Abstract
Coronavirus disease (COVID-19) is a heterogeneous infectious disease caused by the novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The distinctive features of COVID-19 infection encompass a clinical spectrum ranging from asymptomatic forms to severe illness involving diverse underlying pathophysiological processes such as hyperinflammation, endothelial dysfunction, thrombotic microangiopathies, and multiple organ failure. However, the host responses to COVID-19, including systemic inflammation and immunity against SARS-CoV-2, remain largely undefined across different disease states. Here, we performed global transcriptome profiling of 228 peripheral blood samples of COVID-19 patients with different clinical manifestations and subsequent clustering using an unsupervised algorithm. We identified various transcriptomic clusters and globally dysregulated immune-related pathways, leading to distinct host inflammatory cytokine profiles in severe and critical SARS-CoV-2 infected patients. This underscores the association between COVID-19 pathogenesis and excessive cytokine release. Additionally, our results reveal variances in circulating cell populations and the activation of apoptosis and the p53 signaling pathway in lymphocytes induced by SARS-CoV-2 infection. The transcriptome dataset of COVID-19 patients with diverse clinical presentations offers valuable insights into molecular mechanisms and may inform clinical decisions on anti-inflammatory therapies.
Similar content being viewed by others
Introduction
Coronavirus disease (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This highly contagious respiratory illness, first identified in late 2019 in Wuhan, China, spread worldwide and rapidly evolved into a global pandemic. Indeed, the ongoing pandemic has sparked global attention due to its impact on public health, economies, and daily life1. Interestingly, the clinical outcomes of COVID-19 is highly variable ranging from asymptomatic or mild flu-like symptoms to severe pneumonia, and acute respiratory distress syndrome, requiring intensive care2,3. Multiple host factors, including genetics4 epigenetics5 gene expression6 advanced age, gender and multiple pre-existing health conditions7,8,9 are implicated in influencing individual response to SARS-CoV-2. Thus, these factors contribute to disease susceptibility, severity, and potential treatment approaches. Since the onset of the pandemic, there has been remarkable and global efforts to advance our understanding of COVID-19 and the interaction between the virus and the human host, which led to the successful development and implementation of vaccination strategies, aimed at controlling the spread of the disease10,11.
The host immunological response to SARS-CoV-2 infection is still not well understood despite these efforts. Other coronaviruses are known to trigger an exuberant host inflammatory response, ultimately resulting in severe lung injury on account of cytokine storm that12,13,14,15,16,17 also appears to be the common cause of mortality in COVID-1918,19. Recent transcriptomic studies from patients with COVID-19 demonstrated pro-inflammatory host cytokine profile20, a shift in immune cell populations along with cytokine storm and adaptive immune dysfunction21. Other studies have identified circulating RNA biomarkers22 and highlighted the functional pathways involved in SARS-CoV-2 pathogenesis23. Additional, studies have revealed that severe and critical cases of COVID-19 exhibit elevated plasma levels of inflammatory cytokines such as IL2, IL6, IL7, IL10 and TNFα in comparison to mild cases24,25 suggesting the crucial role these cytokines play in COVID-19 progression. Postmortem findings from COVID-19 lung biopsies revealed interstitial mononuclear inflammatory infiltrates in lung tissues26. Elucidating the underlying molecular mechanisms of these pathophysiologic differences that contribute to the clinical sequel of SARS-CoV-2 infection is important to predict disease outcome and tailor treatment strategies. Additionally, accumulated SARS-CoV-2 mutations in the spike protein resulted in the emergence of variants, such as Alpha, Delta, and Omicron with differential transmissibility, pathogenicity, and capacity for immune evasion, thereby altering the epidemiological and clinical landscape of the pandemic and posing specific challenges to clinical management and public health strategies27. This is the first study form Qatar that relies on high-throughput transcriptomic gene expression and clinical data to further our understanding of the underlying molecular processes determining disease severity and mortality in a multiethnic SARS-CoV-2 infected population.
Results
Clinical characteristics of COVID-19 study patients
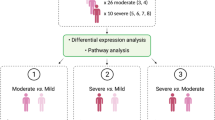
The study encompassed 228 individuals positive for SARS-CoV-2 RT-PCR, featuring a spectrum of clinical presentations ranging from asymptomatic to severe and critical cases (Fig. S1). Notably, 30.7% (n = 70) of the laboratory confirmed COVID-19 positive patients were asymptomatic, 40.3% (n = 92) mildly symptomatic or had mild pneumonia, with the remaining 29% (n = 66) classified as severe or critical with a 12% (n = 28) documented mortality (Table 1). Baseline demographic and clinical characteristics are summarized in Table 1 and supplementary Table 1 (additional clinical data).
The prevalence of diabetes was 53.5% (n = 61/114) and hypertension 58% (n = 67/115) was higher in the severe/critical group. Inflammatory biomarkers such as IL-6 and CRP, known to be predictive markers in COVID-19 patients28were significantly elevated in the COVID-19 cohort suffering from severe/critical disease (Table 1). Additionally, thromboembolic complications were commonly observed in severe COVID-19 cases, with significantly elevated D-dimer and CRP levels (Table 1).
Comprehensive gene expression profiling in patients with varying COVID-19 severity
Transcriptomic changes in patients with varying clinical severity of SARS-CoV-2 infection were analyzed employing RNA-seq along with asymptomatic controls. The global patterns of expression values appear similar and consistent across the samples (Fig. S2). The overall variance in samples measured by principal component analysis (PCA) (Fig. 1A) and hierarchical clustering analysis (Fig. S3) demonstrated discernable gene expression patterns between different severity groups (Fig. 1A). Further analysis aimed to identify genes orchestrating the levels of severity in COVID-19 patients. The study assessed significant differentially expressed genes (DEGs) in pairwise comparisons with an adjusted P-value < 0.05 (Table S2-S4). Overall, when compared to asymptomatic cases, there were 7 genes that were differentially expressed in mild symptomatic patients (3 genes were upregulated, 4 genes were downregulated); 520 genes in mild pneumonia patients (446 genes were upregulated, 74 genes were downregulated); 2236 genes in severe patients (1490 genes were upregulated, 746 genes were downregulated) and 2860 genes in critical patients (1828 genes were upregulated, 1032 genes were downregulated) (Fig. S3; Table S2-S4). Additionally, the analysis of DEGs revealed variations in gene expression within peripheral blood mononuclear cells (PBMCs), reflecting changes associated with different levels of COVID-19 severity, and identifying both common and unique gene signatures. (Fig. 1C & D; Table S5). Notably, gene expression displayed significant variability, with certain genes showing downregulation of up to 30-fold.
Landscape of differential expression genes analysis and Partial Least-Square Discriminant Analysis (PLS-DA). (A) PLS-DA score plot for transcriptomics data, resulting in severity separation along principal component 1 (PC1-22.3%) is presented (B) Volcano plot of differentially expressed genes between COVID-19 transcriptomic profiles of different severity groups of patients showing fold change for each gene and their significance level. Colored dots show genes with an adjusted P-value < 0.05 and an absolute log2 (fold change) > 1. Blue dots represent down-regulated genes, and red dots represent up-regulated genes. Venn diagrams demonstrates the number of overlapping (C) Differentially up regulated genes, and (D) Differentially down regulated genes expressed between COVID-19 subjects.
Identification of differentially expressed genes and partial least-square discriminant analysis (PLS-DA) of COVID-19 patients
In order to highlight the differences between the COVID-19 severity groups, the transcriptomic profiles of each severity group (asymptomatic, mild symptomatic, mild pneumonia, severe and critical) was evaluated against one another where the DEGs are presented in volcano plots using adjusted P-value < 0.05 as cutoff with an absolute log2 (fold change) > 1 (Fig. 1B). The number of genes and their respective fold changes were higher between asymptomatic and critical ICU cohorts. Interestingly, a significant number of genes were downregulated in all symptomatic groups in comparison to asymptomatic controls, including SARS-CoV-2 entry protein the transmembrane protease serine 2 (TMPRSS2), cytotoxic and regulatory T cell molecule (CRTAM) and forkhead box P3 (FOXP3) (Fig. 2 A). Conversely, there was significant upregulation of angiotensin-converting enzyme 2 (ACE2) and key proteins in COVID-19 pathogenesis including arginase 1 (ARG1), Fas-associated death domain protein (FADD), hepatocyte growth factor (HGF) and interleukin 10 (IL10) (Fig. 2 A). PLS-DA analysis showed separation according to severity, wherein 22.3% variation was attributed to principal component 1 (PC1) and minimal separation was observed by principal component 2 (PC2) (Fig. 1A). Additionally, the variable importance of projection (VIP) analysis identified the top 30 contributing transcripts (VIP ≥ 1.3) (Fig. 2B). These top-ranked genes play an important role in hypoxia, apoptosis as well as innate and adaptive immune responses (Table 2). Gene transcripts increased in severe/critical patients, while decreased in mild cases included genes related to mitochondrial function, ionic transport and immune regulation (TMEM11, TXN and SLC22 A4). Adaptive immunity genes, such as IL10RA, TRIM44, PRKCH, MAPRE2, PEA15, CD4, FYN, NFATC, RFTN1, GATA3, SMAD3, PRKCQ, CX3 CR1, and CD247 exhibited suppression with increasing disease severity. Similarly, genes involved in fundamental cellular processes, including gene expression regulation, cell apoptosis, proliferation, and migration such as PRKX, TSPYL1, SMAD3, EVL, RRP1B, KDM2B, and TSHZ1 were downregulated as disease severity increased. Furthermore, genes implicated in cytoskeletal dynamics, intracellular and vesicular trafficking, and protein degradation including ARL4 C, SLC22 A4, EVL, SIDT1, ANKRD40, TMEM11, TIAM1, RASA3 and RNF125 demonstrated a similar pattern of downregulation (Fig. S3; Table S2-S4).
Comparing differently changed genes. A. Gene expression of several key proteins. Dot plot displaying the normalized count of ACE2, TMPRSS2 SARS-CoV-2 entry proteins expression, ARG1, FOXP3, CRTAM, FADD, HGF and IL-10 key proteins expression. Asterisks show significant difference (one-way anova test, Significance codes: >0.05 ‘ns’, < 0.05 ‘*’, < 0.01 ‘**’, < 0.001 ‘***’, 0 ‘****’). Points represent individual patient data. P-values were calculated using a two-tailed Wilcoxon test. B. VIP represents the contribution score of the DEGs that mostly contribute to the differentiation between COVID-19 patients severity groups. The top 30 discriminatory genes are listed from top to bottom, ranked by their VIP scores ≥ 1.3. Changes in expression for each gene are presented, wherein blue: represents decrease and red: represents increase in transcript expression.
Functional enrichment analysis of differentially regulated genes
Functional enrichment analysis was performed on the differentially expressed genes (DEGs) to elucidate their roles in specific cellular biological processes using ShinyGO (version 0.8)54. Interestingly, the up-regulated genes in severe and critical patients were enriched in biological processes of “activation of innate immune cells” specifically in neutrophil activation and degranulation, leukocyte degranulation, granulocyte activation and inflammatory response (Fig. 3A). In addition, a series of inflammation-related processes were activated, such as “regulation of acute inflammatory response” (Fig. 3B). However, downregulated genes were mainly enriched in biological processes of “activation of adaptive immune cells” including cell and biological adhesion, T cell differentiation and activation, lymphocyte activation (Fig. 3). Furthermore, KEGG pathway analysis performed on DEGs in severe COVID-19 samples demonstrated “Metabolic pathways”, “Cell cycle”, “Th1 and Th2 cell differentiation”, and “Th17 cell differentiation” as enriched pathways (Fig. 4). The up-regulated genes in critical ICU admitted cases included the following enriched pathways “Cell cycle”, “Ferroptosis”, and “metabolism”. Whereas, cytokine-related pathways were enriched using the list of down-regulated genes in critical cohort, such as “Th1 and Th2 cell differentiation”, “Cytokine-cytokine receptor interaction”, “Cell adhesion molecules”, “Th17 cell differentiation”, “Natural killer cell mediated cytotoxicity”, “T cell receptor signaling pathway”, “Antigen processing and presentation”, and “Viral protein interaction with cytokine and cytokine receptor” (Fig. 4). Further pathways that were enriched are represented in Fig. S4.
GO-term enrichment analysis of expressed genes. Common genes-based GO-term analysis sorted by adjusted P-values. GO term functional enrichment by Biological Process (BP) were performed for A-B up and down-regulated genes in COVID-19 mild pneumonia patients. C-D. BP analysis for up and down-regulated genes in COVID-19 severe patients. E-F. BP analysis for up and down-regulated genes in COVID-19 critical patients.
KEGG pathway enrichment analysis of expressed genes. Common genes-based KEGG pathway enrichment analysis sorted by adjusted P-values. KEGG pathway enrichment analysis for A-B up and down-regulated genes in COVID-19 severe patients. C-D. KEGG pathway analysis for up and down-regulated genes in COVID-19 critical patients.
Diminished intracellular immunity and potent neutrophils activation gene signature in severe and critical cohort of COVID-19 patients
Previous clinical studies have demonstrated that COVID-19 patients experience a cytokine storm, reminiscent of the response observed in SARS-CoV as well as MERS infections15,24,55,56. To visualize the difference in the immune response between various severity groups, we used the log2 fold change values of the DEGs associated with T cell functionality, neutrophil activation and plasma cytokines to plot a heatmap (Fig. S5 and S6). In severe and critical patients, increased gene expression was observed in granulocyte- and monocyte-associated molecules (eosinophil-derived neurotoxin; RNASE2), and neutrophil activation-associated CD177 and neutrophil elastase (ELANE) (Fig. S5 A). However, these patients had lower expressions of lymphocyte-associated molecules including CD4, CD247, KLRB1, and TCF7 (Fig. S5 A). Similarly, a decrease in the expression of several cytokine genes such as CCL4, CXCL8, IFNG, IL17B, IL23 A, IL34, and genes associated with T/NK cell effector functionality including CCL4, CIMAP7, GZMA, GZMK, HCST, ID2 was identified in severe/critical patients. Analysis of interferon (IFN) and pattern recognition receptors (PRR)-induced signaling indicated that antiviral IFN responses and virus sensing PRR signaling pathways were differentially regulated according to disease severity with a dysregulated expression of type I and III interferons in severe and ICU COVID-19 cases (Fig. S5B and C). Furthermore, platelets in severe/critical COVID-19 patients had a hyperactivated phenotype with altered gene expression (Fig. S5D)57. In agreement with published research, we observe an upregulation of genes related to transforming growth factors, interferons, and interleukins such as IFITM1, IFITM3 and IL10 in severe and critical cases20,23,58.
Lymphocyte survival genes are dysregulated in severely ill patients infected with SARS-CoV-2
Previous clinical and autopsy reports have indicated reduced lymphocyte counts in critically ill COVID-19 patients with an increase in neutrophil to lymphocyte ratio (Table 1)25,59,60,61. The data from this study reveals that several genes involved in apoptosis and P53 signaling pathways (Fig. S5E and Fig. S6) including BAD, ATF4, CTSB, CTSO, PRF1 and TP53I3 are dysregulated. Interestingly, the macroautophagy machinery is among the most enriched biological processes, implicating its significance in disease severity. Therefore, gene expression analysis within this ontology term revealed significantly altered autophagosome and autophagy-related genes in patients classified as severe or critical (Fig. S6)62. For instance, autophagy regulatory genes, such as MAP1LC3, were globally upregulated in severe and critical COVID-19 patients, which positively regulates the process of autophagosome formation63,64.
Gene expression profiling revealed significant differences in circulating immune cells
The composition of circulating immune cells varies with the COVID-19 disease severity42. To further explore this finding in our samples, cell populations were estimated by deconvolution of RNAseq data (Fig. 5; fig. S7). Our analysis revealed a higher granulocyte proportion in severe and critical patients, with a lower proportion of lymphocytes and natural killer cells (Fig. 5A). Following deconvolution and adjustment by total granulocyte fraction, an increased proportion of neutrophils with a decreased proportion of eosinophils were observed, while no significant changes were detected in basophil cells (Fig. 5D and Fig. S7). Furthermore, while no difference in monocytes was observed across severity groups, the monocyte fraction showed a high expression of CD14+ and low expression of CD16+ monocytes suggesting an increase in classical monocyte population with increasing severity65 (Fig. S7). In agreement with the clinical data, we observed a decrease in pan T cells (including T cell subsets) and naïve B cells, whereas no change in memory B-cells were found (Fig. 5B and Fig. S7). Intriguingly, CD56bright NK cells and disease severity had an inverse correlation66 (Fig. 5C). Moreover, in severe/critical patients a higher percentage of myeloid versus lymphoid origin cells correlated with the clinical data that demonstrated a higher neutrophil to lymphocyte ratio, further corroborating with the hyper-inflammatory responses observed in this cohort (Fig. 5D; Table 1).
Estimated circulating immune cell populations. Proportions of circulating immune cell populations estimated from transcriptome data. (A) The average proportion of blood cells were predicted from transcriptome data using a deconvolution algorithm. (B) Lymphocyte subpopulations expressed as proportion of the absolute number of lymphocytes. (C) Natural killer cell subpopulations expressed as proportion of the absolute number of natural killer cells. (D) The proportion of neutrophils and the neutrophil to lymphocyte ratio (NLR) predicted from transcriptome data. The proportion of lymphocyte corresponds to the sum of proportions of T cells, B cells, and NK cells. Asterisks show significant difference (one-way anova test, Significance codes: >0.05 ‘ns’, < 0.05 ‘*’, < 0.01 ‘**’, < 0.001 ‘***’, 0 ‘****’). Points represent individual patient data. P-values were calculated using a two-tailed Wilcoxon test.
Modular co-expression analyses identified six key modules of hub genes in COVID-19 severity groups
Functional enrichment analysis suggested a systemic change in immune response-associated genes and pathways. To identify key gene groups namely modules that are co-expressed, we performed comprehensive modular co-expression analysis. Our analysis revealed six modules of co-expressed genes that either work together or are similarly co‐regulated in our cohort (Fig. 6). Among the six modules, M1 (Fig. 6C) and M2 modules (Fig. 6D) were significantly downregulated (Fig. 6A), whereas, M5 and M6 (Fig. 6E and F) were significantly upregulated in severe and critical groups (Fig. 6A). Over-representation analysis of the six modules uncovered several commonly enriched pathways, related to innate and adaptive immune system, including interferon signaling, cytokine-cytokine receptor interaction, and complement activation and coagulation cascades (Fig. 6C-F), in addition to cell cycle‐related pathways (Fig. S8). Within the identified modules, hub genes were characterized and highlighted by the most connected genes, which included genes associated with neutrophil activation, innate immune response to viral infection, and cell cycle pathways and ribosomes (Fig. 6B; Table S6). These findings underscore significant molecular alterations in the innate and adaptive immune system, as well as significant changes in cell cycle during SARS-CoV-2 infection.
Co-expression gene modules present in blood transcriptomes of COVID‐19 patients. (A) Bubble heatmap showing the results of gene set enrichment analysis, indicating the module (M) activity in COVID‐19 patients. Circle size and color reflect the normalized enrichment score (NES), as determined by CEMiTool. (B) Enriched modules contain hubs genes. (C) Interaction plot for M1, (D) M2, (E) M5 and (F) M6, which contains genes enriching different immunity‐associated pathways, exhibited by the GO BP and KEGG pathway bar plot at the right side of Fig. C-F. The most connected genes (hubs) are highlighted inside rectangles. The node size is proportional to its degree of interactivity. The bar plot indicates the top 10 enriched pathways from the over‐representation analysis of module M1: C, M2: D, M5: E and M6: F.
Discussion
This study explores the transcriptome of venous blood from individuals diagnosed with different severity levels of COVID-19 disease. Global RNA-seq was performed on 228 COVID-19-positive patients, including asymptomatic, mild symptomatic, mild pneumonia, severe and critical (Table 1 and Fig. S1)67,68. Whereas previous studies have investigated SARS-CoV-2 infection comparing hospitalized to non-hospitalized patients or ICU to non-ICU cases, and others categorized patients by illness type or severity level, we examined five COVID-19 severity cohorts, particular distinguishing between severe and critical cases, and including comparisons with asymptomatic patients. In addition, this study includes a diverse multi-ethnic cohort, exploring gene expression and immune responses across different ethnic groups. As the first transcriptomic investigation from the Middle East with large, ethnically varied samples, this research provides valuable insights into how genetic and environmental factors influence COVID-19 severity to foster the development of inclusive treatment strategies.
Notably, critical cohort of COVID-19 patients displayed the highest number of differentially expressed genes (DEGs) compared to asymptomatic individuals (Fig. 1). COVID-19 severity was also found to correlate with proteins that facilitate SARS-CoV-2 viral uptake, such as ACE2 and TMPRSS2 (Fig. 2). Interestingly, the relationship between viral load and disease severity remains unclear according to current literature69,70. The VIP analysis pinpointed the IL-10 receptor as the top predictor of disease severity, showing an inverse correlation and aligning with clinical data that report elevated IL-10 levels in severe cases (Fig. 2)24. Additionally, GO analysis revealed significant enrichment in biological processes related to innate immunity and the complement system, along with notable suppression of lymphocyte function likely through disrupted T cell signaling/exhaustion and calcium homeostasis. The signaling pathways and genes involved in innate immunity, in particular those related to neutrophil activation, secondary to Th-17 induction, as well as interferon signaling pathways exhibited upregulation especially in severe and critical ICU cases of COVID-19 (Figs. 3, 4 and 5 and S5). The cumulative upregulation of these pathways indicates increased cytokine or chemokine activity and the enhancement of inflammatory processes reliant on innate immune responses, consistent with prior literature71,72,73,74,75. The differential responses observed among the groups can be attributed to the variability in disease progression. Patients with more severe or critical disease outcomes exhibited more pronounced type I interferon responses63,64. Furthermore, KEGG pathways analysis demonstrated an upregulation of innate immunity genes linked to cytokine storm, including genes associated with complement and cytokine production like IL-18, interferon-based antiviral responses, reactive oxygen species, Matrix metalloproteinases (MMP) formation, secretory granule formation, and exocytosis (Fig. 4). The identified DEGs align with clinical data showing an elevated total white blood cell count, accompanied by an increased number of circulating neutrophils (Table 1), that is supported by DEGs involved in increased granulocytes and neutrophil levels (Fig. 5). Additionally, the study further highlighted a decrease in NK cell population and pro-inflammatory CD16high monocytes fraction following pulmonary damage, which worsens with oxygen dependency in ICU patients (Fig. 5). Similarly, Guardela et al. have reported 50 genes in a longitudinal study of a small cohort of ICU cases indicating NK cell and monocyte impairment with exaggerated neutrophil responses76similar to previous studies75,77.
The impact of SARS-CoV-2 infection severity on the impairment of adaptive immune responses has been extensively documented24,42,78,79,80. This study further contributes to the growing body of evidence on the impaired anti-viral adaptive immune response, where the lymphocyte count decrease with increasing COVID-19 severity, a decline that is linked to apoptosis (Table 1). As pneumonia manifests in SARS-CoV-2-infected patients, several differentially expressed genes (DEGs) promoting apoptosis are upregulated, while those exhibiting anti-apoptotic properties, including BCL-2 and genes involved in P53 pathways such as CDK6 and CDK2 in cell cycle regulation, are downregulated (Fig. 6). It is well established that IL-10 signaling suppresses activated T cells and neutrophils81,82. The reduced expression of IL-10R expression in ICU patients may lead to unregulated neutrophil activation. Conversely, lymphocytes that are unresponsive to IL-10 signaling are likely to upregulate pro-apoptotic pathways, contributing to reduction in CD4 and CD8 T lymphocyte populations in severe and ICU COVID-19 cases. This targeted suppression of T cells (Fig. 5) is likely due to downregulation of genes involved downstream of TCR signaling, such as CD4, FYN, NFATC PRKCH, MAPRE2, PEA15, GATA3, PRKCQ, and CD247, which limits clonal expansion and induces apoptosis (Fig. 2). Specifically, the downregulation of IL-7R correlates with decreased lymphocyte counts, as IL-7 signaling is crucial for the maintenance of T and B cells83,84. Additionally, in our cohort genes involved in cytotoxic anti-viral responses, such as Granzymes, are significantly downregulated in severely ill COVID-19 patients. The observed decrease in lymphocyte count as well as the expression of genes associated with disrupted T cell activation85collectively highlights dysregulated effector functions of adaptive T cell-mediated immunity. This includes both the suppression of adaptive immune responses and the induction of early apoptosis, which affects lymphocyte maintenance.
Thromboembolic complications are a major concern in severe COVID-19, with multiple studies reporting high rates of venous and arterial thromboses in hospitalized patients86,87,88,89,90,91. A thromboembolism incidence of 27.6% was observed in ICU patients86while other studies reported rates as high as 31% despite prophylaxis92. A meta-analysis showed a pooled VTE prevalence of ~ 31% in critically ill COVID-19 patients, increasing to nearly 50% with systematic screening90. These rates highlight the distinct coagulopathy of COVID-19, characterized by elevated cytokines, endothelial injury, and microthrombi87. Elevated D-dimer levels are strongly associated with disease severity and thrombotic risk93,94. Similarly, elevated CRP levels were linked to higher VTE risk, ICU admission, and mortality, particularly when both markers were elevated93,95. These findings underscore the interplay of inflammation and coagulopathy in severe COVID-19.
SARS-CoV-2 has evolved through mutations, particularly in the spike protein, giving rise to variants with distinct profiles in transmissibility, virulence, and immune evasion. These evolutionary changes have significantly shaped the trajectory of the pandemic, influencing both clinical outcomes and public health responses. Contrary to our data from the first COVID-19 wave, which identified key immune transcriptomic signatures associated with disease severity, later waves have been driven by the emergence of major SARS-CoV-2 variants of concern, including Alpha, Beta, Gamma, Delta, and Omicron. Each variant presented unique challenges, Alpha (B.1.1.7) showed increased transmissibility and a higher risk of severe outcomes96Beta (B.1.351) and Gamma (P.1) exhibited considerable immune evasion97 without clearly increasing virulence. Notably, the Delta variant was linked to increased disease severity and higher hospitalization rates, whereas the Omicron (B.1.1.529) with its numerous spike protein mutations, has been associated with widespread reinfections and breakthrough cases due to immune escape27while generally leading to less severe disease, possibly owing to prior immunity and its preference for upper respiratory tract replication98. The emergence of highly mutated variants has also led to partial escape from immunity, acquired through prior infection or vaccination. Future research should aim to incorporate variant-specific immune transcriptomic analyses, thereby enhancing our understanding of severity markers across diverse SARS-CoV-2 lineages and informing precision public health responses.
While this study provides valuable insights, it is important to acknowledge that it has its limitations. The severe cohort could not be age- and gender-matched with the asymptomatic cases due to the predominance of older individuals among those with severe disease and the higher proportion of males in our sample, a reflection of case presentation and sampling conditions. Future research should incorporate larger, demographically balanced cohorts to enable more accurate stratification. Additionally, the cross-sectional design limits causal inference. Longitudinal studies would provide deeper insights into the progression of immune responses over time and their relationship to disease outcomes. Nevertheless, with a sample size of 228 patients, one of the largest RNA-seq cohorts to date addressing five severity group from a multi-ethnic population (Table S7) using blood samples, this study is robustly equipped to address a substantial amount of biological variability. To address potential confounding effects, we implemented quality control steps, data preprocessing, and normalization. While RNA samples obtained from bedside samples using PAXgene tubes are well preserved, these tubes are not suitable for single-cell RNA sequencing due to their bulk RNA stabilization, which prevents isolation and analysis of individual cells. Additionally, while the immune cell abundances described in this manuscript have not been validated through flow cytometry, the reliability of the deconvolution methods used has been previously confirmed with flow cytometry measurements99,100. While several studies have addressed related questions, our research uniquely focuses on aspects of the COVID-19 disease spectrum that have not been examined in a single study.
Conclusions
Understanding immune responses in COVID-19 patients is crucial for evaluating treatment efficacy, predicting disease prognosis, and elucidating the variability in disease severity. Despite extensive research on SARS-CoV-2, including efforts in vaccine development aimed at reducing disease severity rather than traditional prevention, the factors driving the clinical spectrum of COVID-19 remain poorly understood. The degree of variability in clinical presentation observed in COVID-19 is exceptional among emerging highly transmissible pathogens, highlighting a unique challenge in understanding and managing COVID-19101. SARS-CoV-2 infection can manifest across a spectrum of illnesses, from asymptomatic or mild flu-like symptoms to severe pulmonary disease, which may be accompanied by significant morbidities and mortalities102. Despite the pandemic having lasted for four years, our comprehension of the host immune response to SARS-CoV-2 infection spectrum remains incomplete. This study contributes to the field by elucidating the transcriptomic differences among individuals with COVID-19, encompassing asymptomatic and mildly symptomatic cases, as well as those with mild pneumonia, severe disease, and critical conditions. To the best of our knowledge, this represents the first large-scale investigation of 228 patients that delineates gene expression-based clinical spectrum of COVID-19 within the Gulf region.
Methods
Study design
This cross-sectional study includes 228 of the initially recruited 279 COVID-19 patients infected with SARS-CoV-2 by the national public health care provider (Hamad Medical Corporation - HMC) in Qatar, between July 2020 and August 2021 identified via public screening programs or hospital admission (Fig. S1). The samples analyzed in this study were collected during the first wave of COVID-19 prior to vaccination in Qatar, between July 14 th and October 20 th 2020, in Doha Qatar. All cases were diagnosed in labs reporting to public health care facilities using RT-PCR, employing TaqPath COVID-19 Combo Kit (Thermo Fisher Scientific, Waltham, Massachusetts) or Cobas SARS-CoV-2 Test (Roche Diagnostics, Rotkreuz, Switzerland) from throat or nasopharyngeal swabs. Consented patients provided 2.5 and 4 ml of venous blood samples for PAXgene and EDTA tubes respectively, at the time of diagnosis, post-isolation or hospitalization of which 228 samples are reported in this research following quality assurance (Fig. S1). The study cohort included cases of several nationalities resident in Qatar and categorized into five groups: asymptomatic (n = 70), mild symptomatic (n = 41), mild pneumonia (n = 51), severe (n = 33), and critical (n = 33) following COVID-19 WHO guidelines103. The hospitalized COVID-19 patients with severe to critical cases were provided oxygen support in intensive care unit (ICU), out of which 31 patients died of respiratory failure. All participants were followed for a period of 3 months, with ICU mortality assessed at discharge and overall mortality recorded at the end of the follow-up period. Clinical, demographic, and anthropometric data, along with medical history and COVID-19 severity, were retrieved from HMC’s electronic healthcare system (CERNER) with patient consent. The cohort included 188 male participants, with ages ranging from 21 to 87 years. The study protocol was conducted in accordance with all guidelines and regulations and approved by the Institutional Review Boards (IRBs). None of the patients included had previously diagnosed malignancies. However, pre-existing chronic conditions were noted in some study participants (bronchial asthma in 9 patients, liver cirrhosis in 5, end stage renal disease in 7, cardiovascular disease in 29, and cerebrovascular disease in 14 patients respectively). Importantly, no other infections were identified from the patient’s clinical records. We had limited access to female patients (n = 39) due to predominant male infectivity and other constraints during sample collection.
Sample preparation and RNA isolation
Patient’s venous blood was collected in PAXgene Blood RNA Tubes (Pre Analytix), mixed to ensure complete lysis and total RNA extracted and purified using Blood miRNA kit from Qiagen (Cat. No: 763134, PreAnalytiX GmBH Hombrechtikon, Switzerland) according to the manufacturer’s instructions. The concentration and quality of RNA were assessed by Agilent Bioanalyzer 2100 (Agilent Technologies, CA).
Library construction and sequencing
The Poly-A containing mRNA molecules were purified from total RNA using poly-T oligo hybridization (dT)-attached magnetic beads from 1 µg of total RNA. The mRNA molecules were fragmented into small pieces using fragmentation reagent, followed by synthesized cDNA using SuperScript III (Invitrogen, MA). Libraries for sequencing were prepared according to the manufacturer’s instructions with mRNA Library Prep Kit (BGI) and paired-end sequencing was done by DNBSEQ high-throughput platform.
Data analysis
The raw data were subjected to QC analyses using the FastQC tool (version 0.11.9) (http://www.bioinformatics.babraham.ac.uk/projects/fastqc). Gene expression was calculated by HTSeq104. Differentially expressed genes were identified using DESeq2 pipeline105. P-values were calculated using a paired, two-sided Wilcoxon test, and adjusted P-value (pAdj) were corrected using the Benjamini–Hochberg method. Genes with log2 fold change > 1 or < − 1, pAdj < 0.05 value were considered significant. For significance of each GSEA category, significantly regulated gene sets were evaluated with the Kolmogorov–Smirnov statistic. Demographic data were analyzed by Kruskal-Wallis rank sum test and Fisher’s exact test. A value of p < 0.05, *p < 0.001, **p < 0.0001, ***p < 0.00001 was considered statistically significant. Functional enrichment analysis was performed on the list of differentially expressed genes by using GO enrichment and Ingenuity Pathway Analysis (IPA) and clusterProfiler and ShinyGo (version 0.80) R packages54,106. KEGG pathway enrichment analysis was conducted using R package (ClusterProfiler) to identify significantly enriched biological pathways associated with the gene expression data107,108. Gene co-expression network analysis was done using CEMiTool109.
Circulating cell populations
A variety of computational methods have recently been developed to estimate cell type composition from bulk RNA sequencing data, a process commonly referred to as decomposition or deconvolution. Widely used tools such as MCP-Counter, xCell, and CIBERSORT are popular choices, though they present certain limitations, including incomplete representation of immune cell types. In this study, we employed the Gene Expression Deconvolution Interactive Tool (GEDIT)110which infers the proportions of transcriptionally active circulating immune cell types based on gene expression profiles. GEDIT includes 11 distinct reference matrices optimized for different sample types; we utilized the LM22 and ImmunoStates matrices with default settings. A comprehensive description of the GEDIT algorithm is shown in Fig. S9.
Data availability
The original contributions presented in the study are included in the article/Supplementary Material. The FASTQ files are available through the Gene Expression Omnibus (GEO) database. For any further inquiries, please contact the corresponding authors.
References
Phelan, A. L., Katz, R. & Gostin, L. O. The novel coronavirus originating in wuhan, china: challenges for global health governance. JAMA 323, 709–710. https://doi.org/10.1001/jama.2020.1097 (2020).
Fu, L. et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in china: A systematic review and meta-analysis. J. Infect. 80, 656–665. https://doi.org/10.1016/j.jinf.2020.03.041 (2020).
Williamson, E. J. et al. Factors associated with COVID-19-related death using opensafely. Nature 584, 430–436. https://doi.org/10.1038/s41586-020-2521-4 (2020).
Tavasolian, F. et al. Immune response, and susceptibility to COVID-19. Front. Immunol. 11, 601886. https://doi.org/10.3389/fimmu.2020.601886 (2020).
Schafer, A. & Baric, R. S. Epigenetic Landscape during Coronavirus Infection. Pathogens https://doi.org/10.3390/pathogens6010008 (2017).
Islam, A. et al. Transcriptome of nasopharyngeal samples from COVID-19 patients and a comparative analysis with other SARS-CoV-2 infection models reveal disparate host responses against SARS-CoV-2. J. Transl Med. 19, 32. https://doi.org/10.1186/s12967-020-02695-0 (2021).
Baranova, A., Cao, H., Teng, S. & Zhang, F. A phenome-wide investigation of risk factors for severe COVID-19. J. Med. Virol. 95, e28264. https://doi.org/10.1002/jmv.28264 (2023).
Baranova, A., Cao, H. & Zhang, F. Causal associations and shared genetics between hypertension and COVID-19. J. Med. Virol. 95, e28698. https://doi.org/10.1002/jmv.28698 (2023).
Cao, H., Baranova, A., Wei, X., Wang, C. & Zhang, F. Bidirectional causal associations between type 2 diabetes and COVID-19. J. Med. Virol. 95, e28100. https://doi.org/10.1002/jmv.28100 (2023).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl. J. Med. 383, 2603–2615. https://doi.org/10.1056/NEJMoa2034577 (2020).
Voysey, M. et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in brazil, South africa, and the UK. Lancet 397, 99–111. https://doi.org/10.1016/S0140-6736(20)32661-1 (2021).
Kindler, E., Thiel, V. & SARS-CoV Too little, too late. Cell. Host Microbe. 19, 139–141. https://doi.org/10.1016/j.chom.2016.01.012 (2016).
Fehr, A. R., Channappanavar, R. & Perlman, S. Middle East respiratory syndrome: emergence of a pathogenic human coronavirus. Annu. Rev. Med. 68, 387–399. https://doi.org/10.1146/annurev-med-051215-031152 (2017).
Chen, Y., Liu, Q. & Guo, D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J. Med. Virol. 92, 418–423. https://doi.org/10.1002/jmv.25681 (2020).
Channappanavar, R. et al. Dysregulated type I interferon and inflammatory Monocyte-Macrophage responses cause lethal pneumonia in SARS-CoV-Infected mice. Cell. Host Microbe. 19, 181–193. https://doi.org/10.1016/j.chom.2016.01.007 (2016).
Montazersaheb, S. et al. COVID-19 infection: an overview on cytokine storm and related interventions. Virol. J. 19, 92. https://doi.org/10.1186/s12985-022-01814-1 (2022).
de Wit, E., van Doremalen, N., Falzarano, D. & Munster, V. J. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 14, 523–534. https://doi.org/10.1038/nrmicro.2016.81 (2016).
Ramatillah, D. L. et al. Impact of cytokine storm on severity of COVID-19 disease in a private hospital in West Jakarta prior to vaccination. PLoS One. 17, e0262438. https://doi.org/10.1371/journal.pone.0262438 (2022).
Hojyo, S. et al. How COVID-19 induces cytokine storm with high mortality. Inflamm. Regen. 40, 37. https://doi.org/10.1186/s41232-020-00146-3 (2020).
Xiong, Y. et al. Transcriptomic characteristics of Bronchoalveolar lavage fluid and peripheral blood mononuclear cells in COVID-19 patients. Emerg. Microbes Infect. 9, 761–770. https://doi.org/10.1080/22221751.2020.1747363 (2020).
Ilieva, M., Tschaikowski, M., Vandin, A. & Uchida, S. The current status of gene expression profilings in COVID-19 patients. Clin. Transl Discov. 2, e104. https://doi.org/10.1002/ctd2.104 (2022).
Wargodsky, R. et al. RNA sequencing in COVID-19 patients identifies neutrophil activation biomarkers as a promising diagnostic platform for infections. PLoS One. 17, e0261679. https://doi.org/10.1371/journal.pone.0261679 (2022).
Jain, R. et al. Host transcriptomic profiling of COVID-19 patients with mild, moderate, and severe clinical outcomes. Comput. Struct. Biotechnol. J. 19, 153–160. https://doi.org/10.1016/j.csbj.2020.12.016 (2021).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in wuhan, China. Lancet 395, 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5 (2020).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in wuhan, china: a descriptive study. Lancet 395, 507–513. https://doi.org/10.1016/S0140-6736(20)30211-7 (2020).
Xu, Z. et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 8, 420–422. https://doi.org/10.1016/S2213-2600(20)30076-X (2020).
Carabelli, A. M. et al. SARS-CoV-2 variant biology: immune escape, transmission and fitness. Nat. Rev. Microbiol. 21, 162–177. https://doi.org/10.1038/s41579-022-00841-7 (2023).
Herold, T. et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol 146, 128-136.e124. https://doi.org/10.1016/j.jaci.2020.05.008 (2020).
Luporini, R. L. et al. IL-6 and IL-10 are associated with disease severity and higher comorbidity in adults with COVID-19. Cytokine 143, 155507. https://doi.org/10.1016/j.cyto.2021.155507 (2021).
Santamaria, P. Cytokines and chemokines in autoimmune disease: an overview. Adv. Exp. Med. Biol. 520, 1–7. https://doi.org/10.1007/978-1-4615-0171-8_1 (2003).
Yang, B. et al. Novel function of Trim44 promotes an antiviral response by stabilizing VISA. J. Immunol. 190, 3613–3619. https://doi.org/10.4049/jimmunol.1202507 (2013).
Basu, A., Pal, D. & Blaydes, R. Differential effects of protein kinase C-eta on apoptosis versus senescence. Cell. Signal. 55, 1–7. https://doi.org/10.1016/j.cellsig.2018.12.003 (2019).
Liu, H. Y., Pedros, C., Kong, K. F., Canonigo-Balancio, A. J. & Altman, A. Protein kinase C-eta deficiency does not impair antiviral immunity and CD8(+) T cell activation. J. Immunol. 204, 2439–2446. https://doi.org/10.4049/jimmunol.1900963 (2020).
Renner, C. et al. RP1, a new member of the adenomatous polyposis coli-binding EB1-like gene family, is differentially expressed in activated T cells. J. Immunol. 159, 1276–1283 (1997).
Kerbrat, S. et al. Absence of the adaptor protein PEA-15 is associated with altered pattern of Th cytokines production by activated CD4 + T lymphocytes in vitro, and defective red blood cell alloimmune response in vivo. PLoS One. 10, e0136885. https://doi.org/10.1371/journal.pone.0136885 (2015).
Gorska, M. M., Stafford, S. J., Cen, O., Sur, S. & Alam, R. Unc119, a novel activator of lck/fyn, is essential for T cell activation. J. Exp. Med. 199, 369–379. https://doi.org/10.1084/jem.20030589 (2004).
Blank, C. U. et al. Defining ‘T cell exhaustion’. Nat. Rev. Immunol. 19, 665–674. https://doi.org/10.1038/s41577-019-0221-9 (2019).
Malissen, B., Gregoire, C., Malissen, M. & Roncagalli, R. Integrative biology of T cell activation. Nat. Immunol. 15, 790–797. https://doi.org/10.1038/ni.2959 (2014).
Peng, J., Zhu, X., Zhuang, W., Luo, H. & Wang, E. From sleep deprivation to severe COVID-19: A comprehensive analysis of shared differentially expressed genes and potential diagnostic biomarkers. Front. Biosci. (Landmark Ed). 29, 107. https://doi.org/10.31083/j.fbl2903107 (2024).
Berg, T. et al. Expression of MATE1, P-gp, OCTN1 and OCTN2, in epithelial and immune cells in the lung of COPD and healthy individuals. Respir Res. 19, 68. https://doi.org/10.1186/s12931-018-0760-9 (2018).
Saeki, K., Miura, Y., Aki, D., Kurosaki, T. & Yoshimura, A. The B cell-specific major raft protein, raftlin, is necessary for the integrity of lipid raft and BCR signal transduction. EMBO J. 22, 3015–3026. https://doi.org/10.1093/emboj/cdg293 (2003).
Rydyznski Moderbacher, C. et al. Antigen-Specific Adaptive Immunity to SARS-CoV-2 in Acute COVID-19 and Associations with Age and Disease Severity. Cell 183, 996-1012.e1019. https://doi.org/10.1016/j.cell.2020.09.038 (2020).
Kalfaoglu, B., Almeida-Santos, J., Tye, C. A., Satou, Y. & Ono, M. T-Cell hyperactivation and paralysis in severe COVID-19 infection revealed by Single-Cell analysis. Front. Immunol. 11, 589380. https://doi.org/10.3389/fimmu.2020.589380 (2020).
Chang, H. et al. CD97 negatively regulates the innate immune response against RNA viruses by promoting RNF125-mediated RIG-I degradation. Cell. Mol. Immunol. 20, 1457–1471. https://doi.org/10.1038/s41423-023-01103-z (2023).
Zhou, Z. et al. Decreased HD-MIR2911 absorption in human subjects with the SIDT1 polymorphism fails to inhibit SARS-CoV-2 replication. Cell. Discov. 6, 63. https://doi.org/10.1038/s41421-020-00206-5 (2020).
Nguyen, T. A. et al. SIDT1 localizes to endolysosomes and mediates Double-Stranded RNA transport into the cytoplasm. J. Immunol. 202, 3483–3492. https://doi.org/10.4049/jimmunol.1801369 (2019).
Krummel, M. F. Immunological synapses: breaking up May be good to do. Cell 129, 653–655. https://doi.org/10.1016/j.cell.2007.05.008 (2007).
Banerjee, A. K. et al. SARS-CoV-2 Disrupts Splicing, Translation, and Protein Trafficking to Suppress Host Defenses. Cell 183, 1325-1339.e1321. https://doi.org/10.1016/j.cell.2020.10.004 (2020).
Agrawal, P., Sambaturu, N., Olgun, G., Hannenhalli, S. A. & Path-Based Analysis of infected cell line and COVID-19 patient transcriptome reveals novel potential targets and drugs against SARS-CoV-2. Front. Immunol. 13, 918817. https://doi.org/10.3389/fimmu.2022.918817 (2022).
Mohammadhosayni, M. et al. Matrix metalloproteinases are involved in the development of neurological complications in patients with coronavirus disease 2019. Int. Immunopharmacol. 100, 108076. https://doi.org/10.1016/j.intimp.2021.108076 (2021).
Sharif-Askari, S. Upregulation of oxidative stress gene markers during SARS-COV-2 viral infection. Free Radic Biol. Med. 172, 688–698. https://doi.org/10.1016/j.freeradbiomed.2021.06.018 (2021).
Dexiu, C., Xianying, L. & Yingchun, H. Jiafu, L. Advances in CD247. Scand. J. Immunol. 96, e13170. https://doi.org/10.1111/sji.13170 (2022).
Moni, M. A. & Lio, P. Network-based analysis of comorbidities risk during an infection: SARS and HIV case studies. BMC Bioinform. 15, 333. https://doi.org/10.1186/1471-2105-15-333 (2014).
Ge, S. X., Jung, D. & Yao, R. ShinyGO: a graphical gene-set enrichment tool for animals and plants. Bioinformatics 36, 2628–2629. https://doi.org/10.1093/bioinformatics/btz931 (2020).
Jiang, Y. et al. Characterization of cytokine/chemokine profiles of severe acute respiratory syndrome. Am. J. Respir Crit. Care Med. 171, 850–857. https://doi.org/10.1164/rccm.200407-857OC (2005).
Alosaimi, B. et al. MERS-CoV infection is associated with downregulation of genes encoding Th1 and Th2 cytokines/chemokines and elevated inflammatory innate immune response in the lower respiratory tract. Cytokine 126, 154895. https://doi.org/10.1016/j.cyto.2019.154895 (2020).
Alakus, T. B. & Turkoglu, I. Comparison of deep learning approaches to predict COVID-19 infection. Chaos Solitons Fractals. 140, 110120. https://doi.org/10.1016/j.chaos.2020.110120 (2020).
Dhar, S. K., Damodar, K. V., Gujar, S., Das, M. & S. & IL-6 and IL-10 as predictors of disease severity in COVID-19 patients: results from meta-analysis and regression. Heliyon 7, e06155. https://doi.org/10.1016/j.heliyon.2021.e06155 (2021).
Anwardeen, N. R. et al. The retrospective study of the metabolic patterns of BCG-vaccination in type-2 diabetic individuals in COVID-19 infection. Front. Immunol. 14, 1146443. https://doi.org/10.3389/fimmu.2023.1146443 (2023).
Cyprian, F. S. et al. Complement C5a and clinical markers as predictors of COVID-19 disease severity and mortality in a Multi-Ethnic population. Front. Immunol. 12, 707159. https://doi.org/10.3389/fimmu.2021.707159 (2021).
Shuaib, M. et al. Impact of the SARS-CoV-2 nucleocapsid 203K/204R mutations on the inflammatory immune response in COVID-19 severity. Genome Med. 15, 54. https://doi.org/10.1186/s13073-023-01208-0 (2023).
Yin, Z., Pascual, C. & Klionsky, D. J. Autophagy: machinery and regulation. Microb. Cell. 3, 588–596. https://doi.org/10.15698/mic2016.12.546 (2016).
Bonam, S. R., Bayry, J., Tschan, M. P. & Muller, S. Progress and Challenges in The Use of MAP1LC3 as a Legitimate Marker for Measuring Dynamic Autophagy In Vivo. Cells https://doi.org/10.3390/cells9051321 (2020).
Yu, C. et al. TMEM74, a lysosome and autophagosome protein, regulates autophagy. Biochem. Biophys. Res. Commun. 369, 622–629. https://doi.org/10.1016/j.bbrc.2008.02.055 (2008).
Ziegler-Heitbrock, L. et al. Nomenclature of monocytes and dendritic cells in blood. Blood 116, e74–80. https://doi.org/10.1182/blood-2010-02-258558 (2010).
Michel, T. et al. Human CD56bright NK cells: an update. J. Immunol. 196, 2923–2931. https://doi.org/10.4049/jimmunol.1502570 (2016).
Su, Y. et al. Multi-Omics Resolves a Sharp Disease-State Shift between Mild and Moderate COVID-19. Cell 183, 1479-1495.e1420. https://doi.org/10.1016/j.cell.2020.10.037 (2020).
Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell 184, 3573-3587.e3529. https://doi.org/10.1016/j.cell.2021.04.048 (2021).
Puhach, O., Meyer, B. & Eckerle, I. SARS-CoV-2 viral load and shedding kinetics. Nat. Rev. Microbiol. 21, 147–161. https://doi.org/10.1038/s41579-022-00822-w (2023).
Cevik, M. et al. SARS-CoV-2, SARS-CoV, and MERS-CoV viral load dynamics, duration of viral shedding, and infectiousness: a systematic review and meta-analysis. Lancet Microbe. 2, e13–e22. https://doi.org/10.1016/S2666-5247(20)30172-5 (2021).
Leung, B. P. et al. A role for IL-18 in neutrophil activation. J. Immunol. 167, 2879–2886. https://doi.org/10.4049/jimmunol.167.5.2879 (2001).
Henderson, L. A. et al. On the alert for cytokine storm: immunopathology in COVID-19. Arthritis Rheumatol. 72, 1059–1063. https://doi.org/10.1002/art.41285 (2020).
Jamison, D. A. Jr. et al. A comprehensive SARS-CoV-2 and COVID-19 review, part 1: intracellular overdrive for SARS-CoV-2 infection. Eur. J. Hum. Genet. 30, 889–898. https://doi.org/10.1038/s41431-022-01108-8 (2022).
Daamen, A. R. et al. COVID-19 patients exhibit unique transcriptional signatures indicative of disease severity. Front. Immunol. 13, 989556. https://doi.org/10.3389/fimmu.2022.989556 (2022).
Thompson, R. C. et al. Molecular States during acute COVID-19 reveal distinct etiologies of long-term sequelae. Nat. Med. 29, 236–246. https://doi.org/10.1038/s41591-022-02107-4 (2023).
Juan Guardela, B. M. et al. 50-gene risk profiles in peripheral blood predict COVID-19 outcomes: A retrospective, multicenter cohort study. EBioMedicine 69, 103439. https://doi.org/10.1016/j.ebiom.2021.103439 (2021).
Lipman, D., Safo, S. E. & Chekouo, T. Integrative multi-omics approach for identifying molecular signatures and pathways and deriving and validating molecular scores for COVID-19 severity and status. BMC Genom. 24, 319. https://doi.org/10.1186/s12864-023-09410-5 (2023).
Sette, A. & Crotty, S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell 184, 861–880. https://doi.org/10.1016/j.cell.2021.01.007 (2021).
Merad, M., Blish, C. A., Sallusto, F. & Iwasaki, A. The immunology and immunopathology of COVID-19. Science 375, 1122–1127. https://doi.org/10.1126/science.abm8108 (2022).
Grifoni, A. et al. Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals. Cell 181, 1489-1501.e1415. https://doi.org/10.1016/j.cell.2020.05.015 (2020).
Kamanaka, M. et al. Memory/effector (CD45RB(lo)) CD4 T cells are controlled directly by IL-10 and cause IL-22-dependent intestinal pathology. J. Exp. Med. 208, 1027–1040. https://doi.org/10.1084/jem.20102149 (2011).
Crepaldi, L. et al. Up-regulation of IL-10R1 expression is required to render human neutrophils fully responsive to IL-10. J. Immunol. 167, 2312–2322. https://doi.org/10.4049/jimmunol.167.4.2312 (2001).
Chazen, G. D., Pereira, G. M., LeGros, G., Gillis, S. & Shevach, E. M. Interleukin 7 is a T-cell growth factor. Proc. Natl. Acad. Sci. U S A. 86, 5923–5927. https://doi.org/10.1073/pnas.86.15.5923 (1989).
Barata, J. T., Durum, S. K. & Seddon, B. Flip the coin: IL-7 and IL-7R in health and disease. Nat. Immunol. 20, 1584–1593. https://doi.org/10.1038/s41590-019-0479-x (2019).
Overmyer, K. A. et al. Large-Scale Multi-omic Analysis of COVID-19 Severity. Cell Syst 12, 23-40.e27. https://doi.org/10.1016/j.cels.2020.10.003 (2021).
Lodigiani, C. et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in milan, Italy. Thromb. Res. 191, 9–14. https://doi.org/10.1016/j.thromres.2020.04.024 (2020).
Loo, J., Spittle, D. A. & Newnham, M. COVID-19, immunothrombosis and venous thromboembolism: biological mechanisms. Thorax 76, 412–420. https://doi.org/10.1136/thoraxjnl-2020-216243 (2021).
Othman, H. Y., Zaki, I. A. H., Isa, M. R., Ming, L. C. & Zulkifly, H. H. A systematic review of thromboembolic complications and outcomes in hospitalised COVID-19 patients. BMC Infect. Dis. 24, 484. https://doi.org/10.1186/s12879-024-09374-1 (2024).
Piazza, G. et al. Registry of arterial and venous thromboembolic complications in patients with COVID-19. J. Am. Coll. Cardiol. 76, 2060–2072. https://doi.org/10.1016/j.jacc.2020.08.070 (2020).
Mohamed, M. F. H. et al. Prevalence of venous thromboembolism in critically ill COVID-19 patients: systematic review and Meta-Analysis. Front. Cardiovasc. Med. 7, 598846. https://doi.org/10.3389/fcvm.2020.598846 (2020).
Burn, E. et al. Venous or arterial thrombosis and deaths among COVID-19 cases: a European network cohort study. Lancet Infect. Dis. 22, 1142–1152. https://doi.org/10.1016/S1473-3099(22)00223-7 (2022).
Klok, F. A. et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 191, 145–147. https://doi.org/10.1016/j.thromres.2020.04.013 (2020).
Meisinger, C. et al. Elevated Plasma D-Dimer Concentrations in Adults after an Outpatient-Treated COVID-19 Infection. Viruses https://doi.org/10.3390/v14112441 (2022).
Al-Samkari, H. et al. COVID-19 and coagulation: bleeding and thrombotic manifestations of SARS-CoV-2 infection. Blood 136, 489–500. https://doi.org/10.1182/blood.2020006520 (2020).
Smilowitz, N. R. et al. C-reactive protein and clinical outcomes in patients with COVID-19. Eur. Heart J. 42, 2270–2279. https://doi.org/10.1093/eurheartj/ehaa1103 (2021).
Grint, D. J. et al. Severity of severe acute respiratory system coronavirus 2 (SARS-CoV-2) alpha variant (B.1.1.7) in England. Clin. Infect. Dis. 75, e1120–e1127. https://doi.org/10.1093/cid/ciab754 (2022).
Alefishat, E., Jelinek, H. F., Mousa, M., Tay, G. K. & Alsafar, H. S. Immune response to SARS-CoV-2 variants: A focus on severity, susceptibility, and preexisting immunity. J. Infect. Public. Health. 15, 277–288. https://doi.org/10.1016/j.jiph.2022.01.007 (2022).
Wolter, N. et al. Early assessment of the clinical severity of the SARS-CoV-2 Omicron variant in South africa: a data linkage study. Lancet 399, 437–446. https://doi.org/10.1016/S0140-6736(22)00017-4 (2022).
Monaco, G. et al. RNA-Seq Signatures Normalized by mRNA Abundance Allow Absolute Deconvolution of Human Immune Cell Types. Cell Rep 26, 1627-1640.e1627. https://doi.org/10.1016/j.celrep.2019.01.041 (2019).
Kalatskaya, I. et al. Revealing the immune cell subtype reconstitution profile in patients from the CLARITY study using Deconvolution algorithms after cladribine tablets treatment. Sci. Rep. 13, 8067. https://doi.org/10.1038/s41598-023-34384-5 (2023).
Baker, R. E. et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 20, 193–205. https://doi.org/10.1038/s41579-021-00639-z (2022).
Wiersinga, W. J. et al. Transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): A review. JAMA 324, 782–793. https://doi.org/10.1001/jama.2020.12839 (2020).
WHO. COVID-19: symptoms, (2023). https://www.who.int/westernpacific/emergencies/covid-19/information/asymptomatic-covid-19#:~:text=Symptoms%20of%20COVID%2D19%20can,should%20seek%20immediate%20medical%20attention>
Anders, S., Pyl, P. T. & Huber, W. HTSeq–a Python framework to work with high-throughput sequencing data. Bioinformatics 31, 166–169. https://doi.org/10.1093/bioinformatics/btu638 (2015).
Love, M. I., Huber, W. & Anders, S. Moderated Estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550. https://doi.org/10.1186/s13059-014-0550-8 (2014).
Wu, T. et al. ClusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innov. (Camb). 2, 100141. https://doi.org/10.1016/j.xinn.2021.100141 (2021).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30. https://doi.org/10.1093/nar/28.1.27 (2000).
Kanehisa, M., Sato, Y., Kawashima, M., Furumichi, M. & Tanabe, M. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res. 44, D457–462. https://doi.org/10.1093/nar/gkv1070 (2016).
Russo, P. S. T. et al. CEMiTool: a bioconductor package for performing comprehensive modular co-expression analyses. BMC Bioinform. 19, 56. https://doi.org/10.1186/s12859-018-2053-1 (2018).
Nadel, B. B. et al. The Gene Expression Deconvolution Interactive Tool (GEDIT): accurate cell type quantification from gene expression data. Gigascience https://doi.org/10.1093/gigascience/giab002 (2021).
Acknowledgements
We are extremely grateful of the invaluable support of this project by Prof Abdul Latif Al-Khal and Dr. Mohammed Ibn - Masud Danjuma from Hammad Medical Corporation. Their efforts, support and guidance were critical for timely approvals for sample acquisition and their kind inputs and support has improved the quality of our work. We sincerely appreciate their collaboration.
Funding
This study was supported by the QU internal Grant QUCG-CMED-21/22 − 2; and QU internal grant QUCG-CMED-24/25–424.
Author information
Authors and Affiliations
Contributions
AMA and FC conceived the study; AMA obtained the funding and supervised the work. AMA, FC, HR and MS designed and performed the experiments, did the analysis and interpretation of data. AMA wrote the manuscript. ANE, AD, SSS, FM, HY and FC contributed to patient recruitment, sample collection, handling and processing. Analysis and comments on various sections of the manuscript were provided by AMA, ARA, AD, ME, MS and FC. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The studies involving human participants were reviewed and approved by Hamad Medical Corporation and Qatar University. The patients/participants provided their written informed consent to participate in this study. In cases where patients were unable to provide informed consent due to any reason (unconsciousness, their medical condition, ventilatory support), the informed consent for study participation was obtained from their legally authorized representatives. The study protocol received approval from the Institutional Review Boards (IRBs) of HMC (MRC-05-136) and Qatar University (QU-IRB 1418-EA/20), including provisions for deferred consent when appropriate.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Abdallah, A.M., Ansari, H.R., Shuaib, M. et al. Immune transcriptomic analysis on COVID-19 patients with varying clinical presentations identifies severity markers. Sci Rep 15, 23416 (2025). https://doi.org/10.1038/s41598-025-04837-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04837-0