nested case–control study of night shift work and breast cancer risk among women in the Danish military. Occup. Environ. Med. 69, 551–556 (2012).
Knutsson, A. et al. Breast cancer among shift workers: results of the WOLF longitudinal cohort study. Scand. J. Work. Environ. Health 39, 170–177 (2013).
Wang, P. et al. Night-shift work, sleep duration, daytime napping, and breast cancer risk. Sleep. Med 16, 462–468 (2015).
Yang, W. et al. Long-term sleep habits and the risk of breast cancer among Chinese women: a case–control study. Eur. J. Cancer Prev. 28, 323–329 (2019).
Pronk, A. et al. Night-Shift Work and Breast Cancer Risk in a Cohort of Chinese Women. Am. J. Epidemiol. 171, 953–959 (2010).
Li, W. et al. Shift work and breast cancer among women textile workers in Shanghai. China Cancer Causes Control 26, 143–150 (2015).
Åkerstedt, T. et al. Night work and breast cancer in women: a Swedish cohort study. BMJ Open 5, e008127 (2015).
Travis, R. C. et al. Night Shift Work and Breast Cancer Incidence: Three Prospective Studies and Meta-analysis of Published Studies. J. Natl Cancer Inst. 108, djw169 (2016).
Koppes, L. L. J., Geuskens, G. A., Pronk, A., Vermeulen, R. C. H. & de Vroome, E. M. M. Night work and breast cancer risk in a general population prospective cohort study in The Netherlands. Eur. J. Epidemiol. 29, 577–584 (2014).
Monsees, G. M., Kraft, P., Hankinson, S. E., Hunter, D. J. & Schernhammer, E. S. Circadian genes and breast cancer susceptibility in rotating shift workers. Int. J. Cancer 131, 2547–2552 (2012).
Wegrzyn, L. R. et al. Rotating Night-Shift Work and the Risk of Breast Cancer in the Nurses’ Health Studies. Am. J. Epidemiol. 186, 532–540 (2017).
Vistisen, H. T. et al. Short-term effects of night shift work on breast cancer risk: a cohort study of payroll data. Scand. J. Work. Environ. Health 43, 59–67 (2017).
Jones, M. E. et al. Night shift work and risk of breast cancer in women: the Generations Study cohort. Br. J. Cancer 121, 172–179 (2019).
Rabstein, S. et al. Polymorphisms in circadian genes, night work and breast cancer: Results from the GENICA study. Chronobiol. Int. 31, 1115–1122 (2014).
Bustamante-Montes, L. P. et al. Night Shift Work and Risk of Breast Cancer in Women. Arch. Med. Res. 50, 393–399 (2019).
Szkiela, M., Kusideł, E., Makowiec-Dąbrowska, T. & Kaleta, D. Night Shift Work—A Risk Factor for Breast Cancer. Int. J. Environ. Res. Public Health 17, 659 (2020).
Szkiela, M., Kusideł, E., Makowiec-Dąbrowska, T. & Kaleta, D. How the Intensity of Night Shift Work Affects Breast Cancer Risk. Int. J. Environ. Res. Public Health 18, 4570 (2021).
Li, A. et al. Occupational risk factors and breast cancer in Beijing, China: a hospital-based case–control study. BMJ Open 12, e054151 (2022).
Gómez-Salgado, J. et al. Night Work and Breast Cancer Risk in Nurses: Multifactorial Risk Analysis. Cancers (Basel) 13, 1470 (2021).
Liu, F. C. et al. Night shift work, chemical coexposures and risk of female breast cancer in the Norwegian Offshore Petroleum Workers (NOPW) cohort: a prospectively recruited case-cohort study. BMJ Open 12, e056396 (2022).
Sweeney, M. R., Sandler, D. P., Niehoff, N. M. & White, A. J. Shift Work and Working at Night in Relation to Breast Cancer Incidence. Cancer Epidemiol. Biomark. Prev. 29, 687–689 (2020).
Harris, M. A. et al. Use of a Canadian Population-Based Surveillance Cohort to Test Relationships Between Shift Work and Breast, Ovarian, and Prostate Cancer. Ann. Work Expo. Heal. 64, 387–401 (2020).
Härmä, M., Ojajärvi, A., Koskinen, A., Lie, J.-A. & Hansen, J. Shift work with and without night shifts and breast cancer risk in a cohort study from Finland. Occup. Environ. Med. 80, 1–6 (2023).
Gustavsson, P. et al. Night work and breast cancer risk in a cohort of female healthcare employees in Stockholm, Sweden. Occup. Environ. Med. 80, 372–376 (2023).
Schernhammer, E. et al. The association between night shift work and breast cancer risk in the Finnish twins cohort. Eur. J. Epidemiol. 38, 533–543 (2023).
Chowdhury, R., Shah, D. & Payal, A. Healthy worker effect phenomenon: Revisited with emphasis on statistical methods – A review. Indian J. Occup. Environ. Med. 21, 2 (2017).
Zhang, Y. & Papantoniou, K. Night shift work and its carcinogenicity. Lancet Oncol. 20, e550 (2019).
Acknowledgements
This work was supported by National Recovery and Resilience Plan (PNRR) project “Night-shift work and breast cancer”, PNRR-MAD-2022-12376823, CUP H43C22001200006; strengthening and enhancement of biomedical research of the National Health Service (Sistema Sanitario Nazionale, SSN), funded by the European Union – NextGenerationEU.
Author information
Authors and Affiliations
Contributions
S.V., and C.F.: Concept, design, and draft of the manuscript. T.F., Y.P., and G.S.: Preparation of tables and figures. All authors: Critical revision of the manuscript. All authors: Reading and approval of the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vivarelli, S., Formica, T., Puliatti, Y. et al. Night shift work and breast cancer: from etiopathology to precision risk analysis. npj Breast Cancer 12, 7 (2026). https://doi.org/10.1038/s41523-025-00863-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-025-00863-3