Abstract
Leishmaniasis, caused by the Leishmania parasites, is a significant global health issue with treatment challenges, particularly in endemic regions such as Iran. Current therapies, such as Meglumine antimoniate (MA), Amphotericin B, and Miltefosine, have limitations like high costs and side effects, necessitating innovative approaches. This study evaluates hydroxychloroquine (HC), an antimalarial drug with immunomodulatory properties, against Leishmania tropica (L. tropica), the causative agent of cutaneous leishmaniasis. We explored photodynamic therapy (PDT) and encapsulated HC in niosomal delivery systems with CdS/MIL-125(Ti) nanocomposites (FN) to enhance drug targeting. PDT utilizes these materials to produce reactive oxygen species, targeting cells effectively. Hydroxychloroquine-CdS/MIL-125(Ti)-loaded niosomes (NHC) were synthesized, characterized, and their in vitro anti-leishmanial activities were assessed alongside HC and MA. Results showed that NHC significantly improved anti-leishmanial effects, reducing viability in both promastigote and amastigote forms. Additionally, HC demonstrated favorable interactions with key proteins through molecular docking, modulated cytokine production, and induced apoptosis in infected macrophages. PDT further boosted the efficacy of both HC and NHC. This study indicates that niosomal encapsulation of HC enhances its delivery and efficacy, highlighting the potential for combination therapies in treating L. tropica. Further, in vivo studies are recommended to confirm these findings.
Similar content being viewed by others
Introduction
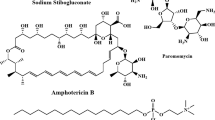
Leishmaniasis is a significant infectious disease caused by protozoa from the Leishmania genus that reside in skin, liver, spleen, and bone marrow macrophages. It manifests in three forms: cutaneous, mucosal, and visceral, and it affects over one billion people globally1. The Leishmania parasite exists as promastigotes in vector insects and amastigotes in a clinical stage in vertebrate hosts2,3. Current first-line treatments include drugs like Meglumine antimoniate (MA), Amphotericin B, and Miltefosine, but these can be expensive and lead to side effects and resistance4,5. Hence, they are not always the treatment of choice for this disease6. Thus, developing novel therapeutic options for leishmaniasis is crucial7.
Current treatments for leishmaniasis often fall short, highlighting the need for more effective and less toxic therapeutic options. Nanotechnology presents a promising approach for controlled drug release, potentially improving treatment efficacy and minimizing side effects8. This method could enhance treatment adherence, reduce outpatient care needs, and lower costs, which is crucial for rural and impoverished areas with limited healthcare access9. One notable application of nanotechnology is in photodynamic therapy (PDT), a minimally invasive treatment that utilizes photosensitizing agents activated by light to generate reactive oxygen species which destroy targeted cells10. Nanotechnology can help deliver these agents more precisely to affected areas, increasing treatment effectiveness while sparing healthy tissues. This could enhance treatment adherence and lower costs, which is crucial for rural and impoverished areas with limited healthcare access11.
Hydroxychloroquine (HC) is an antimalarial drug initially developed for malaria, now widely prescribed for autoimmune diseases like rheumatoid arthritis and systemic lupus erythematosus. As a chloroquine derivative, it inhibits heme polymerization and has immunomodulatory properties, which help reduce inflammation12. During the COVID-19 pandemic, its potential antiviral effects were explored, but research yielded mixed results regarding its effectiveness. Regulatory bodies, such as the FDA, stress the need for rigorous clinical trials13. While generally considered safe, HC can have side effects, including gastrointestinal issues, headaches, and skin reactions, as well as more serious risks like retinal toxicity with long-term use, warranting regular eye exams14.
Niosomes are effective drug delivery carriers that can hold a variety of drugs, including hydrophilic, hydrophobic, and amphiphilic compounds. They are easy to prepare, biodegradable, biocompatible, and non-immunogenic15,16. Niosomes enhance drug stability and provide controlled release, while also allowing for penetration through the skin and facilitating oral administration. Niosomes have a more straightforward preparation process, lower production costs, structural flexibility, and reduced toxicity compared to liposomes. The primary goal of these systems is to achieve optimal drug dosing, targeted delivery, favorable release properties, and high stability with minimal toxicity17.
In addition to niosomes, various drug carriers like dendrimers, micelles, and metal-organic frameworks (MOFs) are being explored for targeted drug delivery. In recent years, porous materials have demonstrated significant promise in nanocarrier drug delivery systems. Recent developments have shown that porous materials play a significant role in nanocarrier drug delivery, enhancing drug stability and facilitating controlled release. This integration of diverse carriers into complex systems promises to enhance the efficacy and safety of treatments18,19.
A notable study was conducted to assess the effect of HC on a composite material, CdS/MIL-125(Ti) (NHC), in the context of PDT. These findings indicate that it is a promising drug carrier, enhancing the delivery of HC against leishmaniasis. CdS/MIL-125(Ti)-HC developed nano-niosomes to improve drug absorption and delivery through the thin-layer evaporation technique. Additionally, the study employed computational methods to investigate the interactions of key proteins, including iNOS, Caspase 3, and Caspase 7, thereby identifying potential therapeutic strategies. Incorporating in vitro analysis further strengthens the validation of these findings, highlighting the potential of PDT as a viable treatment option for leishmaniasis.
Materials and methods
Drugs and reagents
HC, CAS no. 747-36-4, was procured from Sigma (Germany). MA was obtained from Sanofi-Aventis, France. Drug dilutions were prepared in distilled water and were sequential concentrations of 12.5, 25, 50, 100, 200, and 400 µM.
Synthesis and characterization of nanocomposites
To prepare MIL-125(Ti), a mixture of 15 mmol of 2-hydroxy terephthalic acid and 9 mmol of tetra-n-butyl titanate was dissolved in 50 mL of anhydrous DMF and methanol (9:1) and heated at 150 °C in a Teflon-lined autoclave for 20 h. After cooling, the white precipitate was collected, rinsed with DMF and methanol, and dried. The synthesis of CdS on MIL-125(Ti) was performed using Wang’s method: 200 mg of activated MIL-125 was mixed with 10 mL of ammonium sulfide and 20 mL of hexane. Cadmium nitrate was added, and the mixture was heated at 180 °C for 12 h. The yellow powders were then collected, cleaned, and dried in a vacuum at 60°CTo optimize the drug’s efficacy and absorption, we created niosomes and HC nano-niosomes through the thin-layer evaporation technique20,21. For drug optimization, we created niosomes and HC nano-niosomes using Span 60, Tween 60, and cholesterol as surfactants22,23. The ingredients were dissolved in chloroform, evaporated under vacuum at 60 °C, and the thin lipid layer was placed in an aqueous solution (pH 7) at 60 °C for 60 min. The suspension was equilibrated at room temperature for 12 h, sonicated for 15 min, filtered through 0.44 μm and 0.22 μm membranes, and centrifuged for 30 min. Samples were stored at 4 °C for testing.
The classification parameters of niosomes are vital for their stability and efficacy in vivo. Key features, including morphology, zeta potential, particle size, encapsulation stability, and entrapment efficiency, are assessed to optimize formulations. Morphological and size characteristics are evaluated using dynamic light scattering (DLS) and transmission electron microscopy (TEM)24,25. DLS provides particle size distribution data, while TEM offers high-resolution images of surface structure. Zeta potential and particle size are measured with a Zeta-sizer, where a negative zeta potential indicates stability and a low polydispersity index (PDI) signifies uniformity25,26. Entrapment efficiency (EE%) quantifies the drug encapsulated, determined through centrifugation and subsequent drug release using methanol, analyzed via UV spectrophotometry at 343 nm27. In vitro drug release profiles are assessed using a dialysis method with niosomes in phosphate-buffered saline (PBS) at 37 °C, with samples collected for analysis of drug release kinetics28,29.
In silico study
This study aimed to screen HC for an effective antileishmanial compound through molecular docking with iNOS, Caspase 3, and Caspase 7. The 3D structures of HC were sourced from PubChem, and the target proteins were prepared using crystal structures from the Protein Data Bank (PDB).
The preparation of receptors and ligands was conducted via the default 3D protonation procedure in Molecular Virtual Docking (MVD)30. Active sites on iNOS, Caspase 3, and Caspase 7 were identified for docking with HC. The best ligand-target poses were selected based on the lowest energy, followed by data analysis using Discovery Studio and PyMOL, resulting in the optimal composite from each dataset.
In vitro study
PDT
This study utilized advanced LED light sources emitting 83 mW at 470 nm. A total energy of 50.99 J was delivered over a 4 cm² area, 15 cm from the target, yielding an energy density of 12.74 J/cm². The goal was to identify the most effective photodynamic therapy for Leishmania. The research pinpointed the NHC nanocomposite region with the highest production of free radicals and active oxygen species, enabling the selection of the optimal light source for improved therapeutic outcomes in both in vitro and in vivo testing31.
Parasite and macrophage culture
The Kerman Leishmaniasis Research Center provided the standard strain (MHOM/IR/Mash2) of L. tropica promastigotes, which were cultivated in RPMI-1640 medium (Biosera, France) with penicillin-streptomycin and 10% fetal bovine serum (Sigma, USA) at 25 ± 1˚C. The THP-1 human macrophage cell line, obtained from the Pasteur Institute in Tehran, Iran, was cultured in DMEM medium (Sigma, USA) with penicillin, 0.5% streptomycin (Biosera, France), and 10% FBS (Sigma, USA) at 37˚C in a 5% CO2 atmosphere. Differentiation into macrophage-like cells (MLCs) was induced using phorbol 12-myristate 13-acetate (PMA).
The study included several experimental and control groups to evaluate various treatments has been summarized in Table 1. This diverse range of groups allows for a comprehensive analysis of treatment efficacy and mechanisms.
Anti-promastigote activity
To evaluate the anti-promastigote activity of HC, NHC, and MA, with and without light exposure, two complementary assays, MTT and Trypan Blue exclusion, were conducted on L. tropica promastigotes. Promastigotes in the logarithmic growth phase (1 × 10⁵ cells/mL) were seeded into 96-well plates. Treatments with various concentrations of HC, NHC, and MA were applied in both light and dark conditions. For the Trypan Blue assay, promastigotes were incubated for 24 h at 25 ± 1 °C. Following this period, 10 µL of the treated culture was mixed with 10 µL of 0.4% Trypan Blue solution and incubated at room temperature for 5 min. The number of viable (unstained) and dead (blue-stained) cells was counted using a hemocytometer under a light microscope32. In parallel, the MTT assay was performed by incubating treated promastigotes for 72 h under the same conditions. After this incubation, 10 µL of MTT solution (5 mg/mL) was added to each well, and plates were incubated for an additional 3 h. Then, 100 µL of DMSO was added to dissolve the formazan crystals. The absorbance was measured at 530 nm using a Bio-Tek ELISA reader. The 50% inhibitory concentration (IC₅₀) values were calculated using SPSS software.
Anti-amastigote activity
MLC was cultivated on a glass slide at a concentration of 105 per milliliter and incubated for 24 h at 37˚C with 5% CO2. They were then supplemented with 106 stationary phase promastigotes at a 10:1 ratio, allowing a 24-hour transformation into amastigotes. Various concentrations of MAT, CVL, and their combination (50, 100, 200, and 400 µg/mL) were added and incubated for 72 h. After drying, samples were methanol-fixed and stained with Wright-Giemsa. IC50 values for the amastigotes were calculated by averaging the number of amastigotes in 100 macrophages.
Cytotoxicity
To evaluate the cytotoxicity of MLC, HC, NHC, and MA at concentrations of 50, 100, 200, and 400 µg/mL, cells were incubated with these compounds for 72 h at 37˚C in a 5% CO2 atmosphere within 96-well plates. Afterward, 10 µL of MTT solution was added for 3 h, followed by 100 µL of DMSO. The OD was measured at 530 nm using a Bio-Tek ELISA reader. Each concentration was tested in triplicate against an untreated control (UC) group. The selectivity index (SI) was calculated using the formula SI = IC50/CC50 (the 50% Cytotoxic concentration); an SI greater than 1 indicates minimal toxicity.
Cytokines measurement
The supernatants from each well in the treated and untreated sets were used to assess the levels of cytokines, including TNF-α, IFN-γ, IL-12, IL-4, IL-10, and TGF-β through ELISA, the manufacturer’s procedures (Karmania Pars Gene, Kerman, Iran). The plates were examined at 450 nm using an ELISA reader.
Annexin V/PI and flow cytometry
Apoptosis in treated intramacrophage amastigotes was assessed using a flow cytometry assay with the Apoptosis Detection Kit (Bioscience, USA). Six million L. major promastigotes in the logarithmic phase were treated with varying concentrations of HC, NHC, and MA, with or without light exposure, and incubated for 72 h. Samples were washed and resuspended in phosphate-buffered saline (PBS) and 1X binding buffer, followed by the addition of 5 µL of V-FITC and 5 µL of propidium iodide (PI) solution. After a 20-minute dark incubation at room temperature, apoptosis was evaluated using flow cytometry (BD FACS Calibur, USA).
Quantitative real-time PCR
Quantitative real-time PCR was performed to compare expression levels of IFN-γ, IL-12 p40, iNOS, TGF-β, and IL-10 in drug-exposed intra-macrophage amastigotes (Table 2). Total RNA was extracted using the Qiagen RNeasy Mini Kit and assessed for quality and concentration using a NanoDrop spectrophotometer. cDNA synthesis was achieved using the Prime Script™ RT reagent kit, with reverse transcription conducted at 37 °C for 20 min using 0.5 µg of RNA. Takara SYBR® Premix Ex TaqTM II was utilized for qPCR, run in duplicate on the Qiagen Rotor-Gene Cycler. The PCR conditions included an initial hold at 95 °C for 1 min, followed by 40 cycles of denaturation, annealing, and extension, and analyzed using the 2-ΔCt method, with GAPDH as a reference gene.
Reactive oxygen species (ROS) production
The intracellular production of Reactive Oxygen Species (ROS) in treated intra-macrophages amastigotes was evaluated using the fluorescent probe 2’,7’-dichlorodihydrofluorescein diacetate (DCFH − DA) and analyzed by flow cytometry. Specifically, 106 L. tropica intra-macrophages amastigotes in the logarithmic phase were treated with different concentrations of HC, NHC, and MA with and without light administration, followed by a 72 h incubation period. After incubation, the samples were washed with PBS. The cells were then resuspended in a solution containing 10 µM of the DCFH − DA probe and incubated for 30 min at 37 °C in the dark. Finally, the intensity of green fluorescence, which corresponds to the level of ROS, was measured using a flow cytometer (BD FACS Calibur, USA).
Statistical analyses
SPSS v. 22 and GraphPad Prism v.10.0 were used for statistical analysis by employing a paired t-test and one-way ANOVA. A P value threshold of < 0.05 was considered significant.
Results
Characterization of nanocomposites
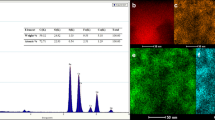
Table 3 summarizes the mean diameters of both unloaded and NHC, along with parameters such as PDI, NHC EE%, and zeta potential values. DLS measurements, as illustrated in Figs. 1 a and b, reveal that the size of unloaded vesicles ranges from 6 to 12 nm. At the same time, incorporating NHC increases the hydrodynamic diameter, reaching between 10 and 60 nm. The surface charge of nanoparticles is a crucial factor in their interactions with cells. Generally, charged nanoparticles exhibit enhanced internalization compared to their uncharged counterparts33. Positively charged nanoparticles enhance uptake, whereas negatively charged nanoparticles do not facilitate this process.
The synthesized unloaded niosomes and NHC demonstrated zeta potential values of -8.33 and − 2.95, respectively, indicating stable colloidal suspensions due to adequate electrostatic repulsion (Table 3).
Figure 2 a shows TEM images of NHC at 50 nm scales, revealing a semi-spherical morphology with a core and layered structure. Additionally, Fig. 2 b offers a histogram of particle sizes of NHC, indicating that the majority of the particles are smaller than 20 nm. This small size is crucial as it greatly influences their reactivity potential and enhances their performance in various applications, such as drug delivery systems and catalytic processes.
The cumulative in vitro release profiles of free HC and NHC were evaluated in PBS (pH 7.4) at 37 °C over 48 h. As shown in Fig. 3, free HC exhibited a rapid release pattern, reaching approximately 92% within the first 2 h and plateauing at around 99% by 24 h. In contrast, the NHC formulation demonstrated a biphasic release behavior. An initial burst release of 30% was observed within the first 0.5 h, followed by a sustained and gradual release, reaching approximately 80% after 48 h. This controlled release suggests that HC was efficiently encapsulated within the niosomal matrix and released over time in a diffusion-controlled manner.
Docking study
A comprehensive molecular docking analysis was performed on HC concerning the receptors iNOS, Caspase 3, and Caspase 7, utilizing the selected crystal structures of 4NOS, 5IAE, and 2QL7, respectively. The detailed docking procedures involved an in-depth assessment of the binding energies using MolDock Scores, which indicate the binding affinity and efficiency of these interactions. Negative energy values signify spontaneous binding events, suggesting a favorable binding process between the compounds and their respective receptors. The molecular docking findings for HC interacting with the iNOS, Caspase 3, and Caspase 7 receptors yielded MolDock Scores of -124.86, -108.02, and − 115.43, respectively, illustrating that HC exhibits a substantial binding potential with these targets. Figure 4 visually summarizes the data obtained from the docking analysis, showcasing the ligand binding maps along with the specific molecular interactions of HC with the iNOS, Caspase 3, and Caspase 7 receptors. The docking analysis elucidated that HC engages in critical interactions with distinct amino acid residues of the iNOS receptor, including Leu(A)125, Trp(A)194, Ala(A)197, Arg(A)199, Cys(A)200, Asp(A)370, Phe(A)488, and Tyr(A)489, as represented in Fig. 4 a. These specific interactions are crucial for the modulating iNOS activity, which is known to play a significant role in inflammatory responses. In terms of the Caspase 3 receptor, HC demonstrated binding interactions at the specific binding site, involving key amino acid residues such as Arg(A)64, His(A)121, Gly(A)122, Cys(A)163, Ser(A)205, and Trp(A)206. These multifaceted interactions are critical for the receptor’s function in apoptosis and cell survival, as depicted in Fig. 4 b.
Furthermore, this report presents the findings from the molecular docking analysis regarding HC’s interaction with the Caspase 7 receptor. Figure 4 c illustrates the ligand interaction maps and the molecular docking configurations of HC bound to the Caspase 7 protein structure. The analysis indicates that HC forms significant interactions with several pivotal amino acid residues, namely Trp(A)232, Arg(A)233, Arg(A)237, Phe(A)273, and Glu(A)274. These interactions imply that HC could effectively alter the conformational dynamics of the iNOS, Caspase 3, and Caspase 7 receptors. A thorough understanding of these ligand-receptor dynamics is essential for the rational design and development of novel therapeutic agents targeting the activity of iNOS, Caspase 3, and Caspase 7. This knowledge will ultimately contribute to the development of more targeted and effective treatment strategies for diseases such as leishmaniasis.
Anti-promastigote functions
The effect of varying HC, NHC, and MA concentrations on promastigote viability after 24 h for trypan blue and 72 h for MTT assay of treatment was analyzed (Fig. 5). All treatment groups significantly reduced promastigote survival compared to the control group (p < 0.001). Combining the two drugs enhanced efficacy more than when administered separately (p < 0.01). A dose-dependent response was noted, with increased concentrations leading to lower viability. Additionally, light exposure improved lethality for specific concentrations of HC and MA. These results suggest that combining HC, NHC, and MA, especially with light, may offer a promising treatment strategy for Leishmaniasis, highlighting the need for further research into the underlying mechanisms and clinical potential. The IC50 values of all treatments, as well as the MTT and trypan blue assay results, are demonstrated in Table 5.
Anti-amastigote assessment
In addition to the significant reduction in amastigote counts, the study also assessed the cytotoxicity of HC, NHC, and MA on macrophages to ensure that the observed effects were not due to harmful effects on the host cells (Table 4). Cell viability assays demonstrated that even at higher concentrations, these compounds did not significantly reduce macrophage viability compared to the UC group, confirming their safety profile. Furthermore, analysis of the mechanism of action revealed that these compounds may enhance the phagocytic activity of macrophages, allowing for increased clearance of the amastigotes. Flow cytometry data supported this, indicating increased expression of surface markers associated with activation.
Cytotoxic
Our study reveals key insights into the cytotoxic effects and interactions of HC, NHC, and MA. As illustrated in Table 5 under illuminated conditions, HC exhibited the highest selective index (SI), indicating strong potent cytotoxicity with minimal harm to healthy cells. Tryptan blue exclusion assays confirmed that the viability of healthy cells remained high in the presence of HC, further supporting its potential for safe therapeutic application. NHC showed a moderate SI, balancing efficacy and safety, and the tryptan blue results indicated a reasonable level of cell viability, suggesting it could be beneficial in certain contexts. Meanwhile, MA’s lower SI suggests a need for optimization, as the tryptan blue results indicated a more significant impact on healthy cell viability.
Analysis of the combination index (CI) revealed that HC and NHC together produced a synergistic effect (CI < 1), enhancing therapeutic efficacy and promoting cancer cell apoptosis. Tryptan blue assays confirmed that this combination resulted in reduced viability in cancer cells while maintaining acceptable levels of healthy cell viability. In contrast, the NHC and MA combination showed an antagonistic interaction (CI > 1), potentially diminishing treatment effectiveness, and tryptan blue results revealed a concerning impact on cell viability in healthy cells.
These findings underscore the impact of light conditions on cytotoxicity and the need for careful drug combination strategies in therapy, laying the groundwork for future research to refine treatment protocols and achieve improved patient outcomes.
M1 and M2 type cytokines
The study provides evidence of the leishmanicidal effects of HC, NHC, and MA on macrophage activity, shown through cytokine level analysis (Figs. 6 and 7). Experiments under varying light conditions revealed differing efficacy levels among treatments, suggesting ways to enhance therapeutic strategies against leishmaniasis by modulating immune responses. HC and NHC significantly increased pro-inflammatory cytokine production compared to the UC group, promoting M1 macrophage polarization, while MA had a lesser effect. Light further enhanced cytokine production in response to HC and NHC, indicating its role in boosting leishmanicidal activity through modulation of macrophage function. The findings highlight the potential of cytokine modulation to improve treatment outcomes for leishmaniasis.
Effects of HC, NHC, and MA with and without light exposure on intra-macrophage L. tropica amastigotes in comparison to the gene expression of M1 macrophage-related cytokines (iNOS, TNF-α, IL-4) and M2 macrophage-related cytokines (IL-12, IFN-γ, TGF-β) compared to the UC group. Statistical significance is indicated as follows: # (P < 0.001 vs. MA), @ (P < 0.001 between HC and NHC), & (P < 0.001 between HC or NHC with and without light exposure).
Effects of HC, NHC, and MA with and without light exposure on intra-macrophage L. tropica amastigotes in comparison to the gene expression on the mean level of M1 macrophage-related cytokines (iNOS, TNF-α, IL-4) and M2 macrophage-related cytokines (IL-12, IFN-γ, TGF-β) compared to the UC group. Statistical significance is indicated as follows: # (P < 0.001 vs. MA), @ (P < 0.001 between HC and NHC), & (P < 0.001 between HC or NHC with and without light exposure).
Apoptotic mediators
The study evaluated the impact of HC, NHC, and MA on key apoptotic mediators, including Bax, Bcl-2, and Caspase 3, under both light and dark conditions. In the presence of light, both HC and NHC significantly increased Bax levels, indicating enhanced pro-apoptotic signaling, with HC exhbiting higher levels than NHC (P < 0.001). Bcl-2 levels decreased in the HC group compared to the NHC and MA groups, reinforcing the apoptotic effect of HC. Caspase 3 activation was also significantly higher in HC and NHC compared to UC group (P < 0.001), whereas MA had a lesser impact. Under dark conditions, HC and NHC still promoted apoptosis, but to a lesser degree. Both treatments outperformed MA significantly (P < 0.001). These findings underscore the influence of environmental factors on apoptotic pathways in L. tropica amastigotes, highlighting potential therapeutic strategies for related infections. Figure 8 illustrates the enhanced apoptotic effects of HC and NHC compared to MA.
Effect of HC, NHC, MA alone, with and without the light on intra-macrophages L. tropica amastigotes on gene expression (UP) and mean level of apoptotic mediator (DOWN) including Bax, Bcl-2, and Caspase 3 compared to the UC group (# (P < 0.001 vs. MA),@ (P < 0.001 between HC vs. NHC),& (P < 0.001 between HC or NHC with and without Light).
Apoptotic profiles
Our findings show that treatments with HC, NHC, and MA significantly increased apoptosis in intramacrophage amastigotes compared to UC group. HC and NHC notably enhanced phosphatidylserine externalization, a marker of early apoptosis, while PI staining confirmed the presence of late apoptosis and necrosis. HC exhibited a superior apoptotic effect over NHC (p < 0.001), with light further enhancing the efficacy of both treatments. Although MA was effective, it did not achieve the same level of apoptotic induction as HC or NHC in the presence of light. These results highlight the potential of HC and NHC, particularly in the context of light exposure, as promising strategies for inducing apoptosis in relevant infections. Figure 9 illustrates the statistical significance of each treatment compared to controls, underscoring the value of combining light-activated therapies with pharmacological agents.
ROS production
In our flow cytometry assay, we observed a significant increase in ROS production with HC and NHC compared to the control group (Fig. 10). Notably, their combination with light exposure led to even higher ROS levels, indicating a synergistic effect that amplifies oxidative stress. Conversely, while MA also increased ROS levels in light, its impact was less pronounced and negligible in the absence of light. The highest oxidative stress was associated with HC and NHC under illuminated conditions, highlighting their pro-oxidative properties. These findings highlight the role of environmental factors in oxidative stress responses and suggest potential therapeutic avenues for mitigating oxidative damage.
Discussion
The synthesized niosomal nanocomposites were characterized using various techniques to assess size distribution, surface charge, morphology, and encapsulation efficiency. DLS analysis indicated that the average hydrodynamic diameter of the NHC was in the nanometric range, which is advantageous for cellular uptake and passive targeting via the EPR effect34. TEM confirmed the spherical morphology and relatively uniform size distribution of the nanovesicles, with images revealing a semi-spherical structure with a core-layered design at scales around 50 nm35. DLS also showed that the unloaded niosomes ranged from 6 to 12 nm in size, whereas the incorporation of NHC significantly increased the hydrodynamic diameter, resulting in sizes between 10 and 60 nm. The zeta potential measurements further elucidated that the unloaded niosomes had a moderately negative charge of -8.33 mV, while NHC had a reduced negative charge of -2.57 mV, indicating a shift towards a more neutral surface. This effect on surface charge contributes to colloidal stability by preventing particle aggregation through electrostatic repulsion36. The stability of the colloidal suspension was supported by the DLS results, with adequate electrostatic repulsion evident from the PDI and zeta potential values. The TEM images provided high-resolution visual confirmation of the particle morphology, reinforcing the DLS size measurements. The histogram analysis from TEM indicated that most NHC particles were smaller than 20 nm, highlighting their compact size, which suggests enhanced reactivity and performance in applications such as drug delivery37.
Furthermore, the EE% of HC within the niosomes was found to be satisfactory, supporting the suitability of the formulation for efficient drug loading. Although UV–Vis spectrophotometry was employed for EE% determination16,38,39, future work may benefit from the use of more sensitive analytical methods, such as HPLC, to improve accuracy and quantitation, especially in complex matrices40,41. Collectively, the characterization results confirm the successful fabrication of stable, nanosized NHC with appropriate physicochemical properties for drug delivery applications.
The molecular docking analysis was performed to gain mechanistic insights into the interaction between hydroxychloroquine and key Leishmania target proteins. The binding affinity results revealed favorable docking scores, suggesting that HC can form stable complexes with the active sites of the selected protein targets. These interactions were primarily stabilized through hydrogen bonding and hydrophobic interactions, indicating a potential for inhibitory activity39,42,43.
The in silico findings support the experimental observations of anti-leishmanial activity, providing a theoretical basis for the therapeutic effect of HC. Docking analysis further underscores the relevance of specific residues in the target site and offers a platform for future optimization of drug-target affinity44,45. While docking studies provide valuable preliminary data, it is important to note their limitations, including reliance on static protein structures and the absence of dynamic biological context. Nevertheless, these computational insights complement the in vitro findings and strengthen the case for HC as a candidate for repurposing against leishmaniasis, particularly in its niosomal nanoformulated form39.
The drug release profile of the NHC formulation confirms its potential for sustained drug delivery. The observed initial burst may be attributed to HC adsorbed on or near the surface of the vesicles, while the prolonged release phase indicates that a significant fraction of the drug was entrapped within the bilayer or aqueous core of the niosomes. This biphasic pattern is consistent with previous studies on niosomal systems, which are known to provide controlled release through both diffusion and erosion mechanisms. In contrast, the free drug exhibited a rapid release, which may lead to fluctuating plasma levels and increased risk of toxicity in vivo. The sustained release of HC from NHC can potentially maintain therapeutic drug levels for extended periods, reduce dosing frequency, and enhance patient compliance important factors in the treatment of chronic infections such as leishmaniasis46,47.
The results provide compelling evidence for the effectiveness of HC, NHC, and MA in reducing promastigote viability, both individually and in combination. The statistically significant reduction in survival rates across all treatment groups compared to the control (p < 0.001) confirms the potent anti-promastigote activity of these compounds. The dose-dependent trend observed with each drug indicates that increasing concentrations correlate with greater parasite lethality, highlighting the concentration-specific pharmacological potential of these agents. A particularly noteworthy finding is the synergistic effect observed when HC and NHC were combined with MA. The combination therapy demonstrated significantly greater promastigote killing than the individual treatments alone (p < 0.01), suggesting potential interaction mechanisms that enhance anti-leishmanial efficacy. Such synergism could allow for lower effective doses of each drug, potentially reducing toxicity and side effects while maintaining or enhancing therapeutic outcomes48.Another critical aspect of the study is the role of light exposure. Specific concentrations of HC and MA were significantly more effective in reducing promastigote viability under light conditions, implying a photosensitizing or photodynamic enhancement of their activity. This opens up avenues for PDT strategies in leishmaniasis treatment42, a concept that has gained interest for its selective cytotoxic effects against pathogens and tumor cells. These findings suggest that the combination of HC, NHC, and MA, particularly when administered under light, represents a promising anti-leishmanial strategy. Further investigations are needed to elucidate the underlying mechanisms of their synergistic and light-enhanced effects, including potential impacts on parasite metabolism, oxidative stress pathways, and drug uptake. Moreover, in vivo studies and clinical evaluations will be essential to assess the safety, efficacy, and translational potential of this combination therapy38,49.
The current study demonstrates the significant effect of HC, NHC, and MA against intracellular amastigotes, with marked reductions in parasite load observed across increasing concentrations of each compound. These activities were consistent in both light and non-light conditions, with the most pronounced reductions observed at higher concentrations, particularly with NHC and in light-enhanced conditions. This dose-dependent decline in amastigote numbers underlines the potency of these treatments and supports their potential therapeutic utility. Importantly, cytotoxicity assessments revealed no significant reduction in macrophage viability, even at the highest concentrations tested. This indicates that the anti-amastigote activity of HC, NHC, and MA is not due to macrophage death, but rather a direct or immune-mediated action on the intracellular parasites. The favorable safety profile of these compounds enhances their appeal for clinical application, especially when compared with traditional therapies that often exhibit higher host toxicity50,51,52.
A striking observation was the enhanced efficacy of NHC compared to HC across all concentrations, suggesting that the niosomal formulation significantly improves the drug’s bioavailability or intracellular delivery. This is further supported by statistically significant differences between the HC and NHC groups (p < 0.001), confirming the advantage of nanoencapsulation in targeted drug delivery strategies. Furthermore, treatments under light exposure (NHC + L and HC + L) demonstrated significantly greater reductions in amastigote burden than those in the absence of light (p < 0.001). This photodynamic enhancement may be attributed to increased ROS generation or structural alterations in the drug that augment its anti-parasitic activity. Among all treatments, NHC + L exhibited the strongest amastigote clearance, reducing counts to zero at the highest tested concentration (400 µg/mL), thereby highlighting the potential of photochemotherapy when combined with optimized drug delivery systems8,53,54,55.
The study also explored the possible immune mechanisms underlying these effects. Flow cytometry analysis suggested increased expression of activation markers on macrophage surfaces, indicative of enhanced phagocytic activity39. This suggests that these compounds may act directly on amastigotes and modulate host cell function to boost pathogen clearance. Collectively, the data strongly support the potential of NHC, particularly in combination with light exposure, as a highly effective and safe anti-leishmanial agent. The use of light-responsive formulations and nanocarriers such as niosomes could represent a next-generation strategy for enhancing the efficacy and targeting of anti-leishmanial therapies. Further in vivo validation and mechanistic studies are warranted to fully harness the benefits of this approach and translate it into clinical settings.
The cytotoxicity assessment of HC, NHC, and MA provides crucial insight into the safety and therapeutic potential of these agents, particularly when considering their use in treating intracellular parasitic infections such as L. tropica. The SI, calculated as the ratio of CC50 in macrophages to IC50 in parasites, serves as a key metric in determining the therapeutic window and overall safety of the compounds. Among the tested agents, HC + L and NHC + L exhibited the highest SI values, with NHC + L achieving an SI of 9.84, the most favorable in the study. This suggests a superior safety profile and strong selectivity toward parasitic cells over host macrophages under light exposure. These findings reinforce the earlier evidence of light-enhanced efficiency, likely due to a photodynamic mechanism that improves drug activation or parasite sensitivity. Similarly, NHC alone demonstrated an SI of 7.02, outperforming MA (6.52) and HC (4.13), indicating that the niosomal formulation of HC enhances its therapeutic selectivity, possibly by improving cellular uptake or controlled release. Interestingly, although MA is a commonly used treatment, it exhibited the lowest SI values across both promastigote and amastigote stages, suggesting a narrower safety margin. This supports the argument for exploring alternative or adjunctive therapies, particularly those with more favorable cytotoxic profiles, such as NHC or its light-activated counterpart54,56.
Analysis of CI further revealed important drug interaction patterns57. The combination of HC and NHC produced CI values below 1, indicating synergistic interactions that could enhance treatment efficacy while possibly allowing dose reductions, thereby minimizing toxicity. In contrast, the NHC + MA combination showed CI values greater than 1, indicating antagonism, which suggests that this pairing may reduce therapeutic benefit and should be avoided or optimized with caution.
These findings also underscore the critical role of light as a modulator of both efficacy and safety. The improved SI values under illumination suggest that photo-responsive strategies may offer a safe and highly effective approach for treating leishmaniasis, particularly when combined with nano-based delivery systems, such as niosomes. Overall, the data confirm the promising safety and therapeutic profiles of HC and NHC, especially under light-enhanced conditions, and highlight the importance of strategic drug pairing to avoid antagonistic effects50,58. Further in vivo studies and pharmacokinetic analyses will be essential to validate these findings and refine optimal treatment combinations for clinical application.
The study demonstrates that HC, NHC, and MA modulate macrophage immune responses by promoting a shift toward the M1 phenotype, characterized by increased production of pro-inflammatory cytokines. Both HC and NHC significantly upregulated M1-associated cytokines compared to the UC group, with NHC showing the most potent effect, particularly under light exposure. This suggests that these compounds, especially in photo-activated conditions, exert direct leishmanicidal effects and enhance host immune responses against L. tropica. MA also induced cytokine production but to a lesser extent, indicating a relatively milder immunostimulatory profile. These findings highlight the dual role of HC and NHC as both antiparasitic and immunomodulatory agents, paving the way for therapies that combine direct pathogen killing with host-directed immune activation to enhance treatment outcomes in leishmaniasis38,51.
This study highlights the apoptotic potential of (HC, its NHC, and MA against L. tropica amastigotes by examining the gene expression of key apoptotic regulators: Bax, Bcl-2, and Caspase 3. The findings reveal a significant modulation of apoptosis-related pathways by HC and NHC, particularly under light exposure, emphasizing the role of both drug formulation and environmental conditions in driving cell death. A notable upregulation of the pro-apoptotic gene Bax was observed in HC- and NHC-treated groups, with HC showing a significantly higher expression than NHC (P < 0.001). The enhanced Bax expression suggests mitochondrial involvement and activation of the intrinsic apoptotic pathway, particularly under illuminated conditions. In parallel, Bcl-2, an anti-apoptotic marker, was markedly downregulated in HC-treated cells compared to both NHC and MA groups, further confirming the pro-apoptotic bias induced by HC 42,49.
The activation of Caspase 3, a key executor of apoptosis, was also significantly elevated in both HC and NHC groups relative to the UC group (P < 0.001)59. This indicates the successful progression of apoptosis beyond initiation, with the formation of apoptotic bodies likely contributing to the clearance of the parasite. In contrast, MA showed a relatively modest impact on all three apoptotic markers, aligning with its less pronounced ability to trigger programmed cell death. Interestingly, while the pro-apoptotic effects of HC and NHC persisted in dark conditions, the overall magnitude was slightly attenuated, suggesting that light may enhance drug activation or cellular sensitivity to apoptosis, possibly through a photodynamic mechanism. Nevertheless, both formulations exhibited significantly higher expression of apoptotic mediators than MA, reinforcing their intrinsic pro-apoptotic capabilities60.
Collectively, these results emphasize the superior pro-apoptotic activity of HC and NHC over MA, with light exposure amplifying these effects. The data support the notion that inducing apoptosis in intracellular amastigotes via host-directed mechanisms may be a practical therapeutic approach. The incorporation of nanoformulations, such as NHC, and the potential of light-enhanced strategies could represent a novel direction in anti-leishmanial drug development, warranting further in vivo validation and mechanistic exploration.
The apoptotic profiles observed in this study provide strong evidence for the efficacy of HC, its NHC, and MA in inducing programmed cell death in L. tropica amastigotes within macrophages. The data reveal a significant increase in both early and late apoptotic markers following treatment, highlighting the therapeutic potential of these compounds in targeting intracellular forms of the parasite. A key indicator of early apoptosis, phosphatidylserine externalization, was markedly elevated in the HC and NHC treatment groups, suggesting active engagement of apoptotic pathways. This effect was further corroborated by PI staining, which revealed plasma membrane compromise, a hallmark of late-stage apoptosis and necrosis. These dual-phase findings confirm that the treatments not only initiate apoptotic signaling but also drive it to completion.
Among the treatments, HC exhibited the strongest pro-apoptotic activity, significantly outperforming NHC (p < 0.001). This may be attributed to HC’s superior membrane permeability or intracellular accumulation, leading to a more robust apoptotic cascade61. However, the use of NHC still showed considerable efficacy and offers the added benefits of controlled drug delivery and reduced systemic toxicity, which are essential considerations for therapeutic application. Importantly, light exposure significantly enhanced the apoptotic effect of both HC and NHC, as shown by higher percentages of apoptotic amastigotes in illuminated conditions (p < 0.001). This enhancement may result from photodynamic interactions that potentiate oxidative stress or activate photoresponsive pathways in the parasite or host cells, further driving apoptotic processes. These findings support the growing body of research advocating for light-assisted therapies as adjuncts to conventional pharmacological treatments. In contrast, MA induced apoptosis to a lesser extent and did not achieve the same level of effectiveness as either HC or NHC under illuminated conditions. This comparatively lower efficacy suggests that while MA retains anti-leishmanial activity, its mechanism may rely less on apoptosis induction and more on other modes of inhibiting the parasite .
Overall, the results highlight the superior ability of HC and NHC, particularly under light exposure, to initiate and sustain apoptosis in intramacrophage L. tropica amastigotes. These findings underscore the potential of HC-based therapies in treating leishmaniasis, while also highlighting the promising role of light-activated delivery systems in enhancing anti-parasitic efficacy. Future studies should further explore the mechanistic underpinnings of this light-enhanced apoptosis and assess its translational potential in vivo.
The current study demonstrates a clear link between treatment with HC, its NHC, and increased production of ROS in L. tropica-infected macrophages. These findings underscore the crucial role of oxidative stress in mediating the anti-leishmanial effects of these compounds and highlight the impact of environmental factors, exceptionally light exposure, on modulating this response. Flow cytometry analysis revealed that HC and NHC significantly elevated intracellular ROS levels compared to the UC group. This ROS upregulation indicates the activation of mitochondrial or NADPH oxidase, leading to enhanced oxidative stress that can contribute to parasite damage and apoptosis. The greater ROS induction observed with NHC compared to HC, particularly under light conditions, may be attributed to improved cellular uptake or controlled drug release properties associated with the niosomal formulation, which enhances intracellular drug bioavailability.
The effect of light exposure on ROS production was particularly striking. HC and NHC treatments under illuminated conditions produced the highest ROS levels, indicating a synergistic interaction between the drug’s action and photodynamic mechanisms. This could be due to light-induced activation of photosensitive drug intermediates, resulting in augmented ROS generation and oxidative stress. These findings are consistent with previous studies on photochemotherapy, supporting the therapeutic potential of light-enhanced drug regimens for intracellular pathogens such as Leishmania7,8,53,54,62,63. In contrast, MA exhibited a more modest capacity to induce ROS, which was only observed in the presence of light. Its lack of significant effect in the dark suggests that MA’s mechanism of action may be less dependent on oxidative stress and more reliant on other intracellular pathways, such as disruption of parasite metabolism or inhibition of thiol-containing molecules.
Notably, the strong pro-oxidative response elicited by HC and NHC, especially when combined with light, aligns with the observed induction of apoptosis and supports the notion that ROS plays a pivotal role in the downstream activation of cell death pathways in amastigotes. However, while increased ROS contributes to anti-parasitic efficacy, it may also pose risks of collateral damage to host cells, emphasizing the need for careful dose optimization and selective targeting.
In conclusion, the data suggest that HC and NHC, particularly under light exposure, are potent inducers of ROS, contributing to their leishmanicidal action via oxidative stress-mediated apoptosis. These insights highlight the therapeutic promise of combining nanocarrier-based drug delivery with light-responsive strategies to enhance efficacy against intracellular pathogens. Future investigations should focus on the mechanistic basis of ROS generation and explore the modulation of antioxidants as a strategy to balance efficacy and safety in host-parasite interactions. Despite the promising in vitro findings, this study has certain limitations that must be acknowledged. One notable concern is the potential immunogenicity and toxicity associated with the FN. While the formulation exhibited minimal cytotoxicity on macrophages under our experimental conditions, cadmium-containing materials are known to pose systemic toxicity risks, particularly upon prolonged exposure or accumulation in vital organs. Additionally, the immunological response to metal-organic frameworks such as MIL-125(Ti) remains incompletely understood and may vary depending on particle size, surface chemistry, and administration route. Therefore, thorough in vivo studies are essential to assess the biodistribution, clearance, long-term safety, and potential immunogenic effects of this nanoplatform. These investigations will be critical in determining the translational viability of CdS/MIL-125(Ti)-based drug delivery systems in clinical settings.
Conclusion
This study demonstrates that HC and its NHC significantly enhance ROS production in L. tropica-infected macrophages, with a marked amplification under light exposure. The light-dependent synergistic effect observed with both HC and NHC underscores their potential as effective photodynamic agents in promoting oxidative stress-mediated clearance of parasites. In contrast, the conventional drug (MA) exhibited limited ROS induction, suggesting a distinct mode of action. These findings highlight the therapeutic promise of combining light-based strategies with targeted drug delivery systems to optimize anti-leishmanial efficacy through controlled ROS generation. Further, in vivo studies are warranted to validate these results and explore the clinical applicability of light-activated treatments.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author.
Abbreviations
- HC:
-
Hydroxychloroquine
- MA:
-
Meglumine antimoniate
- NHC:
-
Hydroxychloroquine-cds/MIL-125(Ti)-loaded niosomes
- FN:
-
Cds/MIL-125(Ti)
- PDT:
-
Photodynamic therapy
- Mofs:
-
Metal-organic frameworks
- DLS:
-
Light scattering
- TEM:
-
Transmission electron microscopy
- PDI:
-
Polydispersity index
- PDB:
-
Protein data bank
- MVD:
-
Molecular virtual docking
- PBS:
-
Phosphate-buffered saline
- MLC:
-
Differentiation into macrophage-like cells
- OD:
-
Optical density
- DMSO:
-
Dimethyl sulfoxide
- SI:
-
Selectivity index
- PI:
-
Propidium iodide
- EE%:
-
Entrapment efficiency
- UC:
-
Untreated control group
- CI:
-
Combination index
References
Karimi, M., Dalimi, A., Jamei, F., Ghaffarifar, F. & Dalimi, A. The killing effect of silver nanoparticles and direct electric current induction on Leishmania major promastigotes In vitro. Modares J. Med. Sciences: Pathobiology. 18, 87–96 (2015).
Handler, M. Z., Patel, P. A., Kapila, R., Al-Qubati, Y. & Schwartz, R. A. Cutaneous and mucocutaneous leishmaniasis: Clinical perspectives. Journal of the American Academy of Dermatology. 73, Preprint at https://doi.org/10.1016/j.jaad.2014.08.051 (2015).
De Almeida, L. et al. Nanotechnological strategies for treatment of leishmaniasis-a review. Journal of Biomedical Nanotechnology. 13, 117–133. Preprint at https://doi.org/10.1166/jbn.2017.2349 (2017).
Mesquita, J. T., da Costa-Silva, T. A., Borborema, S. E. T. & Tempone, A. G. Activity of imidazole compounds on Leishmania (L.) infantum chagasi: reactive oxygen species induced by econazole. Mol. Cell. Biochem. 389, 293–300 (2014).
Rajabi, O., Sazgarnia, A., Abbasi, F. & Layegh, P. The activity of ozonated Olive oil against leishmania major promastigotes. Iran. J. Basic. Med. Sci. 18, 915 (2015).
Singh, N., Kumar, M., Singh, R. K. & Leishmaniasis Current status of available drugs and new potential drug targets. Asian Pac. J. Trop. Med. 5, 485–497 (2012).
Lopera, A. A., Montoya, A., Vélez, I. D., Robledo, S. M. & Garcia, C. P. Synthesis of calcium phosphate nanostructures by combustion in solution as a potential encapsulant system of drugs with photodynamic properties for the treatment of cutaneous leishmaniasis. Photodiagnosis Photodyn Ther. 21, 138–146 (2018).
Ribeiro, J. B. P. et al. Evaluation of the efficacy of systemic miltefosine associated with photodynamic therapy with liposomal Chloroaluminium phthalocyanine in the treatment of cutaneous leishmaniasis caused by Leishmania (L.) amazonensis in C57BL/6 mice. Photodiagnosis Photodyn Ther. 13, 282–290 (2016).
Akbari, M., Oryan, A. & Hatam, G. Application of nanotechnology in treatment of leishmaniasis: A Review. Acta Tropica. 172, 86–90. Preprint at https://doi.org/10.1016/j.actatropica.2017.04.029 (2017).
Pellosi, D. S., De Jesus, P. & Tedesco, A. C. da C. C. Spotlight on the delivery of photosensitizers: different approaches for photodynamic-based therapies. Expert Opinion on Drug Delivery. 14, 1395–1406. Preprint at https://doi.org/10.1080/17425247.2017.1307337 (2017).
Gedda, M. R. et al. Nanodiagnostics in leishmaniasis: A new frontiers for early elimination. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology. 13, e1675 Preprint at https://doi.org/10.1002/wnan.1675 (2021).
Nazir, A. M. et al. Evaluating the use of hydroxychloroquine in treating patients with rheumatoid arthritis. Cureus https://doi.org/10.7759/cureus.19308 (2021).
Bansal, P. et al. Hydroxychloroquine: a comprehensive review and its controversial role in coronavirus disease 2019. Annals of Medicine. 53, 117–134. Preprint at https://doi.org/10.1080/07853890.2020.1839959 (2021).
Yusuf, I. H., Issa, C. & Ahn, S. J. P. Hydroxychloroquine-induced Retinal Toxicity. Frontiers in Pharmacology. 14, 1196783. Preprint at https://doi.org/10.3389/fphar.2023.1196783 (2023).
Bartelds, R. et al. Niosomes, an alternative for liposomal delivery. PLoS One. 13, e0194179 (2018).
Kerr, D. J., Rogerson, A., Morrison, G. J., Florence, A. T. & Kaye, S. B. Antitumour activity and pharmacokinetics of niosome encapsulated adriamycin in monolayer, spheroid and xenograft. Br. J. Cancer. 58, 432–436 (1988).
Moammeri, A. et al. Current advances in niosomes applications for drug delivery and cancer treatment. Materials Today Bio. 23, 100837. Preprint at https://doi.org/10.1016/j.mtbio.2023.100837 (2023).
Zhang, J. et al. Electrogenerated chemiluminescence DNA biosensor based on hairpin DNA probe labeled with ruthenium complex. Anal. Chem. 80, 2888–2894 (2008).
Torad, N. L. et al. MOF-derived nanoporous carbon as intracellular drug delivery carriers. Chem. Lett. 43, 717–719 (2014).
Junyaprasert, V. B., Singhsa, P., Suksiriworapong, J. & Chantasart, D. Physicochemical properties and skin permeation of span 60/Tween 60 niosomes of ellagic acid. Int. J. Pharm. 423, 303–311 (2012).
Manosroi, A. et al. Characterization of vesicles prepared with various non-ionic surfactants mixed with cholesterol. Colloids Surf. B Biointerfaces. 30, 129–138 (2003).
Varshosaz, J., Pardakhty, A., Hajhashemi, V. I. & Najafabadi, A. R. Development and physical characterization of Sorbitan monoester niosomes for insulin oral delivery. Drug Delivery: J. Delivery Target. Therapeutic Agents. 10, 251–262 (2003).
Nasr, M., Mansour, S., Mortada, N. D. & Elshamy, A. A. Vesicular aceclofenac systems: A comparative study between liposomes and niosomes. J. Microencapsul. 25, 499–512 (2008).
Priprem, A., Janpim, K., Nualkaew, S. & Mahakunakorn, P. Topical niosome gel of Zingiber cassumunar Roxb. Extract for anti-inflammatory activity enhanced skin permeation and stability of compound D. AAPS PharmSciTech. 17, 631–639 (2016).
Tavano, L., Aiello, R., Ioele, G., Picci, N. & Muzzalupo, R. Niosomes from glucuronic acid-based surfactant as new carriers for cancer therapy: preparation, characterization and biological properties. Colloids Surf. B Biointerfaces. 118, 7–13 (2014).
Bayindir, Z. S. & Yuksel, N. Characterization of niosomes prepared with various nonionic surfactants for Paclitaxel oral delivery. J. Pharm. Sci. 99, 2049–2060 (2010).
Mehta, S. K. & Jindal, N. Formulation of tyloxapol niosomes for encapsulation, stabilization and dissolution of anti-tubercular drugs. Colloids Surf. B Biointerfaces. 101, 434–441 (2013).
Akhilesh, D., Bini, K. B. & Kamath, J. V. Review on span-60 based non-ionic surfactant vesicles (niosomes) as novel drug delivery. Int. J. Res. Pharm. Biomedical Sci. 3, 6–12 (2012).
Hao, Y., Zhao, F., Li, N. & Yang, Y. Studies on a high encapsulation of Colchicine by a niosome system. Int. J. Pharm. 244, 73–80 (2002).
Bitencourt-Ferreira, G. & de Azevedo, W. F. Molegro virtual docker for docking. In Methods in Molecular Biology. (2019). (2053).
Allison, R. R. et al. Photosensitizers in clinical PDT. Photodiagnosis Photodyn Ther. 1, 27–42 (2004).
Fröhlich, E. The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticles. Int. J. Nanomed. 7, 5577 (2012).
Mok, Z. H. The effect of particle size on drug bioavailability in various parts of the body. Pharmaceutical Science Advances. 2, 100031. Preprint at https://doi.org/10.1016/j.pscia.2023.100031 (2024).
Inkson, B. J. Scanning Electron Microscopy (SEM) and Transmission Electron Microscopy (TEM) for Materials Characterization. in Materials Characterization Using Nondestructive Evaluation (NDE) Methods (2016). https://doi.org/10.1016/B978-0-08-100040-3.00002-X
Honary, S. & Zahir, F. Effect of zeta potential on the properties of nano-drug delivery systems - A review (Part 1). Trop. J. Pharm. Res. 12, 255–264 (2013).
Jia, L. et al. Optimization of nanoparticles for smart drug delivery: A review. Nanomaterials. 11, 2790. Preprint at https://doi.org/10.3390/nano11112790 (2021).
Parizi, M. H. et al. Antileishmanial activity of Niosomal combination forms of Tioxolone along with benzoxonium chloride against Leishmania tropica. Korean J. Parasitol. 57, 359 (2019).
Seyedi, F. et al. Comparison of cytotoxicity of miltefosine and its Niosomal form on chick embryo model. Sci. Rep. 14, 2482 (2024).
Khan, H., Nazir, S., Farooq, R. K., Khan, I. N. & Javed, A. Fabrication and assessment of Diosgenin encapsulated stearic acid solid lipid nanoparticles for its anticancer and antidepressant effects using in vitro and in vivo models. Front. Neurosci. 15, 806713 (2022).
Kako, D., Ghareeb, M. M. & Al-Lami, M. S. High-Performance liquid chromatography (HPLC) method validation for identifying and quantifying rebamipide in ethosomes. Cureus https://doi.org/10.7759/cureus.56061 (2024).
Elahe et al. The synergistic anti-leishmanial effect of photodynamic therapy employing chemotherapy-mediated nanocomposites. Sci. Rep. 15, 16282 (2025).
Khosravi, A. et al. Cytotoxicity of Amphotericin B and AmBisome: In Silico and In Vivo Evaluation Employing the Chick Embryo Model. Front Pharmacol 13, 860598 (2022).
Sarfraz, M. et al. 2,3-Dihydroquinazolin-4(1H)-one as a new class of Anti-Leishmanial agents: A combined experimental and computational study. Crystals (Basel) 12, (2022).
Stevanovic, S. et al. Synthesis, in silico, and in vitro evaluation of anti-leishmanial activity of oxadiazoles and indolizine containing compounds flagged against anti-targets. Molecules 24, 1282 (2019).
Malathi, S. et al. Epidermal growth factor receptor targeted doxorubicin and vitexin loaded niosomes for enhanced breast cancer therapy. Mater. Adv. 4, 5224–5237 (2023).
Rasul, A. et al. In vitro characterization and release studies of combined nonionic surfactant-based vesicles for the prolonged delivery of an immunosuppressant model drug. Int J Nanomedicine 15, (2020).
Karimipour-Saryazdi, A., Jafari, M. M., Omidi, R., Ghaffarifar, F. & Sadeghi, S. H. Anti-leishmania effect of magnesium oxide nanoparticles on Leishmania tropica/infantum and Leishmania -Infected macrophages. Int. J. Enteric Pathog. 10, 144–154 (2022).
Mostafavi, M. et al. Niosomal formulation of amphotericin B alone and in combination with glucantime: In vitro and in vivo leishmanicidal effects. Biomed. Pharmacotherapy. 116, 108942 (2019).
Ilaghi, M. et al. The potential role and apoptotic profile of three medicinal plant extracts on Leishmania tropica by MTT assay, macrophage model and flow cytometry analysis. Parasite Epidemiol. Control. 12, e00201 (2021).
Salarkia, E. et al. In silico and in vitro potentials of crocin and amphotericin B on Leishmania major: Multiple synergistic mechanisms of actions. PLoS One 18, e0291322 (2023).
Keyhani, A. et al. In vitro and in vivo therapeutic potentials of 6-gingerol in combination with amphotericin B for treatment of leishmania major infection: powerful synergistic and multifunctional effects. Int. Immunopharmacol. 101, 108274 (2021).
Varzandeh, M. et al. Photodynamic therapy for leishmaniasis: Recent advances and future trends. Photodiagnosis and Photodynamic Therapy. 36, 102609. Preprint at https://doi.org/10.1016/j.pdpdt.2021.102609 (2021).
Marcolino, L. M. C. et al. Photodynamic therapy of cationic and anionic BSA-curcumin nanoparticles on amastigotes of Leishmania Braziliensis and Leishmania major and Leishmania amazonensis. Photodiagnosis Photodyn Ther. 46, 104001 (2024).
Espitia-Almeida, F., Díaz-Uribe, C., Vallejo, W. & Gómez-Camargo, D. & Romero Bohórquez, A. R. In vitro anti-leishmanial effect of metallic meso-substituted porphyrin derivatives against leishmania braziliensis and leishmania panamensis promastigotes properties. Molecules 25, 1887 (2020).
Campos, T. M., Costa, R., Passos, S. & Carvalho, L. P. Cytotoxic activity in cutaneous leishmaniasis. Mem. Inst. Oswaldo Cruz. 112, 733–740 Preprint at. https://doi.org/10.1590/0074-02760170109 (2017).
Duarte, D. & Vale, N. Evaluation of synergism in drug combinations and reference models for future orientations in oncology. Current Research in Pharmacology and Drug Discovery. 3, 100110. Preprint at https://doi.org/10.1016/j.crphar.2022.100110 (2022).
Mahmoudvand, H., Shakibaie, M., Tavakoli, R., Jahanbakhsh, S. & Sharifi, I. Vitro study of leishmanicidal activity of biogenic selenium nanoparticles against Iranian isolate of sensitive and glucantime- resistant Leishmania tropica. Iran. J. Parasitol. 9, 452 (2014).
Negara, K. S. et al. The role of Caspase-3, Apoptosis-Inducing Factor, and B-cell Lymphoma-2 expressions in term premature rupture of membrane. Revista Brasileira De Ginecol. E Obstet. 40, 733–739 (2018).
Khosravi, A. et al. Vascular apoptosis associated with Meglumine antimoniate: In vivo investigation of a chick embryo model. Biochem. Biophys. Res. Commun. 505, 794–800 (2018).
Gundala, S. R. et al. Hydroxychavicol, a betel leaf component, inhibits prostate cancer through ROS-driven DNA damage and apoptosis. Toxicol. Appl. Pharmacol. 280, 86–96 (2014).
Aureliano, D. P. et al. Treatment and Control of Leishmaniasis Using Photodynamic Therapy. In Leishmaniasis - Trends in Epidemiology, Diagnosis and Treatment. 1, (2014).
Sazgarnia, A., Bahreyni-Toosi, M. H., Layegh, P., Rajabi, O. & Ghodsinia, R. M. Liposomal zinc phthalocyanine as a potential agent for photodynamic therapy of leishmaniasis. Indian Journal of Dermatology, Venereology and Leprology. 76, 417. Preprint at https://doi.org/10.4103/0378-6323.66591 (2010).
Redza-Dutordoir, M. & Averill-Bates, D. A. Activation of apoptosis signalling pathways by reactive oxygen species. Biochimica et Biophysica Acta - Molecular Cell Research. 1863, 2977–2992. Preprint at https://doi.org/10.1016/j.bbamcr.2016.09.012 (2016).
Acknowledgements
We would like to thank all the personnel of the Leishmaniasis Research Center for their help in conducting this study.
Funding
This project was supported by the Kerman University of Medical Sciences, Kerman, Iran (Grant no. 402000402).
Author information
Authors and Affiliations
Contributions
EM, ES, MRA and AK (methodologist and collected the data), EM and ES (analysis data and validation), IS and EM (original draft preparation, supervision), IS, EM, ES, AKh, MHP and MB (review and editing). All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical standards
The Ethics Committee of Kerman University of Medical Sciences, Kerman, Iran, approved the present study (Approval ID. IR.KMU.REC. 1402.497).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Molaakbari, E., Sharifi, I., Khosravi, A. et al. Synthesis, characterization, and comparative evaluation of hydroxychloroquine and its niosomal nanoformulation: anti-leishmanial, cytotoxicity, and immunomodulatory effects in photodynamic therapy. Sci Rep 15, 41540 (2025). https://doi.org/10.1038/s41598-025-25493-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-25493-4