Abstract
Monkeypox (Mpox) is a growing public health concern, with complex interactions within host systems contributing to its impact. This study employs multi-omics approaches to uncover therapeutic targets and potential drug repurposing opportunities to better understand Mpox’s molecular pathogenesis. We developed an in silico host-pathogen interaction (HPI) network and applied weighted gene co-expression network analysis (WGCNA) to explore interactions between Mpox and host proteins. Subtype-specific host-pathogen protein-protein interaction networks were constructed, and key modules from the HPI and WGCNA were integrated to identify significant host proteins. To predict upstream signaling pathways and transcription factors, we used eXpression2Kinases and ChIP-X Enrichment Analysis. The multi-Steiner trees method was applied to compare our findings with those from FDA-approved antiviral drugs. Analysis of 55 differentially expressed genes in Mpox infection revealed 11 kinases and 15 transcription factors as key regulators. We identified 16 potential drug targets, categorized into 8 proviral genes (ESR2, ERK1, ERK2, P38, JNK1, CDK4, GSK3B, STAT3) designated for inhibition, and 8 antiviral genes (IKKA, HDAC1, HIPK2, TF65, CSK21, HIPK2, ESR2, GSK3B) designated for activation. Proviral genes are involved in the AKT, Wnt, and STAT3 pathways, while antiviral genes impact the AP-1, NF-κB, apoptosis, and IFN pathways. Promising FDA-approved candidates were identified, including kinase inhibitors, steroid hormone receptor agonists, STAT3 inhibitors, and notably Niclosamide. This study enhances our understanding of Mpox by identifying key therapeutic targets and potential repurposable drugs, providing a valuable framework for developing new treatments.
Similar content being viewed by others
Introduction
Monkeypox (Mpox), driven by the monkeypox virus, triggered a WHO emergency declaration in 2022, with 94,766 cases and 182 deaths reported across 117 countries by 20241,2. Mpox shares genetic similarities with cowpox, variola, and vaccinia viruses3. Its genome comprises 196,858 base pairs and over 200 genes, including 190 open reading frames. While historically less severe than smallpox, Mpox may become more virulent due to its 21% mutation rate, impacting its evolutionary and pathogenic dynamics4,5.
Host-pathogen interaction (HPI) analysis is pivotal for identifying drug targets and understanding viral-host dynamics. By dissecting these interactions, researchers can identify specific drug targets that disrupt viral replication and modulate host immune responses6. Such insights are critical for the rational design of targeted therapies and effective vaccines, enhancing our ability to combat viral diseases and their associated pathologies7. While genomic data on various poxviruses is available, integrating HPI data from multi-species databases-especially those related to vaccinia and variola- can provide valuable insights into Mpox7,8. This targeted approach unravels the complex interactions between the Mpox virus and host cells by analyzing gene expression in two different types of infected host cells. This analysis clarifies the immunoevasion process of the Mpox virus by network analysis of downregulated interferon pathways and altered pro-inflammatory cytokine signaling9,10.
Numerous in vitro and in vivo studies have shown that Weighted Gene Co-expression Network Analysis (WGCNA) effectively identifies clusters of genes with similar expression patterns and uncovers key gene modules associated with viral disease progression11,12,13,14,15. WGCNA is a powerful in silico tool for investigating co-expression networks across multiple diseases, especially in viral infections, revealing potential druggable targets for human immunodeficiency virus (HIV)-116, hepatitis B virus (HBV)17,18, hepatitis C virus17,19, syndrome coronavirus 211,14,20, and Zika virus21. This method has identified crucial gene modules associated with HBV-induced hepatocellular carcinoma replication and immune response, highlighting new targets for hepatocarcinogenesis and HIV progression17,18,19. Additionally, Michlmayr et al., applied WGCNA to 41 samples from individuals infected with the Zika virus, identifying a novel immunophenotypic gene cluster linked to neuroinflammation and innate immune response21. These findings demonstrate the effectiveness of WGCNA in elucidating the molecular mechanisms of viral diseases and guiding the development of targeted therapies.
In this study, we integrate WGCNA with HPI analysis to investigate the molecular mechanisms of Mpox. WGCNA identifies key gene modules and their co-expression relationships, while HPI analysis characterizes the interactions between Mpox proteins and host cellular components, revealing how the virus alters host gene expression. This combined approach allows us to identify specific host gene modules significantly affected during Mpox infection22. We focus on elucidating the regulatory networks involving transcription factors and kinases that mediate host response to the viral challenge23. Our study identifies potential key drug targets, including kinase inhibitors, hormone-based therapies, and niclosamide, that could modulate NF-kB signaling, IFN signaling, as well as apoptosis. These agents may also impact proviral pathways such as PI3K/AKT, Wnt signaling, and STAT3 signaling. By integrating WGCNA and HPI analysis, we enhance our understanding of the immunopathogenesis of Mpox and reveal the mechanisms underlying viral immune evasion and disease progression. This research not only highlights potential therapeutic targets for intervention but also contributes to the development of effective antiviral strategies and vaccines for Mpox.
Results
Phylogenetic tree
To explore the substantial diversity of Mpox and its various genotyping strains, as well as the close relationship between Mpox’s original host species and the genus orthopoxvirus (OPV), we conducted a comprehensive phylogenetic analysis as the foundation of our study. Initially, we scrutinized the available sequences from current strains in 2022 (n = 225) to meticulously select samples with significant genetic distance and genotyping similarity (< 98%). Using a dissimilarity matrix, we constructed a comprehensive phylogenetic tree illustrating genetic distances within the OPV family and novel Mpox virus strains, with bootstrap values included to enhance the tree’s reliability (Fig. 1A). In selecting the viruses for analysis, we focused on strains with notable genetic relevance; however, we acknowledge that swinepox virus and sheeppox virus were not included in this study. This selection process was crucial for ensuring that our analysis accurately reflects the genetic diversity and relationships among the Mpox strains and related viruses within the OPV genus. Subsequent pairwise alignments of protein sequences highlighted a significant degree of similarity between previously identified Mpox virus proteins, specifically Zaire-96-I-16 (RefSeq: NC_003310.1), and recently discovered counterparts (OP382478.1) as shown in Fig. 1B. Our findings revealed a significant level of similarity, with 218 strains sharing identical sequences, while an additional five strains showed variation in a single nucleotide within the analyzed regions. To evaluate the differences among all analyzed strains in the complete concatenate, we identified a maximum variation of 59 nucleotides compared to strain Zaire-96-I-16. The resulting phylogenetic tree unveiled two prominent clades, with the first primarily consisting of African strains from 2006 to 2007 and 2016 to 2018, while the second clade included contemporary strains and African isolates from 2017 to 2018.
Phylogenetic analysis of orthopoxvirus (OPV). (A) Enlarged unrooted phylogenetic tree illustrating genetic distances within the OPV family. The UPGMA algorithm was used for phylogenetic tree construction. Old-world OPVs define species such as monkeypox (Mpox), vaccinia virus (VACV), and variola virus as monophyletic clades. (B) Global phylogeny of Mpox includes the current predominant 2022 Mpox outbreak variant, strain Zaire-96-I-16 (NC_003310.1), and Mpox virus strain OP382478.1. The red box highlights significant similarities between previously identified Mpox virus proteins and recently discovered counterparts.
HPI network construction
We established an extensive interactome by integrating data from 314 human proteins and 76 Mpox proteins, resulting in 1,120 high-confidence interactions (cutoff > 0.9) with Mpox proteins. The Supplementary File S1 shows the PHI network for orthopox viruses and human protein-protein interactions. This analysis has the potential to reveal novel drug targets for Mpox and host genes. Figure 2 illustrates these interactions, highlighting the significant interaction between viral proteins and specific host proteins. To design the HPI network, we integrated both host and viral protein sets to identify high-confidence interactions. We used degree centrality to measure the number of edges associated with each node in a network and ranked proteins based on their degree and closeness centrality to identify key hubs and bottleneck proteins. The 230 identified HPI proteins, along with module genes of functional significance, are presented in Supplementary File S1. This file outlines key HPI networks and protein-protein interactions between OPV and human proteins, providing crucial insights into the mechanisms of Mpox infection and highlighting potential therapeutic targets. Among the notable human proteins that interact with Mpox proteins, those with the highest degree include EGFR, TRAF6, UBC, SRC, CASP8, RB1, TBK1, IRF3, TNF, IKBKB, EIF2AK2, IKBKE, and BID. The Mpox protein exhibiting the highest degree centrality (> 15) interacts with proteins such as D11L, D9L, F7R, C6R, P2L, EGFR, F3L, C18L, G7R, J2L, TRAF6, UBC, and B12R (Fig. 2). Table 1 highlights the statistical interaction between these virulence factors and a substantial number of human proteins in the HPI network for orthopox viruses and human protein-protein interactions. As shown in Table 1, hub proteins such as EGFR are implicated in cell growth and survival, while TRAF6 is involved in the NF-kB signaling pathway, which is crucial for immune responses. Additionally, proteins like CASP8 and RB1 play vital roles in regulating apoptosis, underscoring their significance in controlling cell death and survival. These insights suggest that our findings primarily reflect mechanisms of HPI virulence. To advance our analysis, we initiated a detailed functional enrichment assessment of host proteins targeted by these virulence factors, concentrating on their functional roles and interactions within the HPI network.
Network of Mpox-human protein interactions. This visualization shows the intricate network of interactions between Mpox virus proteins (green) and human proteins (pink), connected by gray lines. The hub protein is labeled with a black star. Key biological processes in human proteins are highlighted within sub-networks, and HUB proteins, viral and human, are enlarged to emphasize their central roles. This overview of Mpox-HPI interactions provides insights into underlying mechanisms and potential therapeutic targets.
Construction and identification of WGCNA modules
We constructed a biological co-expression network to investigate the genes associated with Mpox disease severity. The gene expression dataset comprised 48 samples, including 24 healthy controls and 24 Mpox patients. Following data normalization and filtering using a standard deviation threshold greater than 0.5, we identified a dataset of 5,008 genes and 48 samples. This dataset provided the foundation for constructing the WGCNA. Using an optimal soft-power thresholding of β = 17, we achieved a scale-free network structure and identified 28 co-expression modules, one of which is the gray module. In WGCNA, genes that are not assigned to any specific module are grouped into the gray module. In our analysis, this module contained only two genes. Hierarchical clustering and a dynamic hybrid tree-cutting algorithm facilitated the extraction of modules, with each assigned a distinct color based on correlated gene expression patterns. After we computed module eigengenes and conducted hierarchical clustering to merge closely related modules (correlation ≥ 0.85; Fig. 3A), we finalized 16 modules. The cluster dendrogram after merging modules is shown in Fig. 3B. Module-trait analysis identified 7 modules significantly correlated (cor ≥ 0.5) with clinical traits, including Mpox and normal (Fig. 3C). ToppGene enrichment analysis highlighted three promising modules for further investigation, summarized in Supplementary File S1. The Black Module includes 10 nodes, the Dark Green Module contains 3 nodes, and the Salmon Module consists of 4 nodes. The integration of 230 previously identified HPI proteins with module genes highlighted functional overlaps and significance (Supplementary File S1).
Preprocessing of co-expression network reconstruction using WGCNA. (A) Detection of module eigengenes and merging of closely related modules. (B) Hierarchical clustering of 16 modules based on dissimilarity (1-TOM measure). Each module is depicted as a branch in the dendrogram, labeled with distinct colors using the WGCNA R package. (C) Visualization of module-trait relationships illustrating the correlations between clinical traits from Mpox samples and those from individuals vaccinated with inactivated Mpox samples, alongside their respective module eigengenes. The accompanying heatmap displays the correlation of host module eigengenes (rows) with viral measures (columns) across seven selected modules. (D) Heatmap of 19 common genes between HPI and WGCNA modules (fold changes > 1 or < − 1). This heatmap illustrates antiviral and proviral gene clusters responding to Mpox infection, emphasizing immune pathways and potential therapeutic targets. Genes associated with circulatory health, viral processes, and oxygen-glucose deprivation highlight host metabolic challenges, while connections to influenza pathways indicate shared viral mechanisms. Additionally, neutrophil activation underscores Mpox’s impact on innate immunity, enhancing our understanding of its immunopathogenic effects.
Antiviral and proviral signatures in Mpox transcriptomics
We categorized the identified genes into antiviral and proviral groups to identify potential druggable targets. This classification highlights potential therapeutic targets and key pathways to mitigate the virus’s effects on the host. We focused on 2358 genes that showed significant differences between case and control samples, prioritizing those with fold changes greater than 1 or less than − 1, resulting in a total of 28 genes (Supplementary File S1). Of these, 2 genes were up-regulated during infection, while 26 were down-regulated. The volcano plot extracted from DEG analysis is reported in Supplementary Fig. S1. The integration of these genes revealed 20 common genes shared between HPI and WGCNA gene modules, highlighting their dual significance in Mpox pathogenesis. These genes are involved in various pathways relevant to Mpox pathogenesis. Notably, they participate in the positive regulation of phospholipid transport, crucial for viral assembly and release, and respond to symbionts, indicating potential interactions with the host microbiome. Pathways related to dendritic spine development and glial cell migration suggest that Mpox may affect neurological functions and immune responses in the central nervous system (Fig. 3C). In Fig. 3D, we present a heatmap analysis of the common genes between HPI and WGCNA modules, highlighting differentially expressed genes (DEGs) in response to Mpox infection and distinct clusters of antiviral and proviral signatures. This expression profiling reveals critical immune pathways shaped by the virus-host interaction.
Prediction of transcription factors and kinases upstream cell signaling networks
To identify key upstream regulators in Mpox infection, we analyzed 28 DEGs associated with pro- and antiviral responses. Our analysis identified 11 kinases and 15 transcription factors with strong potential for drug repurposing based on activity scores. Table 2 outlines the significant interactions between these virulence factors and a substantial number of human proteins, organized by biological processes and Reactome signaling pathways. These regulators are vital for modulating the expression of DEGs linked to Mpox pathogenesis. Notably, we found that cytokine signaling in the immune system is significantly enriched, with 78 proteins identified (p = 8.02 × 10–35). The immune system pathway also showed a substantial involvement, with 114 proteins associated (p = 1.60 × 10–29). Interferon signaling was another key pathway, comprising 40 proteins (p = 2.29 × 10–23), highlighting its importance in the host response to Mpox infection. Additionally, pathways related to TLR4 signaling, both TRIF-mediated and MyD88-independent cascades, were enriched, featuring 26 proteins each (p = 3.80 × 10–20). The innate immune system also demonstrated a significant response, with 67 proteins involved (p = 2.89 × 10–18). Other notable processes included the apoptotic process, with 40 proteins identified (p = 2.05 × 10–15), and regulation of transcription (32 proteins, p = 2.06 × 10–10), reflecting the dynamic interplay between the virus and the host cellular machinery. These findings underscore the pivotal roles of transcription factors and kinases in orchestrating host responses against Mpox infection, providing valuable insights into potential therapeutic targets.
Drug repurposing against Mpox
This section explores the drug repurposing against Mpox infection, integrating insights from Direct-Acting Antivirals and Host-Targeting Antivirals… Computational algorithms were utilized to pinpoint viable drug targets for proviral and antiviral genes. Through this approach, we identified 26 genes deemed credible targets for Mpox treatment. To construct a disease module from transcription factor and kinase gene networks, we employed the Steiner tree algorithm, setting a hub penalty of zero and generating five Steiner trees. This module consisted of 50 nodes and 87 edges, which we analyzed using the Closeness Centrality algorithm to identify approved drugs suitable for repurposing. Our analysis yielded 16 potential drug targets, categorized into two groups: eight proviral genes (ESR2, ERK1, ERK2, P38, JNK1, CDK4, GSK3B, and STAT3) designated for inhibition and eight antiviral genes (IKKA, HDAC1, HIPK2, TF65, CSK21, HIPK2, ESR2, and GSK3B) designated for activation. Figure 4 highlights critical druggable genes implicated in Mpox infection, emphasizing distinct categories for targeted intervention. This comprehensive approach led to the identification of 90 FDA-approved drugs that effectively target druggable kinases (Fig. 4A) and transcription factors (Fig. 4B). Supplementary Table S1 lists FDA-approved and clinical trial host-targeting antiviral drugs for vaccinia and emerging Mpox. Collaboration with the FDA has been instrumental in facilitating this analysis. Table 3 shows targeted druggable genes in Mpox infection, detailing their functions, roles in the OPV replication cycle, potential inhibitors, and signaling pathways. These targeted druggable genes, derived from the IHP and WGCNA networks, are intricately linked to various signaling pathways, including NF-κB activation (IKKA and TF65), PI3K-Akt signaling (GSK3B and AKT1), and apoptosis regulation (HIPK2 and CSK21). Additionally, our analysis encompasses host-targeting antivirals, including experimental compounds that exhibit efficacy against Mpox infection. Inhibiting these genes through agents such as Niclosamide and Sunitinib may significantly reduce viral load and alleviate infection severity. Conversely, the antiviral genes play a pivotal role in activating immune responses, with critical involvement in NF-κB signaling (IKKA and TF65) and apoptosis (HIPK2). The signaling signatures associated with these genes elucidate their antiviral mechanisms, revealing drug effects that can range from activation to inhibition. Notably, compounds such as Estradiol and Medroxyprogesterone acetate are poised to specifically target antiviral genes, thereby enhancing host immune responses.
Drug repurposing discovery in Mpox infection. This figure illustrates the results of the Steiner tree analysis used to uncover molecular pathways connecting DEGs in Mpox infection, focusing on (A) kinases and (B) transcription factors. The analysis identifies critical nodes and edges within the kinase and transcription factors networks, highlighting the key signaling pathways disrupted by Mpox. The screening of repurposed drugs was conducted based on these identified biological processes and signaling pathways significantly impacted by the infection. This analysis provides insights into potential therapeutic strategies for managing Mpox infection through the repurposing of existing drugs. Proviral genes associated with Mpox infection are represented by red ovals, while antiviral genes are shown in green ovals. FDA-approved drugs targeting proviral genes are indicated by green diamonds, and those targeting antiviral genes are shown in red diamonds. Additionally, yellow diamonds represent drugs that target both antiviral and proviral pathways.
Pathway-based drug screening
To identify crucial target genes involved in Mpox infection, we conducted a thorough analysis of biological processes, signaling pathways, and functional predictions for gene sets encompassing both pro- and antiviral genes, upstream regulators, and druggable targets (p < 0.05). This allowed us to categorize Mpox-specific expressed genes based on GO terms and compare their functional annotations. Leveraging insights from drug repurposing efforts, we integrated target genes with enriched biological processes and signaling pathways influenced by Mpox. The final pro- and antiviral drug signatures are detailed in Table 3. Subsequent screening of repurposed drugs, guided by biological processes and the anti-proviral signature, identified eight potential proviral target genes (STAT3, AKT1, CDK4, CSK21, ERK2, ERK1, P38, and JNK1) susceptible to inhibition and two antiviral target genes (ESR2 and GSK3B) amenable to activation.
Functionality of targeted proviral and antiviral genes
In our drug screening process, we evaluated 16 potential drug targets based on their similar molecular functions. Figure 5 outlines the molecular mechanisms of proviral genes designated for inhibition, including ERβ (estrogen receptor beta), ERK1 and ERK2 (extracellular signal-regulated kinases), P38 (p38 MAP kinase), JNK1 (c-Jun N-terminal kinase), CDK4 (cyclin-dependent kinase 4), GSK3B (glycogen synthase kinase 3 beta), and STAT3 (signal transducer and activator of transcription 3). These genes play pivotal roles in signaling pathways such as AP-1, NF-κB, and apoptosis, enhancing viral replication and evading host immune responses. Specifically, ESR2, P38, and JNK1 are involved in proviral AP-1 signaling (Fig. 5A), while IKKA and TF65 activate antiviral NF-κB pathways and interferon (IFN) responses (Fig. 5B). Furthermore, STAT3, CDK4, and GSK3B participate in proviral PI3K/Akt and Wnt/β-catenin signaling, with ERK1 and ERK2 promoting MAPK/ERK1/2 pathways. CSK21 and HIPK2 are implicated in antiviral apoptosis and IFN signaling (Fig. 5C and D).
Mpox’s role in antiviral and proviral cell signaling regulation. (A) AP-1 signaling; Mpox activates the AP-1 signaling pathway through MAPK/MEK/ERK signaling (B14R, D3R, O1L) and c-Jun activation (B14R, B3R). Red arrows/boxes indicate proviral pathways/proteins, while green arrows/boxes highlight antiviral pathways/proteins and potential therapeutic targets. (B) NF-kB signaling; Mpox inhibits NF-kB signaling at various stages using proteins like J2L, B14R, B19R, A47R, C6R, and A52R (OPJ181), among others. (C) Apoptosis signaling; Mpox evades host apoptosis by inhibiting both extrinsic (death receptors: B12R, J2L) and intrinsic (mitochondrial: B12R, B19R, C7L) apoptotic pathways. (D) IFN signaling; Mpox counteracts the IFN pathway by inhibiting IFN induction (E9R, F3L), intercepting receptor binding (B16R, J1R), disrupting intracellular signaling (H1L, D8L), and reducing ISG expression (D11L, F3L).
Conversely, Fig. 6 summarizes the antiviral genes designated for activation, including IKKA (IκB kinase α), HDAC1 (histone deacetylase 1), HIPK2 (homeodomain-interacting protein kinase 2), TF65 (transcription factor 65), CSK21 (C-terminal Src kinase 21), ESR2, and GSK3B. Activation of these genes is crucial for an effective antiviral response against Mpox infection and is linked to the Wnt, AKT, and STAT3 pathways. These findings highlight the influence of CDK4/6 inhibitors on proviral signaling through the PI3K/AKT/mTOR pathway (Fig. 6A), Wnt pathway (Fig. 6B), and IL-6/STAT3 pathway (Fig. 6C).
Mpox manipulation and activation of proviral signaling via AKT, Wnt, and STAT3 signaling pathways. (A) Wnt signaling. Vaccinia virus protein A49 activates Wnt signaling by targeting the E3 ligase β-TrCP, inhibiting the β-catenin degradation complex. This leads to β-catenin accumulation and promotes TCF/LEF transcriptional activation. GSK3β inhibition by the Wnt pathway prevents β-catenin phosphorylation, allowing its cytoplasmic accumulation. Subsequently, β-catenin translocates into the nucleus to activate gene expression by binding TCF/LEF transcription factors. (B) AKT signaling. AKT phosphorylation and activation are facilitated by mammalian targets of rapamycin complex 2 (mTORC2) and phosphoinositide-dependent protein kinase 1 (PDK1 (C) STAT3 signaling. Mpox protein D3R (analogous to Vaccinia virus protein VGF) activates STAT3 function through regulated kinases like ERK, inducing non-canonical phosphorylation of STAT3 at S727 in a D3R(VGF)-dependent manner. Red arrows and boxes indicate proviral signaling pathways and proteins, while green arrows and boxes highlight antiviral signaling pathways, proteins, and potential therapeutic drugs targeting these pathways.
Discussion
Mpox, an OPV infection, has emerged as a significant public health concern following the discontinuation of routine smallpox vaccination, which has heightened susceptibility to related OPV infections and more virulent strains24. The recent global resurgence of Mpox underscores the critical need for comprehensive research into its genomics, proteomics, and molecular pathogenesis to develop effective antiviral therapies and vaccines against this re-emerging threat.
Understanding the molecular mechanisms behind Mpox pathogenesis is still a challenge, making it difficult to develop specific antiviral treatments and vaccines. Currently, most strategies rely on broad-spectrum approaches derived from knowledge of related OPVs, such as the vaccinia virus, because of their genetic similarities and shared pathogenic mechanisms of disease25. This study focuses on how the virulence factors of Mpox interact with host cellular pathways, helping the virus evade immune responses, manipulate host signaling, and facilitate viral replication. To explore these interactions, we applied comparative genomics and proteomics, using the Zaire-96-I-16 strain as a reference point to analyze the functional roles of Mpox-encoded proteins. By aligning and comparing these proteins with those from other OPV species, we can uncover insights into their evolutionary relationships and unique pathogenic mechanisms26,27. Network analyses, including HPI and WGCNA, facilitate the identification of critical proteins within essential signaling pathways, highlighting potential drug targets22,23. However, selecting appropriate target genes is complicated by the vast number of host genes and the associated risk of side effects28,29. Moreover, both strategies-targeting pathogen and host proteins offer distinct advantages and limitations, emphasizing the need for thoughtful consideration in developing therapeutic interventions. Conversely, drug repurposing offers a promising strategy to accelerate the development of effective therapies for Mpox30,31,32. By screening existing FDA-approved drugs against identified target genes and pathways, this study has highlighted compounds with potential antiviral activity33,34. Notably, drugs that target host kinases and hormonal receptors show efficacy in inhibiting viral replication and modulating host immune responses35,36. Our research combines knowledge-based30, signature-based31, and pathway/network-based32 methods, paving the way for potential drug repositioning to treat OPV infection.
We proposed three classes of drugs: kinase inhibitors, steroid hormone receptor agonists, and STAT3 inhibitors, including Niclosamide37,38. Supplementary Fig. S2 shows the Mpox life cycle, highlighting stages like entry, uncoating, genome replication, assembly, and release, each as potential antiviral drug targets, including VIG, Cidofovir, Rifampin, and Tecovirimat. Among these, the latest anti-poxvirus agents are kinase inhibitors such as ABL, EGFR, and CDK4/6 inhibitors, initially designed for cancer therapy39,40. These drugs inhibit both viral and host kinases, thereby reducing the spread and egress of poxviruses from infected cells36,39,41. Specifically, ABL inhibitors (imatinib and dasatinib) and the EGFR inhibitor (afatinib) have shown effectiveness against vaccinia virus replication in vitro and COVID-1942,43,44. Previous research has elucidated pathways targeted by dasatinib and afatinib, including PI3K/mTOR and HER/EGFR/ERBB signaling pathways45. However, our findings reveal a novel proviral pathway involving MAPK14 (P38) and the AP-1 pathway, presenting a new target for inhibiting viral replication46,47. Additionally, CDK4/6 inhibitors such as abemaciclib, palbociclib, and ribociclib have emerged as promising candidates against poxviruses36. This study specifically investigates how CDK4/6 inhibitors influence proviral signaling pathways, including PI3K/AKT/mTOR, Wnt, and IL-6/STAT3. These inhibitors could offer a comprehensive strategy for combating emerging viruses like Mpox48. This classification advances our understanding of Mpox pathogenesis and identifies gene targets with therapeutic potential, offering insights into the host’s immune resilience and the virus’s evasion strategies Furthermore, genes implicated in circulatory system development may influence cardiovascular health during infection. Connections to viral processes underscore the importance of these genes in the Mpox lifecycle, while their roles in the cellular response to oxygen-glucose deprivation indicate the metabolic challenges faced during infection. Links to influenza pathways suggest shared mechanisms with other viral infections, and the regulation of immune system processes highlights how Mpox manipulates host immunity. Lastly, the activation of neutrophils emphasizes the virus’s impact on innate immune responses. This analysis enhances our understanding of the immunopathogenic mechanisms of Mpox and identifies potential therapeutic targets for future research.
Despite limited research on hormonal and gender-specific effects related to Mpox and vaccinia infections, ERβ, has emerged as a key player in the immune response against viral infections, including poxviruses49,50. ERβ, a nuclear receptor that regulates transcription, has demonstrated inhibitory effects on proviral immune signaling pathways, including AKT and Wnt/β-catenin signaling51. Given its potential, leveraging ERβ agonists could provide a novel therapeutic avenue against poxviruses, particularly in the context of HPI.
This study highlights the importance of understanding gender-specific effects on Mpox infection, particularly the roles of ERβ and androgen receptors (ARs) in modulating host immune responses and viral pathogenesis. Targeting these receptors with specific agonists or antagonists presents novel therapeutic options for Mpox and related OPV infections52,53. The AR significantly influences Mpox54 by activating proviral pathways such as PI3K/AKT, Wnt, AP-1, and STAT3 signaling, while inhibiting antiviral pathways like NF-kB, interferon signaling, and apoptosis. Furthermore, the Vaccinia virus produces its steroid hormones using the A44L gene, which encodes the 3β-hydroxysteroid dehydrogenase enzyme (3β-HSD), contributing to the virus virulence by suppressing the host’s inflammatory response55,56. Furthermore, the Vaccinia virus produces its steroid hormones using the A44L gene, which encodes the 3β-HSD enzyme, contributing to viral virulence by suppressing the host’s inflammatory response57. Drugs targeting the AR may induce androgen signaling, but carry risks of proviral activity in Mpox infection58,59.
Previous studies have demonstrated the effectiveness of JAK-STAT3 inhibitors in reducing poxvirus replication, but this research identifies additional proviral signaling pathways inhibited by STAT3 inhibitors such as Niclosamide and cardiac glycosides like Digoxin, Digitoxin, and Ouabain60,61. Originally used to treat heart conditions, cardiac glycosides also modulate various signaling pathways, suppressing pathways like MAPK, PI3K/AKT/mTOR, and Wnt/β-catenin while promoting cell cycle control and apoptosis, making them promising candidates for OPV infections62,63.
Among the drug candidates, Niclosamide emerged as the most promising for Mpox inhibition. Originally developed as an anthelmintic, Niclosamide has gained attention for its antiviral properties64,65. Studies have shown its ability to drastically reduce vaccinia virus proliferation, even at low concentrations36. Niclosamide’s antiviral effects may be due to its capacity to activate antiviral pathways like apoptosis and autophagy, through the activation of caspase-3 and caspase-9, and suppression of Bcl-2. It also inhibits proviral pathways, including AKT, STAT3, and Wnt/β-catenin, by directly enhancing GSK-3B activity66.
Our study introduces a pathway-centered, network-based approach to drug repurposing for Mpox, contrasting with conventional methods focused on single-target affinity. Amar Ajmal’s team primarily used single-target, structure-based docking to identify inhibitors for Mpox’s thymidylate kinase, centering on individual binding affinities without a broader disease context67. Our approach combines HPI networks with WGCNA to prioritize key gene modules and high-confidence interactions, providing a more comprehensive view of viral-host dynamics.
Kang Tang et al. employed a network-based drug repurposing approach using the REMAP model, which predicts drug-target interactions based on structural similarity. However, this similarity-driven method may lead to broader, less disease-specific predictions, potentially limiting its effectiveness for targeting Mpox-specific pathways68. In contrast, we target highly expressed proteins and Mpox-relevant pathways identified by overlapping WGCNA and HPI data. Our use of the MuST algorithm further prioritizes drugs based on their influence on key pathways rather than binding affinity alone, leading to targeted candidates like kinase inhibitors and Niclosamide30. This pathway-centric, multi-target method refines therapeutic discovery, aligning with Mpox’s complex host interactions and offering a strategic route for developing effective treatments.
Despite these findings, several limitations remain. While computational models and bioinformatics tools provide valuable insights, their predictions must be validated through experimental and clinical data. Additionally, the genetic diversity of Mpox and its impact on virulence require further investigation through enhanced genomic surveillance. Future research should focus on preclinical and clinical validation of the identified drug candidates, alongside studies on gender-specific effects in Mpox infection to support personalized treatments69. In conclusion, this study emphasizes the need for further research into Mpox genomics and host interactions to develop effective treatments. By constructing protein-host interaction networks, the study identified key viral and host proteins, prioritizing upstream genes to minimize side effects. Through a drug repurposing pipeline, the study highlighted promising therapeutic candidates, with Niclosamide demonstrating significant anti-pox activity. These findings contribute to the global effort to combat OPV infections and improve infectious disease treatment strategies.
Materials and methods
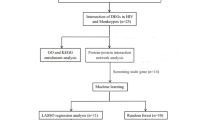
The detailed computational pipeline and subsequent functional analysis of the predicted HPI are illustrated in Supplementary Fig. S3. Our study employs an integrated approach, utilizing HPI and WGCNA, to unravel the intricate model of Mpox pathogenesis and identify druggable genes. The final steps involve screening target genes and exploring drug-based signaling pathways. The workflow delineates crucial stages, from deciphering host gene modules influenced by Mpox proteins to identifying potential drugs such as kinase inhibitors and Niclosamide.
Data acquisition and integration
Detailed information on all in silico data is provided in Supplementary Table S2. In detail, the HPI networks for this study were compiled from various sources, including orthopox virus data, along with data from the Virus String70 server and the IntAct database71. In the following analysis, orthopox proteins with high similarity scores to the primary Mpox strains (MP-ZAI-96 and OP382478.1) were selected. This process resulted in a dataset of 435 high-confidence virus-host interactions involving 76 orthopox viruses and 314 host genes. This compilation resulted in a dataset of 435 high-confidence virus-host interactions involving 75 orthopox viruses and 305 host genes. For the WGCNA, transcriptomics data for Mpox and Vaccinia virus (GSE24125) from the Gene Expression Omnibus (GEO) database were utilized, encompassing 190 samples across platforms GPL10912, GPL10913, and GPL1091472. Focusing on GPL10912, which comprised 48 equally divided samples of killed Mpox virus and Mpox virus, the dataset underwent normalization in R.
Data integration
Here, we integrated protein and genome data from diverse sources to reduce false-positive predictions and false discovery rates. Using five distinct OMICS-basthods, we combined HPI data with WGCNA results to identify common genes with antiviral and proviral signatures, offering insights into HPI73.
Homology and phylogenetic tree
For the construction of a phylogenetic tree, we systematically retrieved pox-related sequences from the NCBI nucleotide database. We performed a ClustalW multiple sequence alignment using the MEGA11 software (version 11.00)74. Additionally, we used the Unweighted Pair Group Method with Arithmetic Mean (UPGMA) algorithm for phylogenetic tree construction and set the bootstrap replication parameter to 50075.
HPI network construction
Here, we established HPI networks by delineating a human protein-protein interaction network that incorporates interactions with pox viral proteins, facilitated by the Cytoscape String App76. We assessed node connections through degree centrality to visualize the HPI network using Cytoscape (version 3.8.2). We compiled virus-host interaction data from multiple sources, including previous orthopox studies, the VIRUS STRING server, and IntAct database77. Utilizing Cytoscape, networks were generated for each data source, transformed into a protein-protein network format, and merged to create a consolidated HPI network related to Mpox viruses. We constructed a human protein-protein interaction network with pox viral proteins using the Cytoscape software at a confidence score of 0.477.
WGCNA analysis
In the process of constructing the co-expression network, we employed the WGCNA package (version 1.60) in R to identify key modules on the carefully filtered dataset. Pairwise gene correlations were determined using Bicor, and a judiciously chosen optimal power (β) of 0.9 was applied to establish a scale-free network. Fine-tuning parameters included specifying a minimum module size of 10, and the network type was set to be signed, reflecting the directionality of interactions. The identification of modules was achieved through the dynamic tree-cutting method, with a focus on merging closely correlated modules exhibiting a correlation greater than 0.85. A subsequent module-trait analysis was conducted, selecting modules with a correlation value of at least 0.578,79. The selected WGCNA module information for Mpox infection is sorted in Supplementary File S1.
Functional enrichment analysis
For functional enrichment analysis, we employed the ToppGene tool, focusing on biological processes, pathways, and disease profiles with a significance threshold (adjusted p-value < 0.05)80. To validate the correlation between the HPI network and Mpox-associated biological annotations, we conducted a comprehensive enrichment analysis81. To assess statistical significance in biological processes and Reactome signaling pathways, we utilized the DAVID server with a stringent Benjamini-Hochberg FDR threshold (< 0.001)77. Visualization of enrichment analysis outcomes was achieved through Cytoscape.
Antiviral and proviral signatures derived from post-Mpox infection
We explored the transcriptomic dynamics in response to Mpox infection to identify antiviral and proviral signatures, focusing on DEGs and key modules through WGCNA. Our selection criteria prioritized genes that either reversed or intensified the infection signature, focusing on the top 28 genes with significant differential expression (log2FC > 1 and adjusted p < 0.05). Additionally, 19 genes common to both HPI and WGCNA modules were included. Thoughtfully categorized into proviral and antiviral signatures82, the resulting heatmap, visualized using the heatmap package for R statistical software (version 3.3.3) as previously described77, illuminated genes countering or intensifying the infection signature.
Transcriptomic and upstream signaling networks
To unravel the intricacies of gene expression and upstream regulatory networks, we employed a multi-faceted approach, combining global mRNA-level profiling with advanced methodologies such as eXpression2Kinases (X2K) and ChEA. The aim was to gain insights into the regulatory landscape by identifying transcription factors and protein kinases associated with specific cellular conditions83. The X2K algorithm predicted upstream cell signaling pathways by identifying enriched transcription factors from DEGs, establishing connections through protein-protein interactions, and conducting kinase enrichment analysis on the subnetwork.
Gene druggability and repurposing screening
To unravel disease pathways and mechanisms, we employed the multi-Steiner trees (MuST) method. A comparative analysis was conducted with FDA-approved antiviral drugs (Supplementary Tables S1), encompassing direct-acting antivirals for the OPV replication cycle and host-targeting antiviral agents9. This meticulous approach facilitated the selection of drugs closely linked to nodes in the disease module, positioning them as robust candidates for repurposing84.
Pathway-based drug screening
To comprehensively present our findings, we integrated the identified antiviral and proviral signatures, gene druggability results, and drug-based screening outcomes. Cytoscape was employed to merge and visualize these data sets, facilitating a holistic understanding of the intricate interactions between Mpox and the host cellular environment.
Statistical analysis
Statistical analyses were conducted using “R” software (version 3.3.3). Univariate and stepwise multivariate logistic regression was employed to identify independent factors associated with Mpox diagnosis, incorporating hub genes from the selected module and clinical risk factors. Phylogenetic trees were constructed using MEGA11. A significance level of p < 0.05 was considered statistically significant. All graphics were created using BioRender.com.
Data availability
The datasets analyzed during the current study WGCNA using the GSE152418 dataset which, is available in the GEO is a repository, [https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE24125]. The data presented in the tables of this article have been extracted from previously published articles and studies, and all relevant references for these data are cited in the text of the article. These data are publicly available and can be accessed through the referenced sources.
References
Haque, M. A., Halder, A. S., Hossain, M. J. & Islam, M. R. Prediction of potential public health risk of the recent multicountry monkeypox outbreak: an update after the end declaration of global public health emergency. Health Sci. Rep. 7, e2136 (2024).
Marziano, V., Guzzetta, G., Longini, I. & Merler, S. Epidemiologic quantities for Monkeypox Virus Clade I from historical data with implications for current outbreaks, Democratic Republic of the Congo. Emerg. Infect. Dis. 30, 2042–2046. https://doi.org/10.3201/eid3010.240665 (2024).
Shchelkunov, S. N. et al. Human monkeypox and smallpox viruses: genomic comparison. FEBS Lett. 509, 66–70. https://doi.org/10.1016/s0014-5793(01)03144-1 (2001).
Shchelkunov, S. N. et al. The genomic sequence analysis of the left and right species-specific terminal region of a cowpox virus strain reveals unique sequences and a cluster of intact ORFs for immunomodulatory and host range proteins. Virology. 243, 432–460. https://doi.org/10.1006/viro.1998.9039 (1998).
Shchelkunov, S. N. et al. Comparison of the genetic maps of variola and vaccinia viruses. FEBS Lett. 327, 321–324. https://doi.org/10.1016/0014-5793(93)81013-p (1993).
Cesur, M. F., Durmuş, S. Systems Biology Modeling to Study Pathogen–Host Interactions. In: Medina, C., López-Baena, F. (eds) Host-Pathogen Interactions. Methods in Molecular Biology, vol 1734;. Humana Press, New York, NY (2018). https://doi.org/10.1007/978-1-4939-7604-1_10
Paul, D., Saha, S., Basu, S. & Chakraborti, T. Computational analysis of pathogen-host interactome for fast and low-risk in-silico drug repurposing in emerging viral threats like Mpox. Sci. Rep. 14, 18736. https://doi.org/10.1038/s41598-024-69617-8 (2024).
Kumar, R. et al. Monkeypox virus: phylogenomics, host–pathogen interactome and mutational cascade. Microb. Genomics. 9, 000987 (2023).
Prichard, M. N. & Kern, E. R. Orthopoxvirus targets for the development of new antiviral agents. Antiviral Res. 94, 111–125 (2012).
Ahmed, S. F., Sohail, M. S., Quadeer, A. A. & McKay, M. R. Vaccinia-virus-based vaccines are expected to elicit highly cross-reactive immunity to the 2022 monkeypox virus. Viruses. 14, 1960 (2022).
Karami, H. et al. Weighted Gene Co-expression Network Analysis Combined with Machine Learning Validation To Identify Key Modules and hub genes Associated with SARS-CoV-2 infection. J. Clin. Med. 10 https://doi.org/10.3390/jcm10163567 (2021).
van Dam, S., Võsa, U., van der Graaf, A., Franke, L. & de Magalhães, J. P. Gene co-expression analysis for functional classification and gene-disease predictions. Brief. Bioinform. 19, 575–592. https://doi.org/10.1093/bib/bbw139 (2018).
Li, Q. et al. Enhancing Gene Co-expression Network Inference for the Malaria Parasite Plasmodium Falciparum. Genes (Basel). 15 https://doi.org/10.3390/genes15060685 (2024).
Alarabi, A. B., Mohsen, A., Mizuguchi, K., Alshbool, F. Z. & Khasawneh, F. T. Co-expression analysis to identify key modules and hub genes associated with COVID-19 in platelets. BMC Med. Genomics. 15, 83. https://doi.org/10.1186/s12920-022-01222-y (2022).
Ma, Z. et al. Weighted gene co-expression network analysis identified underlying hub genes and mechanisms in the occurrence and development of viral myocarditis. Ann. Transl Med. 8, 1348. https://doi.org/10.21037/atm-20-3337 (2020).
Bai, R. et al. Exploring the biological function of immune cell-related genes in human immunodeficiency virus (HIV)-1 infection based on weighted gene co-expression network analysis (WGCNA). BMC Med. Genom. 15, 200. https://doi.org/10.1186/s12920-022-01357-y (2022).
He, D., Liu, Z. P., Honda, M., Kaneko, S. & Chen, L. Coexpression network analysis in chronic hepatitis B and C hepatic lesions reveals distinct patterns of disease progression to hepatocellular carcinoma. J. Mol. Cell. Biol. 4, 140–152. https://doi.org/10.1093/jmcb/mjs011 (2012).
Liu, C., Dai, Q., Ding, Q., Wei, M. & Kong, X. Identification of key genes in hepatitis B associated hepatocellular carcinoma based on WGCNA. Infect. Agent Cancer. 16, 18. https://doi.org/10.1186/s13027-021-00357-4 (2021).
Marchi, E. et al. Defining the key intrahepatic gene networks in HCV infection driven by sex. Gut. 72, 984–994. https://doi.org/10.1136/gutjnl-2021-326314 (2023).
Hasankhani, A. et al. Differential Co-expression Network Analysis reveals key hub-high traffic genes as potential therapeutic targets for COVID-19 pandemic. Front. Immunol. 12, 789317. https://doi.org/10.3389/fimmu.2021.789317 (2021).
Michlmayr, D. et al. Comprehensive Immunoprofiling of Pediatric Zika reveals Key Role for monocytes in the Acute phase and no effect of prior dengue virus infection. Cell. Rep. 31, 107569. https://doi.org/10.1016/j.celrep.2020.107569 (2020).
Tang, Z. et al. A bioinformatics approach to systematically analyze the molecular patterns of monkeypox virus-host cell interactions. Heliyon. 10, e30483. https://doi.org/10.1016/j.heliyon.2024.e30483 (2024).
Loganathan, T. et al. Expression analysis and mapping of viral-host protein interactions of Poxviridae suggests a lead candidate molecule targeting Mpox. BMC Infect. Dis. 24, 483. https://doi.org/10.1186/s12879-024-09332-x (2024).
Gong, Q., Wang, C., Chuai, X. & Chiu, S. Monkeypox virus: a re-emergent threat to humans. Virologica Sinica, 37(4), 477–482 (2022). https://doi.org/10.1016/j.virs.2022.07.006
Manes, N. P. et al. Comparative proteomics of human monkeypox and vaccinia intracellular mature and extracellular enveloped virions. J. Proteome Res. 7, 960–968 (2008).
Giorgi, F. M., Pozzobon, D., Di Meglio, A. & Mercatelli, D. Genomic and transcriptomic analysis of the recent Mpox outbreak. Vaccine. 42 (7), 1841–1849. https://doi.org/10.1016/j.vaccine.2023.12.086 (2024).
Clemente, B. et al. Straight to the point: targeted mRNA-delivery to immune cells for improved vaccine design. Front. Immunol. 14 https://doi.org/10.1016/j.vaccine.2023.12.086/fimmu.2023.1294929 (2023).
Nithya, C., Kiran, M. & Nagarajaram, H. A. Comparative analysis of Pure Hubs and Pure Bottlenecks in Human Protein-protein Interaction Networks. bioRxiv, 2004. 2006.438602 (2021). (2021).
Sadegh, S. et al. Exploring the SARS-CoV-2 virus-host-drug interactome for drug repurposing. Nat. Commun. 11, 3518 (2020).
Tang, K. et al. Network-based approach for drug repurposing against mpox. Int. J. Biol. Macromol. 270, 132468. https://doi.org/10.1016/j.ijbiomac.2024.132468 (2024).
Saha, S., Chatterjee, P., Nasipuri, M., Basu, S. & Chakraborti, T. Computational drug repurposing for viral infectious diseases: a case study on monkeypox. Brief. Funct. Genomics. 23, 570–578. https://doi.org/10.1093/bfgp/elad058 (2024).
Ajmal, A. et al. Computer-assisted drug repurposing for thymidylate kinase drug target in monkeypox virus. Front. Cell. Infect. Microbiol. 13, 1159389. https://doi.org/10.3389/fcimb.2023.1159389 (2023).
Dutt, M. et al. Drug repurposing for Mpox: Discovery of small molecules as potential inhibitors against DNA-dependent RNA polymerase using molecular modeling approach. J. Cell. Biochem. 124, 701–715. https://doi.org/10.1002/jcb.30397 (2023).
Abduljalil, J. M. & Elfiky, A. A. Repurposing antiviral drugs against the human monkeypox virus DNA-dependent RNA polymerase; in silico perspective. J. Infect. 85, 702–769. https://doi.org/10.1016/j.jinf.2022.09.002 (2022).
Hossain, F. M. A. et al. A review on computational studies and bioinformatics analysis of potential drugs against monkeypox virus. J. Biomol. Struct. Dyn. 42, 6091–6107. https://doi.org/10.1080/07391102.2023.2231542 (2024).
Peng, C. et al. Identification of Vaccinia virus inhibitors and cellular functions necessary for efficient viral replication by screening bioactives and FDA-approved drugs. Vaccines. 8, 401 (2020).
Goebel, G. L., Qiu, X. & Wu, P. Kinase-targeting small-molecule inhibitors and emerging bifunctional molecules. Trends Pharmacol Sci. 43(10), 866–881 (2022). https://doi.org/10.1016/j.tips.2022.04.006
Cairns, D. M. et al. Efficacy of Niclosamide vs Placebo in SARS-CoV-2 respiratory viral clearance, viral shedding, and duration of symptoms among patients with mild to moderate COVID-19: a phase 2 Randomized Clinical Trial. JAMA Netw. Open. 5, e2144942–e2144942. https://doi.org/10.1001/jamanetworkopen.2021.44942 (2022).
García-Cárceles, J., Caballero, E., Gil, C. & Martínez, A. Kinase inhibitors as underexplored antiviral agents. J. Med. Chem. 65, 935–954. https://doi.org/10.1021/acs.jmedchem.1c00302 (2022).
Fassl, A., Geng, Y. & Sicinski, P. CDK4 and CDK6 kinases: from basic science to cancer therapy. Science. 375, eabc1495. https://doi.org/10.1126/science.abc1495 (2022).
Schor, S. & Einav, S. Repurposing of kinase inhibitors as broad-spectrum antiviral drugs. DNA Cell. Biol. 37, 63–69. https://doi.org/10.1089/dna.2017.4033 (2018).
Weisberg, E. et al. Repurposing of kinase inhibitors for treatment of COVID-19. Pharm. Res. 37, 1–29 (2020).
Naik, R. R., Shakya, A. K., Aladwan, S. M. & El-Tanani, M. Kinase inhibitors as potential therapeutic agents in the treatment of COVID-19. Front. Pharmacol. 13, 806568. https://doi.org/10.3389/fphar.2022.806568 (2022).
Shin, H. J. et al. SARS-CoV-2 aberrantly elevates mitochondrial bioenergetics to induce robust virus propagation. Signal. Transduct. Target. Ther. 9, 125. https://doi.org/10.1038/s41392-024-01836-x (2024).
Peng, C. et al. Identification of Vaccinia Virus inhibitors and Cellular functions necessary for efficient viral replication by Screening Bioactives and FDA-Approved drugs. Vaccines (Basel). 8 https://doi.org/10.3390/vaccines8030401 (2020).
Khatri, A., Wang, J. & Pendergast, A. M. Multifunctional abl kinases in health and disease. J. Cell Sci. 129, 9–16 (2016).
Börgeling, Y. et al. Inhibition of p38 mitogen-activated protein kinase impairs influenza virus-induced primary and secondary host gene responses and protects mice from lethal H5N1 infection. J. Biol. Chem. 289, 13–27. https://doi.org/10.1074/jbc.M113.469239 (2014).
Xu, X., Zhu, Y., Yue, C., Yang, Q. & Zhang, Z. Comprehensive Bioinformatics Analysis Combined with wet-lab experiments to find Target proteins of Chinese Medicine Monomer. Molecules. 27, 6105 (2022).
Abramenko, N. et al. Estrogen Receptor Modulators in viral infections such as SARS-CoV-2: therapeutic consequences. Int. J. Mol. Sci. 22 https://doi.org/10.3390/ijms22126551 (2021).
Harding, A. T. & Heaton, N. S. The impact of Estrogens and their receptors on immunity and inflammation during infection. Cancers (Basel). 14 https://doi.org/10.3390/cancers14040909 (2022).
Mal, R. et al. Estrogen receptor beta (ERβ): a ligand activated tumor suppressor. Front. Oncol. 10, 587386 (2020).
Indukuri, R. et al. Genome-wide estrogen receptor β chromatin binding in human colon cancer cells reveals its tumor suppressor activity. Int. J. Cancer. 149, 692–706 (2021).
Alfredo, C. A. et al. Effect of Norelgestromin and Ethinylestradiol in Transdermal patches on the clinical outcomes and biochemical parameters of COVID-19 patients: a clinical Trial Pilot Study. Pharmaceuticals. 15, 757 (2022).
Henze, L., Schwinge, D. & Schramm, C. The effects of androgens on T cells: clues to female predominance in autoimmune liver diseases? Front. Immunol. 11, 1567 (2020).
Reading, P. C., Moore, J. B. & Smith, G. L. Steroid hormone synthesis by Vaccinia virus suppresses the inflammatory response to infection. J. Exp. Med. 197, 1269–1278. https://doi.org/10.1084/jem.20022201 (2003).
Kaynarcalidan, O., Moreno Mascaraque, S. & Drexler, I. Vaccinia Virus: from crude smallpox vaccines to elaborate viral Vector Vaccine Design. Biomedicines. 9 https://doi.org/10.3390/biomedicines9121780 (2021).
Holgado, M. P. et al. Deletion of A44L, A46R and C12L Vaccinia Virus genes from the MVA Genome Improved the Vector Immunogenicity by modifying the Innate Immune Response Generating enhanced and optimized specific T-Cell responses. Viruses. 8 https://doi.org/10.3390/v8050139 (2016).
Bereshchenko, O., Bruscoli, S. & Riccardi, C. Glucocorticoids, sex hormones, and immunity. Front. Immunol. 9, 1332 (2018).
Kaikkonen, S., Paakinaho, V., Sutinen, P., Levonen, A. L. & Palvimo, J. J. Prostaglandin 15d-PGJ2 inhibits androgen receptor signaling in prostate cancer cells. Mol. Endocrinol. 27, 212–223 (2013).
Quan, Y., Xu, H., Han, Y., Mesplède, T. & Wainberg, M. A. JAK-STAT signaling pathways and inhibitors affect reversion of envelope-mutated HIV-1. J. Virol. 91 https://doi.org/10.1128/jvi.00075-17 (2017).
Mahjoor, M. et al. Double-edged sword of JAK/STAT signaling pathway in viral infections: novel insights into virotherapy. Cell. Communication Signal. 21, 272. https://doi.org/10.1186/s12964-023-01240-y (2023).
Škubník, J., Pavlíčková, V. & Rimpelová, S. Cardiac glycosides as immune system modulators. Biomolecules. 11, 659 (2021).
Wang, J. et al. Niclosamide-induced wnt signaling inhibition in colorectal cancer is mediated by autophagy. Biochem. J. 476, 535–546 (2019).
Wang, Z. et al. Niclosamide as a Promising Therapeutic Player in Human Cancer and Other diseases. Int. J. Mol. Sci. 23, 16116 (2022).
Singh, S. et al. Niclosamide—A promising treatment for COVID-19. Br. J. Pharmacol. 179, 3250–3267 (2022).
Huang, F. L. et al. Niclosamide suppresses T–cell acute lymphoblastic leukemia growth through activation of apoptosis and autophagy. Oncol. Rep. 47, 1–10 (2022).
Ajmal, A. et al. Computer-assisted drug repurposing for thymidylate kinase drug target in monkeypox virus. Front. Cell. Infect. Microbiol. 13, 1159389 (2023).
Tang, K. et al. Network-based approach for drug repurposing against mpox. Int. J. Biol. Macromol. 270, 132468 (2024).
Lu, J. et al. Mpox (formerly monkeypox): pathogenesis, prevention, and treatment. Signal. Transduct. Target. Ther. 8, 458. https://doi.org/10.1038/s41392-023-01675-2 (2023).
Cook, H. V., Doncheva, N. T., Szklarczyk, D., Von Mering, C. & Jensen, L. J. Viruses. STRING: a virus-host protein-protein interaction database. Viruses. 10, 519 (2018).
Del Toro, N. et al. The IntAct database: efficient access to fine-grained molecular interaction data. Nucleic Acids Res. 50, D648–D653 (2022).
Rubins, K. H., Hensley, L. E., Relman, D. A. & Brown, P. O. Stunned silence: gene expression programs in human cells infected with monkeypox or vaccinia virus. PloS One. 6, e15615 (2011).
Kori, M., Turanli, B. & Arga, K. Y. Drug repositioning via host-pathogen protein-protein interactions for the treatment of cervical cancer. Front. Oncol. 13, 1096081 (2023).
Tamura, K., Stecher, G. & Kumar, S. MEGA11: Molecular Evolutionary Genetics Analysis Version 11. Mol. Biol. Evol. 38, 3022–3027. https://doi.org/10.1093/molbev/msab120 (2021).
Li, Y. & Xu, L. Unweighted Multiple Group Method with Arithmetic Mean. (2010).
Smoot, M. E., Ono, K., Ruscheinski, J., Wang, P. L. & Ideker, T. Cytoscape 2.8: new features for data integration and network visualization. Bioinformatics. 27, 431–432 (2011).
Fu, S. et al. Novel pathogenic CERKL variant in Iranian familial with inherited retinal dystrophies: genotype-phenotype correlation. 3 Biotech. 13, 166. https://doi.org/10.1007/s13205-023-03535-w (2023).
Langfelder, P. & Horvath, S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinform. 9, 1–13 (2008).
Maghsoudloo, M., Azimzadeh Jamalkandi, S., Najafi, A. & Masoudi-Nejad, A. Identification of biomarkers in common chronic lung diseases by co-expression networks and drug-target interactions analysis. Mol. Med. 26, 1–19 (2020).
Chen, J., Bardes, E. E., Aronow, B. J. & Jegga, A. G. ToppGene suite for gene list enrichment analysis and candidate gene prioritization. Nucleic Acids Res. 37, W305–W311 (2009).
Reimand, J. et al. Pathway enrichment analysis and visualization of omics data using g: Profiler, GSEA, Cytoscape and EnrichmentMap. Nat. Protoc. 14, 482–517 (2019).
Josset, L. et al. Gene expression signature-based screening identifies new broadly effective influenza a antivirals. PloS One. 5, e13169 (2010).
Keenan, A. B. et al. ChEA3: transcription factor enrichment analysis by orthogonal omics integration. Nucleic Acids Res. 47, W212–W224 (2019).
Sadegh, S. et al. Network medicine for disease module identification and drug repurposing with the NeDRex platform. Nat. Commun. 12, 6848 (2021).
Chen, N. et al. Virulence differences between monkeypox virus isolates from West Africa and the Congo basin. Virology. 340, 46–63. https://doi.org/10.1016/j.virol.2005.05.030 (2005).
Domán, M., Fehér, E., Varga-Kugler, R., Jakab, F. & Bányai, K. Animal models used in Monkeypox Research. Microorganisms. 10, 2192 (2022).
Li, H. et al. The land-scape of immune response to monkeypox virus. EBioMedicine 87, (2023).
Xiong, C. et al. Monkeypox virus 2022, gene heterogeneity and protein polymorphism. Signal. Transduct. Target. Ther. 8 (1), 278. https://doi.org/10.1038/s41392-023-01540-2 (2023).
Oda, K., Matsuoka, Y., Funahashi, A. & Kitano, H. A comprehensive pathway map of epidermal growth factor receptor signaling. Mol. Syst. Biol. 1, 20050010 (2005).
Li, Y. et al. Monkeypox virus 2022, gene heterogeneity and protein polymorphism. Signal. Transduct. Target. Ther. 8, 278. https://doi.org/10.1038/s41392-023-01540-2 (2023).
Forni, D. et al. Whole-genome sequencing of hMPXV1 in five Italian cases confirms the occurrence of the predominant epidemic lineage. J. Med. Virol. 95, e28493 (2023).
Walsh, M. C., Lee, J. & Choi, Y. Tumor necrosis factor receptor-associated factor 6 (TRAF 6) regulation of development, function, and homeostasis of the immune system. Immunol. Rev. 266, 72–92 (2015).
Rajsbaum, R. et al. Unanchored K48-linked polyubiquitin synthesized by the E3-ubiquitin ligase TRIM6 stimulates the interferon-IKKε kinase-mediated antiviral response. Immunity. 40, 880–895 (2014).
Acknowledgements
This work was supported by the Talent Scientific Research Project of Zhejiang Shuren University under Grant [numbers KXJ1723104, 2021]. The authors extend their gratitude to Tehran University for their invaluable support and for providing the computational resources necessary for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization, S.I. and S.A.; Methodology, M.A., Z.A., M.M. and Z.T.; Formal Analysis, Investigation, S.I. and M.M.; Resources, I.S.M. and S.A.; Data Curation, S.I. and S.A.; Writing- Original Draft Preparation, S.I. and S.A.; Writing – Review & Editing, S.I. and S.A.; Visualization, M.M. and M.A.; Supervision, S.I. and S.A.; Project Administration, I.S.M. and Z.A.; Funding Acquisition, S.I. All authors read the manuscript and gave the final approval for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Imani, S., Aminnezhad, S., Alikarami, M. et al. Exploration of drug repurposing for Mpox outbreaks targeting gene signatures and host-pathogen interactions. Sci Rep 14, 29436 (2024). https://doi.org/10.1038/s41598-024-79897-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-024-79897-9
Keywords
This article is cited by
-
Monkey pox (Mpox): pathogenesis, genetic shifts, vaccination strategies and clinical insights
Archives of Microbiology (2026)
-
Advances in the Management of MPOX Infection: Therapeutic and Vaccination Perspectives
Current Treatment Options in Infectious Diseases (2025)
-
Potent neutralization by antibodies targeting the MPXV A28 protein
Nature Communications (2025)