Abstract
Bullous keratopathy (BK) is known to present with corneal edema and Descemet's folds, which can cause corneal astigmatism. However, no report quantitatively evaluated BK astigmatism by separating it into regular and irregular astigmatism. This study investigated the regular and irregular astigmatism of the anterior and posterior corneal surface with Fourier harmonic analysis and anterior segment optical coherence tomography. Preoperative data from 43 eyes of 41 BK patients who received corneal endothelial transplantation were compared with the data from 43 eyes of 43 subjects without corneal disease. Anterior and posterior cylinder power, central corneal thickness (CCT) and thinnest corneal thickness were significantly greater in BK. With Fourier harmonic analysis, BK eyes were found to have significantly larger anterior and posterior regular astigmatism, asymmetry component and higher-order irregularity. Asymmetry component and higher-order irregularity that accounted for the posterior irregular astigmatism increased as CCT increased in BK. Higher-order irregularity in the posterior cornea also positively correlated with worsening best corrected visual acuity. Subgroup analysis found significant correlations between CCT and posterior higher-order irregularity for intraocular surgery and laser iridotomy, but not Fuchs endothelial corneal dystrophy. This study has significance in that it revealed the characteristics of the corneal posterior irregular astigmatism of BK.
Similar content being viewed by others
Introduction
Bullous keratopathy (BK) is a condition that results from damages to the corneal endothelium, a monolayer of cells located on the posterior surface of the cornea. The corneal endothelial cells have focal tight junctions and Na+/K+-ATPases that help to maintain the cornea in a dehydrated state1,2. With decreased corneal endothelial cell density, there may be stromal edema and bullae formation in the subepithelial and epithelial layers. Causes of BK include cataract surgery, trabeculectomy, laser iridotomy, Fuchs’ endothelial corneal dystrophy, penetrating or blunt trauma, and viral infections3,4,5. Patients can develop severe vision loss and possibly pain with disease progression. The gold standard treatment is a corneal transplantation although several options are available for symptom management6,7,8,9,10.
The BK cornea under the slit-lamp may reveal corneal edema and Descemet’s folds11, which are pathological changes that can increase the irregularity of the anterior and posterior surfaces. There are also BK patients with poor vision despite corneal transparency, suggesting that another factor such as a distortion in corneal shape could have caused the decreased visual acuity. Currently, several methods are used in clinical practice for the evaluation of BK. These include the most basic evaluation with slit-lamp examination for signs such as corneal subepithelial bullae and stromal swelling, specular microscopy to check for decreased endothelial cell density, and ultrasonic pachymetry to determine the corneal thickness, which is also effective in advanced cases as an indicator of corneal endothelial function12. However, these findings represent gross changes that cannot be used to determine details regarding the corneal shape or corneal refraction. The slit lamp examination may be prone to operator dependent variability, and the confirmation of decreased endothelial cell density with a specular microscope may be effective in the early stages, but imaging becomes difficult with disease progression. While the refractive power can be evaluated using keratometry and corneal topography with Scheimpflug imaging, these cannot evaluate the back of the cornea in advanced cases13. Aside from the shortage of information regarding the posterior cornea, previous studies have focused on the postoperative topographic changes associated with corneal transplantation instead of BK itself14,15,16,17,18. In addition, no report quantitatively assessed the astigmatism of BK by separating it into regular and irregular astigmatism.
Fourier harmonic analysis of topographic data is a method that quantitatively separates regular and irregular astigmatism. It deconstructs raw corneal power data into a combination of periodic trigonometric functions and reconstructs these into four components: spherical component, regular astigmatism, asymmetry component, and higher-order irregularity19,20,21. This method has been used for investigating the optical quality of the cornea with cataract surgery22,23,24, trabeculectomy25, scleral buckling26, vitrectomy27, penetrating keratoplasty28,29, photorefractive keratectomy30,31,32, laser in situ keratomileusis33, orthokeratology34, keratoconus35,36,37, and pterygium38.
The early studies on Fourier harmonic analysis used topographic data obtained from videokeratography. However, advancements in OCT technology later made it possible to use anterior segment optical coherence tomography (AS-OCT) to obtain topographic data for both the anterior surface and the posterior surface of the cornea. Fourier harmonic analysis with AS-OCT has been used in recent years to evaluate the topographic changes associated with primary and recurrent pterygium39, ptosis surgery40, penetrating keratoplasty for keratoconus41, rigid gas permeable contact lens use for keratoconus42, and Fuchs endothelial corneal dystrophy (FECD)43. A study also analyzed the relationship between regular astigmatism pattern and irregular astigmatism in normal subjects44. AS-OCT utilizes long-wavelength infrared light that can be used to assess the posterior surface of the cornea even in eyes with corneal opacity45. This is an advantage over Scheimpflug corneal tomography, which uses visible light that cannot pass through the opaque cornea. The components of Fourier harmonic analysis can be useful references for decisions regarding the surgical timing and the surgery method for BK if a relationship is found with increases in corneal thickness or decreases in visual acuity. Since spectacles can correct the spherical component and regular astigmatism but not the asymmetry component and higher-order irregularity, an understanding of the regular and irregular astigmatism associated with BK through Fourier harmonic analysis can help with clinical decision making.
In this study, we evaluated the anterior and posterior corneal astigmatism of BK by Fourier harmonic analysis of corneal topography with AS-OCT. We also looked at the relationship between central corneal thickness (CCT), best corrected visual acuity (BCVA) and each component of the Fourier harmonic analysis.
Results
Patient demographics
Forty-three eyes of 43 subjects without corneal disease as control and 43 eyes of 41 patients with BK were analyzed in this study. The average age was 69.3 ± 9.3 years and 73.3 ± 11.8 years, respectively. There was no statistically significant difference between the 2 groups for age, gender, and right eye to left eye ratio. The BCVA was − 0.06 ± 0.04 for the control group and 1.15 ± 0.49 for the BK group (p < 0.0001). Of the 43 BK eyes, 17 (39.5%) were the result of trabeculectomy, 4 (9.3%) were the result of cataract surgery, 17 (39.5%) were caused by laser iridotomy, and 5 (11.6%) were due to FECD (Table 1).
AS-OCT measurements and Fourier components
Anterior cylinder power, posterior cylinder power, CCT and thinnest corneal thickness were significantly greater in the BK group but there was no significant difference in the anterior or posterior averaged keratometry (p < 0.0001, p = 0.0003, p < 0.0001, p < 0.0001, respectively) (Table 1). The mean CCT was 529.4 ± 14.2 µm in the control group and 747.6 ± 102.1 µm in the BK group (p < 0.0001). Representative OCT images of the control group and the BK group are provided for comparison (Fig. 1). With Fourier harmonic analysis, the BK group was found to have significantly larger anterior and posterior regular astigmatism, asymmetry component and higher-order irregularity (p < 0.0001 for all) (Table 2). These increases were seen within the central 3 mm and 6 mm zones.
Representative Fourier maps taken with anterior segment optical coherence tomography in (a) control without corneal disease and (b) subject with bullous keratopathy (BK). The original color-coded map is separated into spherical component, regular astigmatism, asymmetry component and higher-order irregularity. Fourier indices from the central 3 mm and 6 mm zones are shown for the anterior, posterior, and anterior + posterior cornea. Central corneal thickness is 530 µm for the control and 724 µm for BK.
CCT and linear regression analysis
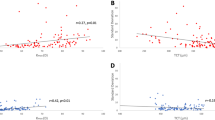
When linear regression analysis was used to check for the relationship between CCT and the 4 components of Fourier harmonic analysis in the BK group, no significant correlation was detected in the anterior cornea. With the posterior cornea, there were significant positive correlations between CCT and the spherical component within the central 6 mm zone (R2 = 0.096, p = 0.04), as well as asymmetry and higher-order of irregularity within the central 3 mm (R2 = 0.18, p = 0.005 for asymmetry; R2 = 0.47, p < 0.001 for higher-order irregularity) and 6 mm zones (R2 = 0.16, p = 0.008 for asymmetry; R2 = 0.47, p < 0.001 for higher-order irregularity) (Fig. 2).
Linear regression between central corneal thickness (CCT) and each Fourier component in the anterior and posterior cornea within the central (a) 3 mm and (b) 6 mm zones. Significant correlations are seen for the posterior cornea between CCT and the spherical component within the central 6 mm zone (R2 = 0.096, p = 0.04), asymmetry within the central 3 mm (R2 = 0.18, p = 0.005), higher-order irregularity within the central 3 mm (R2 = 0.47, p < 0.001), asymmetry within the central 6 mm zone (R2 = 0.16, p = 0.008) and higher-order irregularity within the central 6 mm zone (R2 = 0.47, p < 0.001). Regression lines are drawn for graphs with statistical significance (*p < 0.05).
Sub-group analysis was done after dividing the BK etiologies into 3 groups: (i) intraocular surgery—trabeculectomy or cataract surgery (21 eyes; 48.8%), (ii) laser iridotomy (17 eyes; 39.5%) and (iii) FECD (5 eyes; 11.6%). No statistical significance was seen with the anterior cornea in all the groups. For the posterior cornea, the intraocular surgery group had significant positive correlations between CCT and the spherical component within the central 6 mm zone (R2 = 0.23, p = 0.03), as well as the higher-order irregularity within the central 3 mm (R2 = 0.44, p = 0.001) and 6 mm zones (R2 = 0.43, p = 0.001). The laser iridotomy group had significant positive correlations between CCT and the higher-order irregularity within the central 3 mm (R2 = 0.58, p < 0.001) and 6 mm zones (R2 = 0.59, p < 0.001). No significant correlations were seen in the FECD group (Fig. 3).
Subgroup analysis of the posterior cornea based on the cause of bullous keratopathy: intraocular surgery, laser iridotomy and Fuchs endothelial corneal dystrophy (FECD). Linear regression analysis is done between central corneal thickness (CCT) and each Fourier component within the central (a) 3 mm and (b) 6 mm zones. Linear regression shows significant correlations between CCT and the spherical component within the central 6 mm zone (R2 = 0.23, p = 0.03), the higher-order irregularity within the central 3 mm zone (R2 = 0.44, p = 0.001) and the higher-order irregularity within the central 6 mm zone (R2 = 0.43, p = 0.001) for the intraocular surgery group. The laser iridotomy group has significant correlations between CCT and the higher-order irregularity within the central 3 mm zone (R2 = 0.58, p < 0.001) and the central 6 mm zone (R2 = 0.59, p < 0.001). Regression lines are drawn for graphs with statistical significance (*p < 0.05).
BCVA and linear regression analysis
Associations with BCVA (logMAR) were also looked at for the 4 components of Fourier harmonic analysis and CTT using linear regression analysis. No significant association was seen with the Fourier harmonic analysis in the anterior cornea. Statistically significant associations were seen with higher-order irregularity in the central 3 mm (R2 = 0.16, p = 0.008) and 6 mm zones (R2 = 0.15, p = 0.01) of the posterior cornea, as well as CCT (R2 = 0.18, p = 0.0043) (Fig. 4). With subgroup analysis that divided BK etiologies into three groups (intraocular surgery, laser iridotomy and FECD), only CCT significantly correlated with BCVA in the intraoperative surgery group (R2 = 0.25, p = 0.020).
Linear regression between (a) each Fourier component of the posterior cornea and logMAR best corrected visual acuity (BCVA), as well as (b) CCT and logMAR BCVA. Significant associations are seen with higher-order irregularity in the central 3 mm zone (R2 = 0.16, p = 0.008) and the central 6 mm zone (R2 = 0.15, p = 0.01). A significant association is seen between CCT and logMAR BCVA (R2 = 0.18, p = 0.0043) With subgroup analysis that divides BK etiologies into three groups (intraocular surgery, laser iridotomy and FECD), only CCT in the intraoperative surgery group significantly correlates with BCVA (R2 = 0.25, p = 0.020). Regression lines are drawn for graphs with statistical significance (*p < 0.05).
Discussion
This study is the first to examine the regular and irregular astigmatism in BK with Fourier harmonic analysis and AS-OCT. Fourier harmonic analysis enabled the quantitative assessment of the astigmatism, while AS-OCT provided a better assessment of the posterior cornea compared to older imaging technologies. Compared to the control group, BK eyes had increased regular and irregular astigmatism for the anterior and posterior cornea. There was no significant difference in the spherical component of the Fourier harmonic analysis between the control group and BK eyes, indicating that BK did not result in prominent protrusion or flattening. The asymmetry component and higher-order irregularity that accounted for the posterior irregular astigmatism within the central 3 mm and 6 mm zones increased as the corneal thickness increased in BK. This positive correlation was not seen in the anterior cornea. The positive correlation seen in the posterior cornea suggests that as the cornea thickens with worsening BK, the back of the cornea becomes increasingly irregular. This may be associated with Descemet folds seen on the clinical exam. Furthermore, the significant correlation between higher-order irregularity and BCVA as well as the significant correlation between CCT and BCVA point to a relationship between posterior irregular astigmatism and worsening visual function.
Other studies that looked at astigmatism in BK differed from our study in several ways regarding the study design. Yamaguchi et al. looked at the anterior and posterior corneal irregularity in 13 BK eyes that underwent Descemet-stripping endothelial keratoplasty (DSEK) using a rotating Scheimpflug camera and Zernike polynomial decomposition for corneal wavefront aberrations14. Although Yamaguchi et al. also found a significant increase between the control group and the BK group for preoperative anterior and posterior irregularity, the irregularity was not broken down into different components. Spadea et al. looked at 20 BK eyes that underwent DSEK with videokeratography maps and Zernike polynomial decomposition for corneal wavefront aberrations but followed the patients for a longer postoperative period than Yamaguchi et al. and investigated only the anterior irregularity18. Spadea et al. also found increased anterior astigmatism in the preoperative BK eyes compared to the control but did not analyze the different components that made up the astigmatism. Both studies had fewer cases than our study and did not analyze the relationship with CCT. The third study, by Oie et al., investigated the anterior and posterior cornea for FECD with Fourier harmonic analysis and AS-OCT43. They divided 75 eyes of 43 FECD subjects into 5 categories of severity and analyzed the association between the modified Krachmer grade or CCT and each component to see if there might be differences among groups. They also assessed the relationship between each component and BCVA using the Spearman rank correlation and found significant associations with the spherical power and asymmetry in the anterior cornea, as well as the spherical power, asymmetry, and higher-order irregularity in the posterior cornea. Their results differed from ours likely because we used a linear regression analysis, included other etiologies of BK, and had fewer FECD eyes.
The relationship between CCT and each component of the Fourier harmonic analysis was not investigated by Oie et al., so our study fills a gap within the existing literature by demonstrating significant associations between CCT and several components of the Fourier harmonic analysis in the posterior cornea.
There are two notable limitations with this study. One is that the small sample size could have decreased the statistical power and made it more difficult to detect significant findings. The effect would have been especially large with the FECD group in the subgroup analysis. The other is that this was a retrospective cross-sectional study, so how the state of the cornea changed for each subject and the exact duration of bullous keratopathy were not studied. In addition, the decision to undergo or not undergo surgery could have been influenced by the subjects’ social circumstances. In the future, it will be important to conduct a larger cohort study to acquire data at multiple time points, preferably starting before the onset of bullous keratopathy.
In conclusion, this study demonstrated that both regular and irregular corneal astigmatism increased in BK eyes compared to eyes without corneal disease. A significant correlation was seen between CCT and the spherical component, asymmetry and higher-order irregularity in the posterior cornea, and between BCVA and the higher-order irregularity of the posterior cornea. Components of the Fourier harmonic analysis did not show a correlation with CCT or BCVA in the anterior cornea. Based on these findings, advanced bullous keratopathy increases irregular astigmatism of the posterior cornea. Since posterior irregular astigmatism cannot be fully corrected with glasses or contact lenses, corneal transplantation is recommended in such cases to improve visual acuity.
Methods
This retrospective observational study was approved by the Institutional Review Board of the Research Ethics Committee of the University of Tokyo School of Medicine (Examination No. 2020006NI) and adhered to the tenets of the Declaration of Helsinki. The need for written patient consent was waived due to the study’s retrospective nature. Information from medical charts of patients with BK who received corneal endothelial transplantation (Descemet stripping automated endothelial keratoplasty [DSAEK] or Descemet membrane endothelial keratoplasty [DMEK]) between May 2017 and August 2021 was reviewed and compared with that of age- and gender-matched subjects without corneal disease. BK was diagnosed by corneal specialists based on the clinical findings of epithelial and stromal edema, as well as a corneal endothelial density below 500 cells/mm2. Preoperative corneal topography was done using AS-OCT (CASIA2; Tomey Corporation, Tokyo, Japan). Patients who were not evaluated with AS-OCT during the preoperative period were excluded from the study.
BCVA was measured with decimal visual acuity and expressed in logarithm of the minimum angle of resolution (logMAR) units. CCT, Kmax, AvgK, and corneal topographic data with Fourier harmonic analysis were obtained via AS-OCT and its built-in software (CASIA2; Tomey Corporation, Tokyo, Japan). CASIA2 is capable of 10 µm axial and 30 µm transverse high-resolution imaging and has a scan depth of 13 mm, scan speed of 50,000 A-scans per second and 1310 nm wavelength light source. The corneal topography of CASIA2 analyzes the shape of the anterior and posterior corneal surfaces from high-resolution AS-OCT images. Fourier series harmonic analysis divided corneal topographic data into four components: spherical, regular astigmatism, asymmetry, and higher-order irregularity. Calculations for Fourier series harmonic analysis were as described in a previous report19. Dioptric powers on a mire ring i, Fi(σ ), were converted into trigonometric components as follows: Fi(σ ) = a0 + c1 cos(σ − α1) + c2 cos 2(σ − α2) + c3 cos 3(σ − α3) + ⋯ + cn cos n(σ − αn ). Spherical component is a0, regular astigmatism is 2c2, asymmetry is 2c1, and higher-order irregularity is the sum of c3…cn. Values of the rings that made up the central 3 mm and 6 mm zones were averaged for each parameter.
Statistical analysis was conducted with Microsoft Excel (Office 365) and Graphpad Prism 9.3.1 (Graphpad Software. San Diego, CA, USA). The unpaired t-test was used for continuous variables. The Chi-square test was used for categorical variables. p value less than 0.05 was considered statistically significant. Normal eyes from age- and gender-matched subjects were selected using the MatchIt package for R (version 3.6.1; R Foundation for Statistical Computing, Vienna, Austria). Simple linear regression analysis was done using Graphpad Prism 9.3.1 to calculate the goodness of fit (R2) and the statistical significance of a line with non-zero slope.
Ethical approval
This retrospective observational study was approved by the Research Ethics Committee of the University of Tokyo School of Medicine (Examination No. 2020006NI). This study was conducted under the principles of the Declaration of Helsinki.
Consent to participate
Due to the observational nature of the study and the use of medical records, the Institutional Review Board waived the requirement of written consent. Patients were given the opportunity to opt out of the study.
Data availability
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
References
Riley, M. V., Winkler, B. S., Starnes, C. A., Peters, M. I. & Dang, L. Regulation of corneal endothelial barrier function by adenosine, cyclic AMP, and protein kinases. Invest Ophthalmol. Vis. Sci. 39, 2076–2084 (1998).
Bonanno, J. A. Molecular mechanisms underlying the corneal endothelial pump. Exp. Eye Res. 95, 2–7. https://doi.org/10.1016/j.exer.2011.06.004 (2012).
Shimazaki, J. et al. National survey on bullous keratopathy in Japan. Cornea 26, 274–278. https://doi.org/10.1097/ICO.0b013e31802c9e19 (2007).
Wang, X., Wang, W., Xu, J. & Wang, Y. Analysis of causes of bullous keratopathy in East China: A 10-year retrospective study. Graefes Arch. Clin. Exp. Ophthalmol. 250, 307–308. https://doi.org/10.1007/s00417-010-1606-4 (2012).
Papaioannou, L., Tsolkas, G., Theodossiadis, P. & Papathanassiou, M. An atypical case of herpes simplex virus endotheliitis presented as bullous keratopathy. Ocul. Immunol. Inflamm. 21, 475–477. https://doi.org/10.3109/09273948.2013.815784 (2013).
Khan, M. S. et al. Corneal Collagen Cross Linking (CXL) in treatment of Pseudophakic Bullous Keratopathy. Pak. J. Med. Sci. 32, 965–968. https://doi.org/10.12669/pjms.324.10138 (2016).
Ono, T. et al. Sustainability of Pain Relief After Corneal Collagen Cross-Linking in Eyes With Bullous Keratopathy. Asia Pac. J. Ophthalmol. (Phila.) 7, 291–295. https://doi.org/10.22608/APO.201832 (2018).
Kasai, K. et al. A prospective, randomized clinical study comparing accelerated corneal collagen crosslinking with 5% NaCl hypertonic saline for bullous keratopathy in Asian eyes. Medicine 98, e18256. https://doi.org/10.1097/MD.0000000000018256 (2019).
Choy, B. N. K. et al. Randomized control trial on the effectiveness of collagen cross-linking on bullous keratopathy. Cornea 39, 1341–1347. https://doi.org/10.1097/ICO.0000000000002395 (2020).
Chow, S. C. & Chan, J. C. Review on the use of topical ocular hypertonic saline in corneal edema. Cornea 40, 533–539. https://doi.org/10.1097/ICO.0000000000002652 (2021).
Goncalves, E. D., Paris Fdos, S., Gomes, J. A., Kanecadan, L. & Campos, M. Bullous keratopathy. Ophthalmology 118(2303–2303), e2301-2302. https://doi.org/10.1016/j.ophtha.2011.05.034 (2011).
Chang, D. T., Pantcheva, M. B. & Noecker, R. J. Corneal thickness and intraocular pressure in edematous corneas before and after Descemet stripping with automated endothelial keratoplasty. Cornea 29, 1125–1130. https://doi.org/10.1016/S0161-6420(03)00659-6 (2010).
Seitz, B., Langenbucher, A., Küchle, M. & Naumann, G. O. Impact of graft diameter on corneal power and the regularity of postkeratoplasty astigmatism before and after suture removal. Ophthalmology 110, 2162–2167. https://doi.org/10.1016/S0161-6420(03)00659-6 (2003).
Yamaguchi, T. et al. Effect of anterior and posterior corneal surface irregularity on vision after Descemet-stripping endothelial keratoplasty. J. Cataract Refract. Surg. 35, 688–694. https://doi.org/10.1016/j.jcrs.2008.11.062 (2009).
Hayashi, T., Hirayama, Y., Yamada, N., Shimazaki-Den, S. & Shimazaki, J. Descemet stripping automated endothelial keratoplasty for bullous keratopathy with an irregular posterior surface. Cornea 32, 1183–1188. https://doi.org/10.1097/ICO.0b013e31829623d6 (2013).
Javadi, M. A., Feizi, S., Jafari, R., Mirbabaee, F. & Ownagh, V. Descemet stripping automated endothelial keratoplasty in Fuchs’ endothelial dystrophy versus pseudophakic bullous keratopathy. J. Ophthalmic Vis. Res. 11, 372–378. https://doi.org/10.4103/2008-322X.194073 (2016).
Kim, S. E., Lim, S. A., Byun, Y. S. & Joo, C. K. Comparison of long-term clinical outcomes between Descemet’s stripping automated endothelial keratoplasty and penetrating keratoplasty in patients with bullous keratopathy. Korean J. Ophthalmol. 30, 443–450. https://doi.org/10.3341/kjo.2016.30.6.443 (2016).
Spadea, L., Santamaria, V., Vingolo, E. M. & Cagini, C. Anterior corneal surface irregularity after Descemet-stripping endothelial keratoplasty for bullous keratopathy. Eur. J. Ophthalmol. 26, 209–215. https://doi.org/10.5301/ejo.5000698 (2016).
Oshika, T., Tomidokoro, A., Maruo, K., Tokunaga, T. & Miyata, N. Quantitative evaluation of irregular astigmatism by fourier series harmonic analysis of videokeratography data. Invest Ophthalmol. Vis. Sci. 39, 705–709 (1998).
Hjortdal, J. O., Erdmann, L. & Bek, T. Fourier analysis of video-keratographic data. A tool for separation of spherical, regular astigmatic and irregular astigmatic corneal power components. Ophthalmic Physiol. Opt. 15, 171–185 (1995).
Olsen, T., Dam-Johansen, M., Bek, T. & Hjortdal, J. O. Evaluating surgically induced astigmatism by Fourier analysis of corneal topography data. J. Cataract Refract. Surg. 22, 318–323. https://doi.org/10.1016/s0886-3350(96)80243-4 (1996).
Olsen, T., Dam-Johansen, M., Bek, T. & Hjortdal, J. O. Corneal versus scleral tunnel incision in cataract surgery: A randomized study. J. Cataract Refract. Surg. 23, 337–341. https://doi.org/10.1016/s0886-3350(97)80176-9 (1997).
Hayashi, K., Hayashi, H., Oshika, T. & Hayashi, F. Fourier analysis of irregular astigmatism after implantation of 3 types of intraocular lenses. J. Cataract Refract. Surg. 26, 1510–1516. https://doi.org/10.1016/s0886-3350(00)00435-1 (2000).
Oshika, T., Sugita, G., Tanabe, T., Tomidokoro, A. & Amano, S. Regular and irregular astigmatism after superior versus temporal scleral incision cataract surgery. Ophthalmology 107, 2049–2053. https://doi.org/10.1016/s0161-6420(00)00379-1 (2000).
Hayashi, K., Hayashi, H., Oshika, T. & Hayashi, F. Fourier analysis of irregular astigmatism after trabeculectomy. Ophthalmic Surg. Lasers 31, 94–99 (2000).
Tomidokoro, A., Oshika, T. & Kojima, T. Corneal astigmatism after scleral buckling surgery assessed by Fourier analysis of videokeratography data. Cornea 17, 517–521. https://doi.org/10.1097/00003226-199809000-00009 (1998).
Okamoto, F. et al. Changes in corneal topography after 25-gauge transconjunctival sutureless vitrectomy versus after 20-gauge standard vitrectomy. Ophthalmology 114, 2138–2141. https://doi.org/10.1016/j.ophtha.2007.01.034 (2007).
Kagaya, F., Tomidokoro, A., Tanaka, S., Amano, S. & Oshika, T. Fourier series harmonic analysis of corneal topography following suture removal after penetrating keratoplasty. Cornea 21, 256–259. https://doi.org/10.1097/00003226-200204000-00004 (2002).
Miyai, T. et al. Visual acuity measurements using Fourier series harmonic analysis of videokeratography data in eyes after penetrating keratoplasty. Ophthalmology 112, 420–424. https://doi.org/10.1016/j.ophtha.2004.09.026 (2005).
Bessho, K., Maeda, N., Watanabe, H., Shimomura, Y. & Tano, Y. Fourier analysis of corneal astigmatic changes following photorefractive keratectomy. Semin. Ophthalmol. 18, 23–28. https://doi.org/10.1076/soph.18.1.23.14073 (2003).
Keller, P. R., McGhee, C. N. & Weed, K. H. Fourier analysis of corneal topography data after photorefractive keratectomy. J. Cataract Refract. Surg. 24, 1447–1455. https://doi.org/10.1016/s0886-3350(98)80165-x (1998).
Tomidokoro, A. et al. Corneal irregular astigmatism and contrast sensitivity after photorefractive keratectomy. Ophthalmology 108, 2209–2212. https://doi.org/10.1016/s0161-6420(01)00847-8 (2001).
Baek, T. M., Lee, K. H., Tomidokoro, A. & Oshika, T. Corneal irregular astigmatism after laser in situ keratomileusis for myopia. Br. J. Ophthalmol. 85, 534–536. https://doi.org/10.1136/bjo.85.5.534 (2001).
Hiraoka, T. et al. Quantitative evaluation of regular and irregular corneal astigmatism in patients having overnight orthokeratology. J. Cataract Refract. Surg. 30, 1425–1429. https://doi.org/10.1016/j.jcrs.2004.02.049 (2004).
Oshika, T., Tanabe, T., Tomidokoro, A. & Amano, S. Progression of keratoconus assessed by fourier analysis of videokeratography data. Ophthalmology 109, 339–342. https://doi.org/10.1016/s0161-6420(01)00903-4 (2002).
Tomidokoro, A. et al. Changes in anterior and posterior corneal curvatures in keratoconus. Ophthalmology 107, 1328–1332. https://doi.org/10.1016/s0161-6420(00)00159-7 (2000).
Suzuki, M. et al. Longitudinal changes in corneal irregular astigmatism and visual acuity in eyes with keratoconus. Jpn. J. Ophthalmol. 51, 265–269. https://doi.org/10.1007/s10384-007-0453-2 (2007).
Tomidokoro, A., Oshika, T., Amano, S., Eguchi, K. & Eguchi, S. Quantitative analysis of regular and irregular astigmatism induced by pterygium. Cornea 18, 412–415. https://doi.org/10.1097/00003226-199907000-00004 (1999).
Ono, T. et al. Comparison of Corneal Irregularity After Recurrent and Primary Pterygium Surgery Using Fourier Harmonic Analysis. Transl Vis. Sci. Technol. 10, 13. https://doi.org/10.1167/tvst.10.11.13 (2021).
Yamamoto, R. et al. Assessment of long-term anterior and posterior topographic changes in the cornea after ptosis surgery using Fourier harmonic analysis. Cornea 40, 440–444. https://doi.org/10.1097/ICO.0000000000002429 (2021).
Ono, T. et al. Corneal topography in keratoconus evaluated more than 30 years after penetrating keratoplasty: A Fourier harmonic analysis. Sci. Rep. 10, 14880. https://doi.org/10.1038/s41598-020-71818-w (2020).
Koh, S. et al. Corneal tomographic changes during corneal rigid gas-permeable contact lens wear in keratoconic eyes. Br. J. Ophthalmol. 106, 197–202. https://doi.org/10.1136/bjophthalmol-2020-317057 (2022).
Oie, Y. et al. Fourier analysis on regular and irregular astigmatism of anterior and posterior corneal surfaces in Fuchs endothelial corneal dystrophy. Am. J. Ophthalmol. 223, 33–41. https://doi.org/10.1016/j.ajo.2020.09.045 (2021).
Ueno, Y. et al. Comparison of corneal irregular astigmatism by the type of corneal regular astigmatism. Sci. Rep. 11, 15769. https://doi.org/10.1038/s41598-021-95358-z (2021).
Fukuda, R. et al. Noninvasive observations of peripheral angle in eyes after penetrating keratoplasty using anterior segment fourier-domain optical coherence tomography. Cornea 31, 259–263. https://doi.org/10.1097/ICO.0b013e318226daa9 (2012).
Funding
The authors have not received a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
L.W.C. and T.M. designed and conducted the study. T.O., Y.H., M.T., Y.A., T.O., Y.T., and T.T. contributed to data collection and management. L.W.C., T.O., Y.H. and T.M. participated in the preparation and the analysis of the manuscript. M.A. and T.M. reviewed and supervised the study. All authors critically reviewed the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, L.W., Ono, T., Hashimoto, Y. et al. Regular and irregular astigmatism of bullous keratopathy using Fourier harmonic analysis with anterior segment optical coherence tomography. Sci Rep 12, 17865 (2022). https://doi.org/10.1038/s41598-022-22144-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-022-22144-w
This article is cited by
-
Corneal Fourier harmonic analysis in prostaglandin-associated periorbitopathy patients with blepharoptosis
Japanese Journal of Ophthalmology (2025)
-
Corneal irregularity of the anterior and posterior surface in patients with limbal stem cell deficiency evaluated with anterior-segment optical coherence tomography
Japanese Journal of Ophthalmology (2025)