Abstract
Delirium is an acute change in cognition, common in hospitalized older adults, and associated with high healthcare and human cost; however, delirium’s genetic and proteomic background remains poorly understood. Here we conducted a genetic meta-analysis on delirium using multi-ancestry data from the UK Biobank, FinnGen, All of Us Research Program and Michigan Genomics Initiative cohorts (n = 1,059,130; 11,931 cases), yielding the Apolipoprotein E (APOE) gene as a strong delirium risk factor independently of dementia. A multi-trait analysis of delirium with Alzheimer disease identified five delirium genetic risk loci. Plasma proteins associated with up to 16-year incident delirium in UK Biobank (n = 32,652; 541 cases) revealed protein biomarkers implicating brain vulnerability, inflammation and immune response processes. Incorporating proteomic and genetic evidence via Mendelian randomization, colocalization and druggability analyses, we indicate potentially useful drug target proteins for delirium. Combining proteins, APOE-ε4 status and demographics significantly improved incident delirium prediction compared to demographics alone. Our results provide insight into delirium’s etiology and may guide further research on clinically relevant biomarkers.
Similar content being viewed by others
Main
Delirium is a complex neurocognitive condition affecting nearly 25% of hospitalized older adults1. It has a rapid onset, usually lasting from hours to days, and is characterized by an acute and often reversible disturbance of attention, cognitive ability and awareness2. It is triggered mainly by acute illness, surgery or injury. Delirium is strongly associated with multiple adverse outcomes, including increased mortality, prolonged hospitalization3 and increased healthcare costs, with one study estimating an annual cost of US$182 billion per year to European healthcare systems4.
Delirium has a complex bidirectional relationship with dementia, in that people with dementia are more likely to experience delirium in the context of an acute trigger, and delirium episodes are strongly associated with future dementia risk3,5. There is some overlap in the clinical features of these conditions, notably with respect to cognitive dysfunction, perceptual disturbances and sleep–wake cycle changes6; however, the course of delirium is markedly different with respect to onset and duration. The pathophysiology of delirium is complex and likely involves multiple potential mechanisms3. Animal model and human biomarker studies implicate systemic inflammation triggering neuroinflammation, disruption of the blood–brain barrier and neuronal injury in delirium3,7,8,9. Aspects of these mechanisms are also present in dementia, leading to the proposal that there may be shared and potentially bidirectional pathology between delirium and dementia, such as neuroinflammation leading to neurodegeneration9,10.
Despite its high healthcare burden, current understanding of genetic and biological mechanisms underlying delirium’s pathophysiology is still limited, hindering personalized medicine efforts to predict, prevent and treat the condition. Given delirium’s increasing presence in the global aging population6, alleviating its human and economic cost11 through personalized medicine is all the more important.
Previous studies on the genetic determinants of delirium have been small in scale and inconclusive3,6,12, largely focusing on a single or small sets of candidate genes13,14,15,16,17,18,19,20,21,22. The Apolipoprotein E (APOE) gene, specifically its ε4 haplotype, is the most intensively studied gene15,17,19,20,21, though clear conclusions on its relationship with delirium remain lacking6,23. Advances in genome-wide association studies (GWAS) over recent decades24 have allowed researchers to search the full spectrum of the human genome for genetic risk factors involved in neurocognitive disorders25,26,27, offering invaluable new insights into disease mechanisms; however, research on delirium using these methods has lagged behind other neurocognitive disorders, with only a few, relatively underpowered delirium GWAS conducted to date28,29,30. Moreover, those studies did not address comprehensively the biological implications of potential gene–disease associations and were conducted primarily on individuals of European descent.
Research on protein biomarkers for delirium has received increased attention recently, identifying potential blood plasma, serum and cerebrospinal fluid (CSF) candidates6,31. Those biomarkers include inflammatory proteins, such as interleukin (IL)-6 and C-reactive protein (CRP)6,31,32, Alzheimer disease (AD) pathology markers6 and markers of neuronal injury, such as the neurofilament light chain (NEFL)9 and glial fibrillary acidic protein (GFAP)8. Previous studies, however, are limited in terms of sample size and, often, the range of proteins tested.
In the current study we aim to upscale the efforts in identifying genetic and proteomic determinants of delirium risk. To achieve this, we (1) conducted a large-scale meta-analysis of delirium GWAS datasets, including individuals from diverse ancestries; (2) tested for plasma proteome signatures of incident delirium for up to 16 years of follow-up in the UK Biobank (UKB)33 and triangulated the results using genetically supported evidence from Mendelian randomization, colocalization and druggability analyses; and (3) conducted a multi-trait meta-analysis between delirium and AD, leveraging the shared genetic basis of the two conditions6 and boosting the power to detect genetic associations for delirium34.
Results
APOE gene as delirium genetic risk factor
To identify genetic variants associated with delirium, a multi-ancestry genome-wide association meta-analysis (GWAMA) was conducted on eight subcohorts (Supplementary Table 1) from four global ancestries: European (EUR, \({n}_{\mathrm{cases}}=7,988\); \({n}_{\mathrm{controls}}=549,568\), 52.6% of total sample size), Finnish (FIN, \({n}_{\mathrm{cases}}=3,371\); \({n}_{\mathrm{controls}}=\mathrm{388,560}\), 37%), African (AFR, \({n}_{\mathrm{cases}}\) = 348; \({n}_{\mathrm{controls}}=\mathrm{59,780}\), 5.7%), south Asian (SAS, \({n}_{\mathrm{cases}}=107\); \({n}_{\mathrm{controls}}\) = 9,356, 0.9%) and admixed American/Hispanic (AMR, \({n}_{\mathrm{cases}}=117\); \({n}_{\mathrm{controls}}=39,977\), 3.8%). Age distributions for the UKB and All of Us Research Program (AoU) cohorts are presented in Extended Data Fig. 1. In total, the GWAMA consisted of up to 1,059,130 individuals and 11,931 delirium cases, yielding results for 24,951,028 single-nucleotide polymorphism (SNP) genetic variants. The overall SNP heritability (\({h}_{\mathrm{SNP}}^{2}\)) of delirium was estimated on the observed scale as \({h}_{\mathrm{SNP}}^{2}=0.0055\,({\rm{s}}.{\rm{e}}.\,9\,\times \,{10}^{-4}{;}\,P=2.5\,\times \,{10}^{-9})\), significantly different from zero, and as \({h}_{\mathrm{SNP},l}^{2}=0.029\) on the liability scale.
Variants at the APOE gene and within its close genomic region on chromosome 19 (Fig. 1) were significantly associated with delirium. The lead variant rs429358 (T > C, odds ratio (OR) 1.60, 95% CI 1.55–1.65; P = 9.7 × 10−177) is an APOE missense variant, which together with the rs7412 C > T variant forms the APOE-ε4 haplotype (the rs429358 C and rs7412 C alleles), an established risk factor for AD35. rs7412 was also significantly associated with delirium in our GWAMA (C > T, OR 0.84, 95% CI 0.79–0.88; P = 1.8 × 10−11).
Each point represents a genetic variant. The x axis denotes the variant’s genomic position and the y axis the two-sided P value of the inverse-variance based meta-analysis association z-score. No multiple testing P value adjustments were applied. The gray dashed line denotes the genome-wide significance P value threshold 5 × 10−8. The gene in which the lead significant variant is located is annotated. The plot was created using the GWASLab Python package.
The lead variant rs429358 showed population-specific genetic effects for delirium in the contributing subcohorts (Fig. 2). Significant associations were observed in all, except European (Michigan Genomics Initiative (MGI), P = 0.27) and admixed American (AoU AMR, P = 0.12) populations from the USA, with USA-based populations generally showing smaller effect sizes.
Forest plot showing the cohort-specific association results for the rs429358 T > C lead variant with delirium. Effect sizes (log OR ± 95% CI) for the C allele and corresponding two-sided P values are shown for each contributing subcohort and the overall meta-analysis. Meta-analysis two-sided P value is derived based on the inverse-variance based meta-analysis association z-score. No multiple testing P value adjustments were applied. Gray dash-dotted lines separate results for each ancestry group. EUR, European; FIN, Finnish; AFR, African; SAS, south Asian.
Conditional GWAS analysis on the APOE-ε4 haplotype resulted in all variants on the APOE region losing significance (Extended Data Fig. 2), suggesting that APOE-ε4 is the sole independent genetic risk factor in the region. On the same analysis, an intronic variant within the ADAM32 gene on chromosome 8 gained significance (rs531178459; P = 3.3 × 10−8).
Furthermore, using a series of sensitivity analyses in UKB (Methods and Supplementary Table 2), we tested to what extent the observed APOE association with delirium is driven by underlying dementia. Variants in the APOE region remained significant after adjusting for dementia status in the delirium GWAS (Extended Data Fig. 3). Specifically, the lead variant from the unadjusted GWAMA, rs429358, showed again a strong association (OR 1.20, 95% CI 1.12–1.28; P = 3.7 × 10−15). Variants on the SEC14L1 gene on chromosome 17 were also significant in the dementia-adjusted analysis. rs429358 remained significant in GWAS conducted on dementia-free (OR 1.27, 95% CI 1.2–1.34; P = 4.7 × 10−18; Extended Data Fig. 4) and AD-free (OR 1.45, 95% CI 1.38–1.52; P = 3.9 × 10−56; Extended Data Fig. 5) stratified cohorts. rs429358 genetic signals in dementia-adjusted and dementia/AD-free GWAS were replicated in AoU (Supplementary Table 2). The APOE genetic signal remained highly significant in an age-stratified GWAS, on participants with age 60 years or more (OR 1.7, 95% CI 1.63–1.77; P = 2.7 × 10−141; Extended Data Fig. 6 and Supplementary Table 2).
Multi-trait analysis between delirium and Alzheimer disease
We found a significant genetic correlation (\({r}_{g}\)) between delirium and AD, \({r}_{g}=0.38\,({\rm{s}}.{\rm{e}}.\,0.12{;}\,P=1.9\,\times \,{10}^{-3})\), pointing out to a partially shared genetic architecture. Given this, we further conducted a multi-trait analysis of GWAS summary statistics (MTAG) between delirium and AD. MTAG can increase statistical power to detect new genetic associations, by leveraging the shared genetic information between related traits34. Our MTAG analysis identified ten independent genetic loci associated with delirium, of which five replicated in the held-out set (Fig. 3 and Supplementary Table 3). The closest genes mapped to the lead replicated variants included: CR1 (rs4844610 A > C; OR 1.01, 95% CI 1.006–1.014; P = 1.4 × 10−8), BIN1 (rs6733839 T > C; OR 1.015, 95% CI 1.012–1.018; P = 7 × 10−25), CLU (rs2279590 T > C; OR 0.992, 95% CI 0.989–0.995; P = 4.2 × 10−8), MS4A4A (rs1582763 A > G; OR 0.991, 95% CI 0.988–0.994) and TOMM40 (rs117310449 T > C; OR 1.09, 95% CI 1.07–1.1; P = 7 × 10−38).
Delirium-specific MTAG summary statistics are shown. Each point represents a genetic variant. The x axis denotes the variant’s genomic position and the y axis the two-sided P value of the MTAG-adjusted unstandardized effect size estimate in the discovery set. No multiple testing P value adjustments were applied. The gray dashed line denotes the genome-wide significance P value threshold 5 × 10−8. The closest gene in which the lead significant variant is located is annotated. Red highlights the loci ± 1,000 kb around lead variants that replicated. The plot was created using the GWASLab Python package.
Four out of five of the lead replicated MTAG signals were also significant in the original delirium GWAMA (Supplementary Table 3), with rs2279590 (CLU gene) being marginally nonsignificant (P = 0.058). Effect sizes were consistent between MTAG and delirium GWAMA results. Variants in the APOE genomic region that were significant in our delirium GWAMA were also significant in MTAG.
Mediation analysis
We implemented a mediation analysis to estimate how much of the APOE-ε4 genetic effect on delirium is mediated by dementia, adjusted for age and sex (Fig. 4). We found that APOE-ε4 exerts a significant direct effect on delirium in a dose-dependent way: OR direct effect (0vs1) 1.14, 95% CI 1.08–1.2; P = 4.5 × 10−7; for one APOE-ε4 copy, and OR direct effect (0vs2) 1.29, 95% CI 1.15–1.45; P = 1.7 × 10−5 for two APOE-ε4 copies. The APOE-ε4 total effect on delirium was partially mediated by dementia (OR indirect effect (0vs1) 1.39, 95% CI 1.36–1.42; P = 1.1 × 10−237; and OR indirect effect (0vs2) 2.59, 95% CI 2.47–2.77; P = 2.1 × 10−233), with the direct effect accounting for 29% and 21% of the total effect for one and two APOE-ε4 copies, respectively. These results further support the role of APOE gene on delirium, independently of dementia.
a, Hypothesized directed acyclic graph, showing all-cause dementia as mediator of APOE-ε4 genetic effect on delirium (black arrows), adjusted for baseline covariates: age and sex (gray arrows). b,c, Effect decomposition of the total APOE-ε4 effect, into natural direct (independent of dementia) and natural indirect (mediated through dementia) effects ± 95% CI (n = 407,827 individuals in UKB). The effect of having one APOE-ε4 haplotype (b) and the effect of having two APOE-ε4 haplotypes (c), compared to having none. NDE, natural direct effect; NIE, natural indirect effect.
Our sensitivity analysis regarding the role of unmeasured confounding suggests that, an unmeasured confounder associated with both dementia and delirium with approximate effect sizes of 1.54 each, over and above the measured covariates, could suffice to completely explain away the observed direct effect of one APOE-ε4 copy on delirium, but weaker confounding could not36. Respectively, the minimum unmeasured confounder effect size would need to be 1.9 to completely explain away the direct effect of two APOE-ε4 copies.
Finally, a mediation analysis further adjusting for cognitive function, socioeconomic deprivation and chronic disease burden, on top of age and sex, still detected a significant direct effect of APOE-ε4 on delirium: OR direct effect (0vs1) 1.12, 95% CI 1.01–1.25; P = 0.038 (32% of the total effect) for one APOE-ε4 copy and OR direct effect (0vs2) 1.55, 95% CI 1.18–2.06; P = 2 × 10−3 (34% of the total effect) for two APOE-ε4 copies, respectively (Extended Data Fig. 7).
Protein risk factors for incident delirium
A proteome-wide association study (PWAS) on 32,652 European UKB participants (541 cases) revealed 109 out of the 2,919 total proteins, whose plasma levels were significantly associated with incident delirium up to 16 years of follow-up (Fig. 5a and Supplementary Table 4) at a Bonferroni-adjusted P value threshold (P = 1.7 × 10−5). The APOE protein had a negative effect on incident delirium risk, meaning that higher plasma levels of the protein are associated with reduced future risk. The association was significant at the nominal level (0.05), but not after multiple test correction (OR 0.86, 95% CI 0.79–0.94; P = 7 × 10−4; Supplementary Table 4).
a,b, Volcano plot showing the proteome-wide associations of 2,919 plasma proteins with incident delirium in the nonstratified (a) and the dementia-free (b) UKB proteomic set. ORs of the logistic regression models are plotted on the x axis and respective two-sided −log10(P) of the corresponding logistic regression z-scores are plotted on the y axis. All models are adjusted for age at protein collection, sex and BMI. The black dashed horizontal line indicates the Bonferroni-adjusted P value threshold of 1.7 × 10−5, with proteins above this line colored red (a) and blue (b), respectively. The gray dashed horizontal line indicates the nominal P value threshold of 0.05. The plot was created using the EnhancedVolcano R package (v.1.18.0).
Further adjusting the individual protein models for APOE-ε4 status did not substantially alter the results (Supplementary Table 5), having highly correlated effect size estimates with the models adjusted only for age, sex and body mass index (BMI) (Pearson’s correlation r = 0.99). Additionally including a protein × APOE-ε4 interaction term also yielded highly similar results (main effect correlation r = 0.93). No significant protein × APOE-ε4 interaction has observed at a Bonferroni-adjusted threshold of P value < 1.7 × 10−5 (Supplementary Table 6); however, the CEND1 protein exhibited an interaction with APOE-ε4 marginally below threshold (β(interaction) 0.27, 95% CI 0.10–0.42; P(interaction) = 8 × 10−4).
The 109 proteome-wide significant proteins were found to be significantly enriched (q-value < 0.05) in several important inflammation and immune response biological pathways, such as IL and tumor necrosis factor signaling (Supplementary Table 7).
Restricting our PWAS on the dementia-free subset of UKB (31,692 participants; 349 delirium cases) reduced the number of proteins significantly associated with incident delirium to 75 (Fig. 5b and Supplementary Table 8). Notably, the APOE plasma protein, although still had a negative effect size, lost nominal significance and had reduced magnitude that in the nonstratified PWAS (OR 0.97, 95% CI 0.87–1.08; P = 0.63).
Protein selection and prediction models
A machine-learning framework was applied to further pin down which plasma proteins are robustly associated with incident delirium. Our approach, based on the Least Absolute Shrinkage and Selection Operator (LASSO) regularized regression37 and stability selection38, revealed 19 proteins (stability-selected proteins; Supplementary Table 9) consistently selected as predictive of incident delirium in the training set. All the stability-selected proteins represent a subset of the top individually significant proteins identified through the proteome-wide association analysis. The FGL1 protein was removed from subsequent analyses, as it had a nonsignificant contribution to the re-fit prediction models and was dropped during stepwise regression. The 18 remaining stability-selected proteins provide marginal prediction improvements of incident delirium on an independent test set, compared to predictions based on demographic factors alone (Fig. 6 and Supplementary Tables 10 and 11). Specifically, adding the 18 stability-selected proteins to the ‘basic’ model that includes age, sex and BMI as predictors increased the area under the curve (AUC) from 0.764 to 0.791, but the increase was not significant (DeLong test P value = 0.09; Supplementary Table 11); however, adding proteins and APOE-ε4 status to the basic model showed a significant prediction improvement (AUC from 0.764 to 0.794, P = 0.049; Supplementary Table 11). Finally, the model fit with only the selected proteins performed worse than the basic model (AUC from 0.764 to 0.729; P = 0.21; Fig. 6a and Supplementary Table 11). The precision–recall (PR) performance showed a similar pattern (Fig. 6b), with the full models having higher PR-AUC of 0.065 and 0.06 for the ‘APOE + proteomic + basic’ and the ‘proteomic + basic’ models, respectively, compared to 0.043 for the basic model.
a,b, ROC (a) and PR curves (b) showing performance metrics of different models for predicting incident delirium on the held-out test set (ncases = 105; ncontrols = 6,378). The ‘proteomic’ logistic regression model is fit with the 18 stability-selected proteins, the ‘basic’ model is fit using only age at protein collection, sex and BMI and the ‘proteomic + basic’ includes both. The ‘APOE + proteomic + basic’ model additionally includes APOE-ε4 haplotype count as predictor. The dotted black lines indicate the performance of a randomly classifying model (the diagonal of the ROC curve (a) and the disease prevalence horizontal line in the PR curve (b)). ROC and PR plots and AUC calculations were made using the yardstick R package (v.1.3.0).
We repeated our protein selection and prediction framework in the dementia-free subcohort of the UKB proteomic set. Overall, 14 out of the 19 stability-selected proteins still had a significant effect on incident delirium in the training set (Supplementary Table 9); however, only the AREG and MSLN proteins were consistently selected in the dementia-free subcohort (selection frequency >0.5). We still observed a marginally better prediction of incident delirium on the test set using APOE-ε4 and the 14 stability-selected proteins on top of demographic factors (AUC from 0.758 to 0.79, P = 0.13; PR-AUC from 0.033 to 0.036) (Extended Data Fig. 8 and Supplementary Table 10), although now with a nonsignificant AUC improvement.
Mendelian randomization
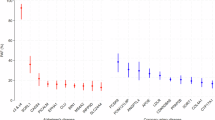
We performed Mendelian randomization (MR), to test for causal associations between 1,989 plasma proteins (exposures) and delirium (outcome). We found 53 proteins causally associated with delirium at a false discovery rate (FDR) q threshold <0.05 using inverse-variance weighted (IVW) or Wald ratio MR (Fig. 7 and Supplementary Table 12). Out of the 53 MR significant proteins, DSC2 was the only one with a significant association in our PWAS analysis of protein risk factors (Fig. 5) and a consistent direction of effect. Using a less strict FDR q < 0.05 threshold in our PWAS, seven additional proteins were identified (ADAM8, APOE, DPP10, LAYN, NT5C1A, PILRA and PVR) that were significant in both the PWAS and MR. At a nominal PWAS P value level (P < 0.05), three more proteins (CCL25, PON3 and GGH) overlapped the significant MR results. Four of the above PWAS-MR overlapping significant proteins successfully replicated in our FinnGen replication MR: GGH, PVR, APOE and PILRA (Fig. 7). All the replicated delirium-associated proteins were also significant using sensitivity MR methods (weighted median (WM), maximum likelihood and MR-Egger; P < 0.05) (Supplementary Table 13). The MR-Egger intercept test did not reveal evidence of horizontal pleiotropy (P > 0.05). Genetic variant heterogeneity was suggested by the Cochran’s Q test (P < 0.05) for the genetic instruments used in the APOE and PVR MR (Supplementary Table 13). Repeating MR for these two proteins using more strictly independent pQTLs (r2 < 0.001), APOE did not show evidence for heterogeneity (Q test P = 0.37), while its causal effect on delirium remained significant (IVW MR β (s.e.) = −0.57 (0.03); P = 1.13 × 10−78). For PVR, heterogeneity remained high (Q test P = 0.03), and lost significance for its causal effect (IVW MR β (s.e.) = 0.06 (0.06); P = 0.34), suggesting that PVR’s initially observed significant MR effect may be driven by pleiotropy and linkage disequilibrium of its genetic instruments with the APOE-ε4 haplotype that is located in close proximity. Using delirium in the dementia-free UKB GWAS as outcome, ADAM8, CCL25, PILRA and LAYN lost their MR causal effect significance (FDR q > 0.05). A summary of analyses supporting each protein’s association with delirium is presented in Table 1, with full summary results in Supplementary Data 1.
MR associations were derived using the IVW or Wald ratio method and UKB delirium GWAS summary statistics. Only significant (two-sided FDR q < 0.05) MR associations are shown. Effects are presented as IVW/Wald ratio log OR ± 95% CI. Replication MR was conducted using delirium GWAS summary statistics from FinnGen. Colors are assigned to proteins based on their significance in the PWAS logistic regression analysis: Bonferroni, unadjusted two-sided P < 1.7 × 10−5; FDR, FDR-adjusted two-sided q < 0.05; nominal, unadjusted two-sided P < 0.05 and having consistent direction of effect.
Colocalization
We further conducted colocalization analysis to test whether the protein and delirium genetic effects are exerted by the same rather than distinct genetic variants in each genomic region. A total of 37 proteins colocalized with delirium within the APOE genomic region (Supplementary Table 14 and Supplementary Data 2) with high probability (posterior probability of a shared causal variant, PP.H4 > 0.9 as per colocalization software notation39). Overall, 30 more proteins showed suggestive evidence of colocalization with delirium throughout the genome (PP.H4 > 0.5). It should be noted that colocalization methods are generally not well powered to detect shared casual genetic signals unless both traits show strong genetic support (GWAS P < 5 × 10−8)39,40. Here, only the APOE region is strongly associated with delirium; thus many colocalization signals in other parts of the genome may be missed.
Druggability assessment
For delirium-associated proteins with support from both our PWAS and MR analyses, we assessed their suitability to act as drug targets (Table 1). We used the ‘druggable genome’ curated by Finan et al.41, a resource that stratified human proteins on tiers based on the strength of their druggability evidence. Of the selected proteins, PON3 belonged in the druggability tier 1 (targets of approved drugs or clinical-phase drug candidates); ADAM8 and GGH belonged in tier 2 (‘targets with known bioactive drug-like small-molecule binding partners’41 or having high similarity with approved drug targets); PVR, APOE, DPP10 and CCL25 in tier 3 (secreted or extracellular proteins, proteins with medium similarity to approved drug targets, and members of key druggable gene families not included in tier 1 or 2; ref. 41). DSC2, NT5C1A, PILRA and LAYN did not have druggability information.
KGWAS
Knowledge graph GWAS (KGWAS) analysis of our GWAMA summary statistics revealed four disease-critical genes within the APOE genomic region (APOE, TOMM40, PVRL2 and BCAM), prioritized via functional genomics knowledge graph42. All of the KGWAS-identified significant SNPs were also significant in our GWAMA (Supplementary Table 15).
Discussion
In this analysis we conducted a multi-ancestry genome-wide meta-analysis on delirium. Genetic variants on the APOE gene on chromosome 19 were identified as significantly associated with delirium, with the top variant hit, rs429358, showing population-specific association patterns. The APOE gene encodes for APOE, a lipid transporter protein in the periphery and the brain. APOE is a strong risk factor for AD, through its diverse roles in pathways such as amyloid-β plaque deposition, neuroinflammation and dysregulation of lipid metabolism in the brain43.
The role of the APOE gene in delirium is currently unclear, with previous meta-analyses reporting no association between APOE and delirium12,23. In UKB, a previous study on European participants found an association between APOE-ε4 status and delirium (hazard ratio 3.73, 2.68–5.21)44. It has been suggested that interactions between APOE-ε4 and inflammation-related proteins can drive delirium development6. To assess this hypothesis, we tested whether the interaction term between each plasma protein level and APOE-ε4 status significantly associated with incident delirium (Supplementary Table 6). No protein × APOE-ε4 interaction reached significance adjusted for multiple testing (P value threshold = 1.7 × 10−5). CEND1 protein, whose interaction with APOE-ε4 was marginally below significance threshold, is a mitochondrial neural differentiation protein, expressed in the nervous system45. It has previously been implicated in cognitive impairment in mice45 and AD in human46 brains. Additionally, APOE-ε4 expression in astrocytes has been implicated in impaired mitochondrial function47, although to our knowledge CEND1 and APOE have not been linked in previous studies. CEND1 role in delirium has also not been investigated so far.
Ancestry-dependent APOE-ε4 genetic effects on delirium have not been systematically assessed previously. For AD, the risk conferred by APOE-ε4 varies by ancestral background, with African/African Americans and Hispanics having less pronounced risk than white Europeans and Asians48,49. Additionally, higher APOE-ε4 expression levels have been observed in carries of European compared to African ancestry50. Here, findings suggest a similar pattern, with rs429358-C having a higher effect in European, Finnish and south Asian populations than African and Hispanic/Admixed American populations. Overall, subpopulations from the USA (AoU and MGI) have weaker APOE effects than those from the UK or Finland (UKB and FinnGen). This might reflect the younger age of participants in USA-based studies (Supplementary Table 1) or phenotypic differences in delirium diagnoses across the healthcare systems of different countries. Age-dependent genetic effects have been previously described for APOE-ε4 with regard to AD48,51 and progression to mild cognitive impairment and AD52, showing increasing effects until an age of 70–75 years, with reduced effect on later ages48,51,52.
It is also possible that underlying dementia is driving the strong association between APOE and delirium observed here. A total of 36% of UKB European delirium cases had a dementia diagnosis, compared to 1.4% in the control group (Supplementary Table 1). This is to be expected given the close relationship of the two disorders6, but it may hide delirium-specific genetic effects and overemphasize the role of APOE. To this end, APOE remained significant in our range of sensitivity analyses (GWAS adjusting for all-cause dementia (Extended Data Fig. 3), mediation analysis (Fig. 4), dementia and AD-stratified GWAS (Extended Data Figs. 4–5 and Supplementary Table 2)) although with weaker effect. This result may suggest that APOE association with delirium is not entirely through its role in dementia or AD.
Regarding our mediation analysis, it should be noted that unmeasured confounding could bias the estimate of APOE’s direct effect on delirium36,53 (Methods). Unmeasured confounding between APOE (exposure) and dementia (mediator) or delirium (outcome) could be introduced by residual population stratification or linkage disequilibrium between APOE-ε4 and linked causal genetic variants. It is also possible that APOE-induced pleiotropic genetic effects can confound the delirium–dementia relationship, also introducing bias. Our results remained significant after adjusting for possible confounders between dementia and delirium (shared risk factors such as cognitive function, socioeconomic deprivation and comorbidity burden)3,4,5,54,55. None of the additional confounders had an independent OR effect on both delirium and dementia above 1.54 each, the minimum required to explain away the observed APOE direct effect on delirium; however, some residual confounding may still remain, for example due to precipitating factors of delirium episodes during hospitalization, such as infections, medication status, sleep disruptions or severity of presenting illness. These factors have been previously estimated to have a strong effect on delirium3,4, and may be also related to dementia55. Assessing the effect of those factors was outside the scope of our study.
Adjusting for APOE-ε4 attenuated the genetic effects within the whole APOE region. This observation suggests that the significance of the genetic variants in the close proximity is driven by linkage disequilibrium with the APOE-ε4 haplotype, not secondary independent signals. Moreover, an intronic variant on the ADAM32 gene gained significance after adjusting for APOE-ε4. ADAM32 belongs to the ADAM family of metalloproteinases, some of which have been implicated in AD56. ADAM proteins are involved in diverse functions, including immunity-related pathways57.
Regarding our multi-trait analysis of delirium with AD (MTAG), five genetic loci were found to have a significant effect on delirium, supported by replication in the AoU EUR cohort. Among the replicated loci, several important AD risk genes58 were detected: BIN1, CLU, CR1, MS4A4A and TOMM40. The MS4A4A gene is expressed in macrophages and has been linked with AD59, vascular dementia and systemic lupus erythematosus60. The lead variant’s minor allele on the MS4A4A gene, rs1582763, has been previously associated with decreased risk of AD59. This variant’s association with delirium has not been reported before, but we also found a protective effect of the rs1582763 minor allele on delirium. BIN1 has been recently implicated in the regulation of calcium homeostasis in glutamatergic neurons, and its expression in AD human brains is reduced compared to healthy brains61. The clusterin gene (CLU), also named Apolipoprotein J (APOJ), codes for a multifactorial protein, with an apparent role in neurodegenerative diseases62. CLU, much like APOE, is thought to be involved in amyloid-β plaque deposition in AD pathologies. With regard to delirium, protein expression of apolipoproteins including CLU and APOE were previously found to be downregulated in the CSF of people with delirium compared to those with mild AD63. In our proteomic analysis, CLU protein levels were also downregulated in the plasma of people with incident delirium (Supplementary Table 3), but not significantly (P > 0.05). This discrepancy may reflect different CLU protein abundance between CSF and plasma tissues. The CR1 gene, implicated in complement activation, is believed to exert its role to AD pathogenesis through amyloid-β clearance, neuroinflammation and tauopathy (the deposition of abnormal tau protein in the brain)64. To the best of our knowledge, the role of CR1 in delirium has not been investigated previously. In our study, CR1 plasma protein levels had a nominally significant association with incident delirium (P = 0.013). TOMM40 genetic variants have been associated with AD previously65. Given TOMM40’s close proximity and high linkage disequilibrium with the APOE gene, its role in AD has frequently been contested65; however, it has also been suggested that TOMM40 independently affects AD risk through its encoding protein’s role in regulating protein transportation in mitochondria65,66. TOMM40 has not been previously implicated in delirium. Overall, given the small effect sizes of the MTAG-identified genes for delirium (Supplementary Table 2), and their prominent role in AD, it may be possible that their significance in our analysis is mainly driven due to their role in AD. Nonetheless, our findings suggest newly identified genes (for example MS4A4A, CR1 and TOMM40) that may be of relevance to future delirium research and therapeutic targets investigations.
Previous proteomic studies for delirium have, to our knowledge, focused on the protein landscape shortly before or following delirium episodes31. Our proteomic study has a large follow-up period between protein measurements and delirium incidence (median time to first delirium event of 11.4 years, interquartile range 9.5–12.7), allowing the identification of relevant biomarkers and biological mechanisms at an early stage, such as several neurologically relevant and immune system-related proteins.
For example, we found plasma GFAP and NEFL levels (biomarkers of neuronal injury) to be associated with incident delirium. Previous research paints a complex, possibly bidirectional relationship between neuronal injury and delirium. Increased plasma and CSF NEFL levels, a marker of neuroaxonal injury, have been observed in patients with delirium pre- and postoperatively6,8,9,67,68. It is unclear, however, whether this is due to underlying neurodegeneration (for example due to preclinical dementia) or a feature of delirium6. In our proteomic analyses we observed significant and consistent effect of NEFL on incident delirium in both the full and dementia-free populations. This may implicate neuroaxonal injury as an underlying driver of delirium independently of dementia-related neurodegeneration, even long before hospitalization. Our findings, thus, add support for the role of NEFL as a useful predictive biomarker for delirium6.
GFAP is an astrogliosis marker; there is an increase in astrocyte levels in the CNS in response to injury. High GFAP levels have been observed previously in postmortem brains of people with delirium69, in the CSF of those with persistent delirium8 and in the blood and CSF of patients with delirium undergoing elective surgery32,67. In our analysis, GFAP was only predictive of incident delirium in our full proteomic set (Supplementary Table 4), not in the dementia-free population (Supplementary Tables 8 and 9). This may indicate that, in the years preceding delirium, astrogliosis is only relevant for delirium in the context of underlying dementia. GFAP may be more useful as a delirium biomarker in the short term, possibly in patients with traumatic brain injury or underlying neurodegeneration.
Systemic inflammation markers have been observed among the delirium-associated proteins in our study. For instance, C7, BTLA and FGL1 participate in the immune response, whereas LRG1 and LTA4H in inflammatory processes. LRG1 has been implicated in brain injury after sepsis in mice70, sepsis being a main driver of delirium etiology3. Interleukins, identified through our enrichment analysis, play an important role in regulating immune response and inflammation and have frequently been implicated in delirium71,72. Indeed, IL-6 (found to have a strong delirium association in our PWAS) is among the most consistently identified biomarkers of delirium and markers of postoperative cognitive decline31,32. All the inflammatory-related proteins were significant in our dementia-free sensitivity analyses, suggesting a role for delirium partially independent of dementia pathology.
Other notable proteins robustly associated with delirium in our proteomic analysis are BCAN, SELENOP, AREG and MSLN. BCAN, a protein with a role in brain extracellular matrix formation, has been observed to be downregulated in brains of post-infection delirium and in patients with AD73. Lower plasma levels of SELENOP, an important selenium transporter in the brain, have been associated with worse global cognition and AD74. To the best of our knowledge, an association between SELENOP and delirium has not been reported previously. The associations of AREG and MSLN with delirium were also notable findings. AREG is a member of epidermal growth factor protein family, involved in many aspects of cell proliferation75. Possible mechanisms linking AREG to delirium could include neuroinflammation and regulation of T cells in astrocytes in sepsis-associated delirium76, type 2 inflammatory response and tolerance against pathogens77, or tumor development75. MSLN is a mesothelial cell surface glycoprotein, overexpressed in many cancers78. Delirium is common in patients with cancer, arising either as a complication of the disease or indirectly through medical and surgical intervention for cancer treatment79. Further research on the overlapping pathophysiology between delirium and cancer (for example, shared biomarkers80) is important for better management of delirium throughout cancer care trajectories79.
Overall, our proteomic analysis results align with the proposed mechanisms of delirium pathophysiology (brain vulnerability, indicated by brain injury marker proteins), systemic and nervous system inflammation being driving factors for delirium3,6. At the same time, our results could inform future research in delirium prediction biomarkers, some of which are first reported in delirium research (for example SELENOP, CEND1, AREG and MSLN).
Our findings have notable clinical and biological clinical implications. We found that APOE-ε4 is a robust genetic risk factor, remaining significant after adjustment for presence of dementia. The findings suggest that APOE-ε4 confers vulnerability to adverse acute brain changes induced by triggers of delirium. Indeed, it is known that APOE-ε4 is associated with exaggerated neuroinflammatory responses81, altered blood–brain barrier integrity82,83, increased β-amyloid accumulation following various injuries84 and increased white matter pathology85. APOE-ε4 therefore could contribute to increased risk of delirium and also cause or amplify neuropathological changes linked with dementia. A key next step is to test whether APOE-ε4 carriers are disproportionately likely to develop new dementia after a delirium episode, even in the absence of previous cognitive impairment.
Clinically, APOE-ε4 status has potential to assist in stratification for delirium prevention trials, in prediction of dementia following delirium and as a target for neuroprotective therapies during acute illness, especially if delirium is present. Animal studies targeting APOE have shown encouraging results in terms of improving AD phenotypes83. Some promising therapeutic approaches include increasing APOE levels and lipidation, APOE mimetics (small peptides mimicking APOE’s receptor-binding structure) and APOE-ε4 gene therapy43,83; however, therapeutic translation in human clinical trials is still limited83. A currently unpublished phase 2 clinical trial (NCT03802396)86 found that administration of CN-105 (an APOE mimetic drug) lowered postoperative delirium incidence and severity compared to administration of placebo, but not significantly. Further clinical research is needed to clarify the therapeutic potential of APOE-targeting therapies.
In terms of delirium treatment, we explored whether our identified proteins could be suitable drug targets. For this, we triangulated our proteomic study findings with proteome-wide MR and colocalization analyses. Incorporating genetics in drug target identification, for example through MR, is particularity attractive, as drugs with genetic support are more likely to be successful in clinical trials87,88 or can offer drug repurposing opportunities89. Our druggability assessment found PON3 to be a notable drug target for delirium. PON3 is a secreted high-density lipoprotein-associated enzyme90, participating in the metabolism of the statin lovastatin, a licensed lipid-lowering medication. The role of statins in delirium management is unclear. Statin usage has been associated with improved delirium outcomes in randomized controlled trials and observational studies, but overall evidence is inconsistent, with a recent meta-analysis finding no significant protective effect and high heterogeneity91. In our analysis, increased PON3 plasma level was found to have protective effect against delirium. This is consistent with high PON3 levels being protective against atherosclerosis and cardiovascular disease92, possibly through its antioxidant action92,93. It is not clear, however, how PON3 levels can affect statin metabolism. It may be possible that PON3 can affect lovastatin and other statins’ efficacy via their involvement in the drug activation90, which may explain part of the high heterogeneity observed regarding statins’ effect on delirium91. Our results may, thus, suggest a reconsideration of a possible role for statins in improving delirium prevention or treatment.
Additionally, we identified proteins previously suggested as therapeutic targets for cancers (ADAM8 (ref. 94), GGH95 and PILRΑ96) and AD (PILRA97). This may offer promising opportunities for investigating new delirium treatment targets; however, results should be interpreted with caution, as liberal P value thresholds (up to P < 0.05) were used to indicate proteomic support for our druggability assessment, and some proteins (for example, PON3 and ADAM8) were not replicated in our replication MR, although the same effect direction was still observed (Table 1 and Supplementary Data 1).
The main strength of our analysis is the large-scale investigation of delirium genetic and proteomic risk factors. Both in terms of sample size, follow-up time before protein measurement and delirium episodes and number of genetic variants/proteins tested, this is a large study on the molecular background of delirium risk. On the other hand, some of the limitations of the study include the underdiagnosis of delirium in hospital health records from which the phenotype was mostly derived98. This misclassification could introduce noise to the results, limiting discovery of genetic and protein effects. Also, the small sample sizes of the non-European subpopulations hinder the identification of risk factors specific to them. Moreover, the full spectrum of the human proteome is not captured in the assayed plasma proteins, potentially missing proteins that are important for delirium biology and prognosis. Finally, although the use of plasma proteins as predictive biomarkers is of great importance, proteomic profiles of delirium-relevant tissues, such as the brain or CSF would be invaluable.
In conclusion, our results point out to an oligogenic genetic architecture for delirium, with the APOE locus identified as a strong, potentially population-specific genetic risk factor, independently of dementia; however, further replication in larger non-European cohorts is required. Our plasma proteome analysis supports previous findings and discovers proteins putatively implicated to delirium, some of which are suggested for therapeutic applications. Taken together, genetic and proteomic risk factors suggest a shared etiology between delirium and dementias, possibly contributing to a better understanding of delirium’s complex biological origin and the discovery of clinically relevant biomarkers.
Methods
Ethics statement
The UKB project was approved by the National Research Ethics Service Committee North West-Haydock (REC reference 11/NW/0382). Participants provided written informed consent to participate in the UKB. An electronic signed consent was obtained from the participants.
For the AoU Research Program, informed consent for all participants is conducted in person or through an eConsent platform that includes primary consent, HIPAA Authorization for Research electronic health records (EHRs) and Consent for Return of Genomic Results. The protocol was reviewed by the Institutional Review Board of the AoU Research Program, which follows the regulations and guidance of the National Institutes of Health (NIH) Office for Human Research Protections for all studies, ensuring that the rights and welfare of research participants are overseen and protected uniformly.
Study populations
The project utilizes biomedical data from ancestrally diverse large-scale cohorts. Included cohorts were either (1) databases containing individual-level genomic measurements linked to healthcare records or (2) previously published summary results from genomic studies on delirium phenotypes. Contributing individual-level cohorts include the UKB33,99 and the AoU Research Program100. Summary results have been obtained from ancestrally Finnish (FinnGen101; \({n}_{\mathrm{cases}}=\mathrm{3,371}\); \({n}_{\mathrm{controls}}=\mathrm{388,560}\)) and European participants (MGI cohort102; \({n}_{\mathrm{cases}}=160\); \({n}_{\mathrm{controls}}=\mathrm{44,654}\)).
The UKB is a population-based prospective study, containing a rich set of genetic and phenotypic data for approximately 500,000 participants living across the UK. Participants, aged 40–69 years at recruitment between 2006 and 2010, have been linked to their annually updated EHRs, allowing longitudinal investigation of healthcare outcomes. Similarly, AoU includes genomic data and healthcare outcomes for approximately 245,000 individuals from diverse populations in the USA.
Age distributions for UKB and AoU participants, along with delirium and all-cause dementia prevalence by age group, can be found in Extended Data Fig. 1. Age distributions for the FinnGen and MGI cohort can be found in their respective original publications (Kurki et al., Supplementary Methods101 and Zawistowski et al.102, respectively). Age distribution of delirium first events in FinnGen can be found at https://r10.risteys.finregistry.fi/endpoints/F5_DELIRIUM.
Delirium phenotype
The analysis focused on delirium episodes that were not triggered by substance intoxication or withdrawal2. For convenience, such delirium episodes will hereby be referred to as simply ‘delirium’. Delirium cases were defined as individuals with one or more delirium-corresponding codes in their EHRs (hospital inpatient, death register or primary care data). The relevant codes were ‘F05’ (delirium, not induced by alcohol and other psychoactive substances) for ICD-10 (ref. 103) and ‘293.0’ (acute confusional state) for ICD-9 (ref. 104). Read v2 and v3 codes105 for primary care data mapping to delirium were obtained from a previously defined list by Kuan et al.106, published in the HDRUK Phenotype Library (https://phenotypes.healthdatagateway.org/).
Discovery of genetic risk factors
A GWAS framework was implemented to identify genetic variants associated with delirium in UKB’s and AoU’s ancestrally distinct subpopulations. For this purpose, the REGENIE software (v.3.2.2) was used, which carries out a logistic regression analysis between a disease phenotype and each genetic variant, accounting for covariates, population structure and relatedness of participants107.
In UKB, the set of imputed genotypes was used33 (data field 22828), filtered to include variants with >5 minor alleles in cases and controls, imputation score >0.5, missingness rate <3% and deviation from Hardy–Weinberg Equilibrium (HWE) with P value < 10−6. Individuals were filtered to include those with missingness rate <5%, no mismatch between reported and genetically inferred sex (data field 22001), no sex chromosome aneuploidy (data field 22019), no excessive heterozygosity (data field 22027) and no more than ten third-degree relatives (data field 22021). The covariates considered for the UKB GWAS included age, sex, genotyping batch (data field 22000) and the first 20 precomputed genomic principal components (data field 22009). Here, age was defined as age at first delirium occurrence for cases and age at last data freeze (31 October 2022) or age at death for controls. GWAS were conducted separately for subpopulations of white British ancestry (EUR; \({n}_{\mathrm{cases}}=7,176\); \({n}_{\mathrm{controls}}=385,097\)), African (AFR; black/black British; \({n}_{\mathrm{cases}}=115\); \({n}_{\mathrm{controls}}=7,480\)) and south Asian (SAS; \({n}_{\mathrm{cases}}=107\); \({n}_{\mathrm{controls}}=9,356\)) ethnic backgrounds. Summary statistics from the UKB GWAS were converted from GRCh37 to GRCh38 genomic coordinates using the LiftOver software108. In total the analysis covered approximately 22.5, 13.6 and 8.8 million genetic variants in EUR, AFR and SAS ancestries respectively.
In AoU, short-read whole-genome-sequencing genotypes were used100 for conducting GWAS on European (EUR; \({n}_{\mathrm{cases}}=652\); \({n}_{\mathrm{controls}}=119,817\)), African/African American (AFR; \({n}_{\mathrm{cases}}=233\); \({n}_{{\mathrm{controls}}}=52,300\)) and admixed American/Hispanic (AMR; \({n}_{\mathrm{cases}}=117\); \({n}_{\mathrm{controls}}=39,977\)) subpopulations. The same GWAS framework as described for UKB was followed, except that it did not include genotyping batch and principal components 11–20 as covariates, as they were not available in the AoU datasets. Subpopulations with a low number of delirium cases (<20) were excluded from the analysis. Those consisted of east Asian ethnic background in UKB and east Asian and middle Eastern genetic ancestries in AoU.
To increase power to detect genetic associations, our GWAS summary statistics and previously published GWAS results were combined into a multi-ancestry genome-wide meta-analysis. The METAL software (v.2020-05-05)109 was used to conduct a fixed effects inverse-variance meta-analysis on the set of 24,951,029 variants that were present in at least two studies. The genomic control correction method was applied in METAL to allow for multi-ancestry analysis. In total, up to 1,059,130 individuals (\({n}_{\mathrm{cases}}=11,931\); \({n}_{\mathrm{controls}}=\mathrm{1,047,199}\)) were included in the meta-analysis. Genome-wide significance was considered at a P value threshold of 5 × 10−8. Significantly associated variants at the multi-ancestry meta-analysis were inspected for consistency at each contributing subcohort. Descriptive statistics for each subcohort are presented in Supplementary Table 1.
Wherever reported, ORs were calculated as \(\mathrm{OR}={e}^{\beta }\), where \(\beta\) is the logistic regression coefficient. 95% CI for the ORs were calculated as \({\mathrm{OR}}_{95 \% \mathrm{CI}}\,={e}^{\beta }\pm 1.96\times {\rm{s}}.{\rm{e}}{.}_{\beta }\times {e}^{\beta }\).
Sensitivity analyses
A series of sensitivity analyses were conducted in addition to our main genetic analysis, to:
-
Identify genetic variants associated with delirium independently of APOE. For this purpose, we performed a GWAS on the UKB EUR cohort conditional on the APOE-ε4 haplotype count (0, 1 or 2) (Extended Data Fig. 2). We inferred APOE-ε4 haplotypes for each participant based on their rs429358 and rs7412 genotypes, as described in previous studies35.
-
Identify genetic signals for delirium independently of dementia. To this end, we conducted in the UKB EUR cohort (1) delirium GWAS conditional on dementia (dementia-adjusted), by including all-cause dementia status as a covariate (Extended Data Fig. 3); (2) delirium GWAS on subcohorts stratified by all-cause dementia status (whether or not individuals have developed all-cause dementia at any time point) (Extended Data Fig. 4); and similarly (3) delirium GWAS on subcohorts stratified by AD status (Extended Data Fig. 5).
-
Better distinguish genetic signals in true delirium cases and controls in the older adults, by conducting a delirium GWAS on UKB EUR participants aged 60 years or older (Extended Data Fig. 6).
For all sensitivity analyses, the same GWAS framework as in our main analysis of genetic risk factors was followed. All sensitivity analyses were repeated in the AoU EUR cohort for replication (significance P value threshold <0.05). Sample sizes for each analysis and results for rs429358, the top delirium-associated genetic variant from our main genetic risk factor analysis, are presented in Supplementary Table 2.
For the analyses that utilized dementia or AD status in UKB, the algorithmically defined all-cause outcomes were used (data field 42018), provided by UKB. Briefly, disease outcomes were constructed based on self-reported medical conditions reported at the baseline assessment, ICD-9/10 codes in hospital diagnoses and procedures, and ICD-10 codes in death register records. The full list of ICD codes for all-cause dementia and AD is included in Supplementary Table 16 (as reported in UKB Recourse 460, https://biobank.ctsu.ox.ac.uk/ukb/refer.cgi?id=460). All-cause dementia and AD diagnoses codes for the AoU cohort are reported in Supplementary Table 17.
Multi-trait analysis between delirium and AD
Given the close inter-relationship between delirium and AD6, we wanted to quantify the shared genetic architecture between the two traits. For this purpose, we used the high-definition likelihood (HDL) software (v.1.4.0)110 to estimate the SNP heritability (\({h}_{\mathrm{SNP}}^{2}\)) of delirium and the genetic correlation (\({r}_{g}\)) between delirium and AD using GWAS summary statistics. SNP heritability, the proportion of phenotypic variance explained by the additive SNP genetic factors111, was estimated in the observed scale, and converted to the liability scale using the equation: \({h}_{\mathrm{SNP},l}^{2}={h}_{\mathrm{SNP}}^{2}\frac{K(1-K)}{{z}^{2}}\frac{K(1-K)}{P(1-P)}\), where \(K\) = 0.015 is the population prevalence of delirium4, \(P\) = 0.018 is delirium prevalence in UKB, and \(z\) is standard normal probability density function’s height at the quantile corresponding to cumulative probability \(K\). The equation is derived from Lee et al.112. Genetic correlation is a measure of the variance shared by two traits due to genetic causes111. For AD, we used the largest to-date AD GWAS meta-analysis of Bellenguez et al.58. The AD GWAS was conducted on 487,511 European individuals (stage I, 39,106 clinically diagnosed AD cases and 46,828 proxy AD cases) and 21 million variants. AD summary statistics were obtained from European Bioinformatics Institute GWAS Catalog (https://www.ebi.ac.uk/gwas/) under accession no. GCST90027158. Delirium summary statistics were taken from our UKB EUR GWAS subcohort, to better match the ancestry of the AD GWAS summary statistics and the HDL precomputed European-ancestry reference panel.
We also applied a joint analysis of summary statistics between delirium and AD. Such approach increases statistical power to detect genetic associations for each trait34. The multi-trait analysis of GWAS (MTAG) software (v1.0.8) was used for this purpose34, jointly analyzing summary statistics from our delirium meta-analysis (excluding the AoU sets) and the Bellenguez et al.58 AD summary statistics. The MTAG analysis for the discovery of delirium genetic risk variants was conducted on 9,883,704 SNPs that overlapped across the two disorders, filtered for minor allele frequency ≥ 0.01 and sample size N ≥ (2/3) × 90th percentile for each trait. MTAG results are trait-specific summary statistics (effect estimates, s.e. and P values), interpreted similarly with single-trait GWAS results. The genome-wide significance threshold was defined as a P value = 5 × 10−8. Independent lead variants were defined as the most significant variants within a ± 500-kb region, using the GWASLab Python package (v.3.4.46)113.
The AoU EUR set was held out for replication of the MTAG lead hits. A multi-trait analysis with AD was conducted on the replication set as described for the discovery MTAG. Lead variants were considered replicated if they had a Bonferroni-adjusted P value < (0.05/number of lead variants) and same direction of effect across the discovery and replication set.
Mediation analysis
We employed a mediation analysis framework to quantify to what extent the effect of APOE gene on delirium is mediated through underlying dementia status. Mediation analysis enables the decomposition of an exposure’s total causal effect on an outcome, here APOE and delirium respectively, into direct and indirect effect through a hypothesized mediator variable (here dementia)53. We used the R package ‘medflex’53 (v.0.6-10) to calculate the so-called natural direct and natural indirect effects of the number of APOE-ε4 haplotypes (0, 1 and 2) on delirium, mediated through dementia. When exponentiated, natural direct and indirect effect estimates can be interpreted as ORs. Medflex’s weighting-based approach was used, to estimate the unobserved potential outcomes. For the natural effect model’s parameters, bootstrap-based (n = 1,000) s.e. and Wald-type two-sided P values were obtained. Sex and age were used as covariates.
Mediation analysis, as implemented under the counterfactual framework in ‘medflex’, relies on the assumption that, after adjusting for baseline covariates, there is no unmeasured confounding between (1) exposure and outcome, (2) exposure and mediator and (3) mediator and outcome53. It is also assumed that (4) there are no confounders of the mediator–outcome relationship that are themselves induced by the exposure53. We assessed the robustness of our mediation analysis to violations of unmeasured confounding assumptions, using the E-value sensitivity analysis method36,114. An E-value, calculated as \({RR}+\sqrt{{RR}\times ({RR}-1)}\), where \({RR}\approx {\rm{OR}},{\rm{for\; OR}} > 1\) is the observed direct or indirect effect risk ratio114, can be interpreted as the minimum unmeasured confounder effect size required to completely explain away the observed effect36.
We also conducted a sensitivity mediation analysis additionally adjusted for measurements of cognitive function, socioeconomic deprivation and chronic disease burden, to assess the robustness of our analysis to common dementia and delirium risk factors4. General cognitive ability was calculated as a composite measure (the first unrotated principal component) of four UKB cognitive tests: fluid intelligence (data field 20016), numeric memory (data field 4282), reaction time (data field 20023, log transformed) and visual memory (data field 399, log1p transformed), as described and validated in previous studies115,116. When cognitive tests were unavailable at baseline, measurements of the same tests at repeat assessments or online follow-up were used if available. The Townsend deprivation index immediately before joining UKB (data field 22189, decile transformed) was used as a measure of socioeconomic deprivation117. The Charlson comorbidity index (CCI) was calculated as an estimate of chronic disease burden118. CCI is a weighted sum of 12 chronic comorbid diseases, here calculated at the time of delirium episode. Diseases were extracted from self-reported medical conditions and cancers (data fields 20002 and 20001) and ICD-9 and ICD-10 disease codes119 from linked healthcare records. Weights were obtained from Quan et al.118. This sensitivity analysis was conducted on a subset of n = 141,864 individuals, due to missing cognitive function data.
Proteomic study population
Plasma proteome data were available in UKB for a subset of 53,075 participants. Protein measurements of 2,923 unique plasma proteins120 were derived from blood samples taken during randomly selected participants’ initial UKB assessment visit between 2006 and 2010. Proteins were measured using the antibody-based Olink Explore 3072 proximity extension assay. Proteome data have been previously undergone extensive quality control120. As additional filtering in the present analysis, European participants from batches 0 to 6 were extracted, as they have been reported to be highly representative of the UKB European population120. Moreover, protein measurements with >20% missing data were removed and the remaining proteins were mean-imputed, inverse-rank normalized and standardized (mean zero s.d. 1) to ensure homogeneity across the proteins. Delirium incident cases were defined as the participants whose first reported delirium episode was >1 year after baseline (the date of blood sample collection at the first UKB assessment visit; data field 53-0.0). Delirium data were available for up to 16 years of follow-up after baseline (censoring date 31 October 2022). The final population consisted of 32,652 European participants and 2,919 plasma proteins. A total of 541 participants had an incident delirium diagnosis within the follow-up period (cases). Of the remaining 32,111 participants (controls), 29,440 reached the end of follow-up without a delirium diagnosis and 2,671 died before the end of follow-up. Follow-up information was available for all participants. As inverse-rank normalization was applied, proteomics data distributions were assumed to be normal; however, this was not formally tested.
Discovery of protein risk factors
To explore the relationships between baseline protein levels and incident delirium, we performed a PWAS on the UKB proteomic study population. Multivariable logistic regression models were fit between each protein as predictor and incident delirium status as outcome. In total, 2,919 models were fit, equal to the number of proteins. The models were adjusted for sex, BMI and age at baseline. Associations were deemed significant at a Bonferroni-adjusted P value threshold < 1.7 × 10−5. For sensitivity analyses, we further adjusted protein models for APOE-ε4 haplotype status (zero, one or two copies of the haplotype) and for interaction between each protein and APOE-ε4.
We performed a pathway enrichment analysis on the set of Bonferroni-adjusted significant proteins emerging from the protein-wide association analysis. We used the Enrichr121 web-based tool and pathway annotations based on the Reactome122, Molecular Signatures Database (MSigDB)123 and Kyoto Encyclopedia of Genes and Genomes (KEGG)124 databases. The full set of Olink proteins was used as background genes. Fisher’s exacts tests were implemented to assess whether the identified proteins significantly overlap with the proteins in any of the pathways. Q-values were obtained by adjusting P values for multiple testing using the Benjamini–Hochberg method.
Protein selection and prediction models
To investigate whether baseline plasma proteome can improve prediction of incident delirium, a supervised machine-learning approach was implemented. The LASSO method37 was utilized for the selection of important proteins and to avoid overfitting given the high multicollinearity of proteomics data. For this analysis, the full set was randomly split into a training (80%; ncases = 436; ncontrols = 25,733) and test (20%; ncases = 105; ncontrols = 6,378) set. A LASSO model for binary outcomes was implemented in the training set using the glmnet R package (v.4.1.8)125. Here, the whole set of 2,919 proteins adjusted for demographic covariates: age, sex and BMI were used as predictors of incident delirium. In brief, the coefficients penalty parameter lambda was tuned using a tenfold cross-validation (CV) framework for 100 lambdas between 10−6 and 0.07. The model with lambda.1se was chosen as the most parsimonious, giving the strictest model such that cross-validated error is within one s.e. of the minimum125. To increase the robustness of the LASSO protein selection, a stability selection38 approach was additionally applied. For each of 100 random subsampling iterations of the training set, including all 436 delirium cases and an equal number of 436 randomly selected controls, a LASSO model as described in the present section was fit using the penalty factor tuned in the full training set. The proteins that were selected on at least half of the subsampling iterations were chosen as robustly selected (stability-selected proteins).
Four logistic regression models with incident delirium as outcome were subsequently re-fit in the training set: (1) using only demographic covariates (age, sex and BMI) as predictors (basic model); (2) using only the stability-selected proteins as predictors (proteomic model); (3) using both demographic covariates and the stability-selected proteins as predictors (proteomic + basic model); and (4) using demographics, stability-selected proteins and APOE-ε4 haplotype status as predictors (APOE + proteomic + basic model). For the models that included proteins as predictors (models 2, 3 and 4), stepwise regression models were fit, starting with all the stability-selected proteins and removing predictors until no AIC improvement was observed.
The performance of the models was evaluated in the held-out test set. Receiver operating characteristic (ROC) curves, AUC and PR-AUC estimates were used to compare the predictive performance of the three models in the test set. Precision–recall metrics were chosen as they are more sensitive to binary outcome imbalance126, as is the situation here. Two-sided DeLong tests were used to compare whether AUCs were significantly different between each model pair127 (ΔAUC P value < 0.05).
pQTL analysis
We obtained protein quantitative trait loci (pQTL), which are genetic variants affecting plasma protein levels, from the UKB proteomic study population. A GWAS was conducted for each of the 2,923 inverse-rank normalized and standardized protein traits. Autosomal and X chromosome genetic variants were derived from UKB’s called genotypes (data field 22418), filtered to include variants with missingness <1%, HWE deviation P value > 10−15, minor allele frequency >1%. The proteomic study population was further filtered to include unrelated, up to second-degree, individuals, with missingness rate <10%. The GWAS on each protein were conducted using REGENIE (v.3.2.2)107 on 30,272 individuals and ~540,000 genetic variants. Age, age2, sex, sex × age and sex × age2, batch, UKB assessment center, UKB genetic array, time between blood sampling and measurement and the first 20 genetic principal components were used as covariates.
A total of 2,464 proteins were significantly associated with at least one genetic variant (P < 5 × 10−8). Per-protein, independent pQTLs were obtained through linkage disequilibrium (LD)-based clumping, including variants with LD r2 < 0.2 within ±250-kb windows of the top associated pQTLs. Genotype filtering and LD-clumping was performed using PLINK (v.1.90b)128.
The independent pQTLs derived here were used as genetic instruments for protein levels in the subsequent MR and colocalization analyses.
Mendelian randomization
MR is a method used to assess potential causal influence of a modifiable exposure on an outcome, often disease risk. MR analyses are based on the use of genetic variants as instrumental variables (IVs). IVs are variables associated with an exposure but not with the outcome of interest through any other pathway129,130. Three assumptions are required for MR to be valid: (1) IVs are significantly associated with the exposure; (2) there are no confounders of the IVs and the outcome; and (3) IVs do not affect the outcome other than through the exposure (no pleiotropy)129.
We assessed whether the identified protein risk factors (exposures) showed causal effects on delirium (outcome), using a two-sample MR approach131. Genetic instruments for protein exposure traits comprised of the per-protein independent pQTLs, as derived from our pQTL analysis in UKB (P value < 5 × 10−8, LD r2 < 0.2). To further ensure no weak instrument bias in our genetic instrument pQTLs (relevant to MR assumption (1)) we also excluded pQTLs with an F-statistic < 10 in their per-protein exposure GWAS. F-statistics were approximated as \(F=\frac{\widehat{{\gamma }_{j}^{2}}}{{\sigma }_{j}^{2}}\) for each pQTL j, where \(\hat{\gamma }\) is the pQTL exposure effect size and \(\sigma\) is its respective s.e.132. To minimize the chances of including genetic instruments with pleiotropic effects, we included only (1) pQTLs associated with fewer than five proteins (P value < 5 × 10−8) and (2) cis-pQTLs (pQTLs in close proximity with their associated protein’s encoding gene). cis-pQTLs were defined as being located within ±1 Mb (106 base pairs) of the protein-encoding gene’s coding region. Protein-encoding genes’ start and end positions were derived as reported in the metadata from Sun et al.120. Genetic associations of the pQTLs with delirium were derived from our UKB EUR GWAS, excluding the individuals in the proteomic set, to avoid sample overlap in our two-sample setting (\({n}_{\mathrm{cases}}=\mathrm{6,650}\); \({n}_{\mathrm{controls}}=354,251\)). The same procedure as our full UKB EUR GWAS was followed, as described in the section ‘Discovery of genetic risk factors’.
For our main MR analysis, 1,989 proteins were tested in total. The IVW method was used133 to assess causal estimates between 1,738 proteins with more than one cis-pQTL and delirium. For 251 proteins with one cis-pQTL the Wald ratio method was used. We further employed the WM, maximum likelihood and MR-Egger sensitivity MR methods134, to test for consistency of estimates with our main analysis. The MR-Egger intercept and the Cochran’s Q tests were used to assess for the presence of horizontal pleiotropy and heterogeneity in the IVs, respectively135,136,137. MR associations were considered significant at an FDR q < 0.05 in our main IVW or Wald ratio MR analysis. For significant proteins, IVW or Wald ratio MR were repeated using delirium in the dementia-free UKB subcohort as outcome GWAS, again using an FDR q threshold of 0.05. Finally, the FinnGen delirium GWAS was used as a replication MR outcome set, following the same MR framework as described above for the UKB EUR delirium GWAS outcome. A significance threshold of P value < 0.05 was used in the replication MR. Full MR results are reported in Supplementary Tables 12 and 13. All MR analyses were conducted using the TwoSampleMR R package (v.0.5.11)134. A full list of the cis-pQTLs used, together with their association statistics with each exposure and delirium, is available in Supplementary Data 3. A STROBE-MR checklist130 for the conducted MR analyses can be found in Supplementary Table 18.
Colocalization
We tested whether genetic signals for delirium and each of the plasma proteins colocalize (the two traits are affected by the same, rather than distinct genetic variants in a specific genomic region)40. For each of the 2,456 proteins with at least one pQTL, we analyzed genomic regions around lead pQTLs with boundaries defined by recombination hotspot locations, based on a previously published map138 (https://bitbucket.org/nygcresearch/ldetect-data/src/master/EUR). We used the coloc R package (v.5.2.3)39, specifically the Approximate Bayes Factor colocalization method (coloc.abf), which assumes at most one causal variant per trait per region39. Using per-trait GWAS results and the default prior probabilities of \({{p}}1={{p}}2={10}^{-4}\) for each variant being the causal for delirium or the analyzed protein respectively and \({p12=10}^{-5}\) for each variant being the causal for both, coloc.abf calculates per-variant posterior probabilities that the two traits have a common causal genetic variant in a genomic region (PP.H4 as per colocalization notation). Proteins and delirium were considered to share a causal genetic variant when PP.H4 > 0.9. Suggestive colocalization was considered for protein–delirium pairs with PP.H4 > 0.5. The colocalization assumption of one causal variant per trait was not formally tested.
Druggability assessment
We further investigated whether selected delirium-associated proteins are suitable to act as potential drug targets. The selected proteins included those identified as significant in both our protein risk factor (P < 0.05) and MR analyses (FDR q < 0.05), as well as having a consistent direction of effect in the two analyses. We utilized the ‘druggable genome’ resource developed by Finan et al.41. In this resource 4,479 genes encoding drugged or druggable proteins were systematically identified, and further stratified into three tiers based on druggability evidence strength, as described on the original publication41. We therefore tested whether our selected proteins overlap with the druggable genes’ encoding proteins. For proteins in tier 1 druggability we searched the Drug Bank (https://www.drugbank.ca/) and https://clinicaltrials.gov/ databases for additional information on drug indications and clinical trial status, respectively. The druggable genome can be found in Supplementary Table 1 of the original Finan et al. publication41.
KGWAS
We implemented Knowledge Graph GWAS (KGWAS), a novel geometric deep-learning approach that integrates GWAS summary statistics with functional genomics data (variant and gene-level annotations and interactions), to improve power in GWAS association testing42. Using functional genomics knowledge graphs, KGWAS estimates variants’ prior relevance to disease and recomputes the original GWAS associations in a P value weighting framework. We used our delirium GWAMA summary statistics and KGWAS’s default fast mode, which uses Enformer embedding for variant features and Evolutionary Scale Modeling embedding for gene features. We further used MAGMA139, as integrated in KGWAS, for gene prioritization of KGWAS significant associations. We used a P value threshold of 0.05/16,637 = 3 × 10−6 for gene-based P values estimated by MAGMA, with 16,637 genes tested.
Statistics and reproducibility
Sample sizes
No statistical methods were used to predetermine sample sizes, but our sample sizes are larger than those reported in similar publications for delirium28,71 and similar to previous genetic and proteomic studies in other traits58,120. The sample sizes were as follows:
-
For the GWAS, sample sizes for each contributing cohort are described in Supplementary Table 1. For the overall meta-analysis n = 1,059,130 individuals, including 11,931 delirium cases.
-
For the mediation analysis, n = 407,827 in the UKB EUR subcohort. For the sensitivity mediation analysis n = 141,864 in the UKB EUR subcohort.
-
For the MTAG, n = 846,034 individuals in the discovery set and n = 120,466 individuals in the replication MTAG.
-
For the proteomics analysis, n = 32,652 in the UKB EUR, including 541 delirium cases.
Data exclusions
Individuals were excluded if they were missing genotype, protein or phenotype/covariate data. Specific exclusion criteria are described in the ‘Discovery of genetic risk factors’ and ‘Proteomic study population’ sections.
Randomization and blinding
No new randomization and blinding were conducted due to the observational nature of the study.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Details for accessing individual-level data can be found at https://www.ukbiobank.ac.uk/enable-your-research/apply-for-access (UKB) and https://www.researchallofus.org/register (AoU Research Program). Details on obtaining delirium GWAS summary statistics used in this work can be found at https://www.finngen.fi/en/access_results (FinnGen R10 release) and https://precisionhealth.umich.edu/our-research/michigangenomics (MGI freeze 3). GWAS summary statistics generated in this work are publicly available via the University of Edinburgh’s Datashare service at https://doi.org/10.7488/ds/8014. Summary statistics for the proteomic, MR and colocalization analyses can be found in the Supplementary Tables file and Supplementary Data 2 and 3. Source data are provided with this paper.
Code availability
All software used in the present study is publicly available. The code used for all analyses in the study can be found on GitHub at https://github.com/VasiliosRaptis/deliriumGen.
References
Anand, A. & MacLullich, A. M. J. Delirium in older adults. Medicine 49, 26–31 (2021).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013).
Wilson, J. E. et al. Delirium. Nat. Rev. Dis. Prim. 6, 90 (2020).
Inouye, S. K., Westendorp, R. G. & Saczynski, J. S. Delirium in elderly people. Lancet 383, 911–922 (2014).
Gordon, E. H., Ward, D. D., Xiong, H., Berkovsky, S. & Hubbard, R. E. Delirium and incident dementia in hospital patients in New South Wales, Australia: retrospective cohort study. BMJ https://doi.org/10.1136/bmj-2023-077634 (2024).
Fong, T. G. & Inouye, S. K. The inter-relationship between delirium and dementia: the importance of delirium prevention. Nat. Rev. Neurol. 18, 579–596 (2022).
Watne, L. O. et al. Cerebrospinal fluid quinolinic acid is strongly associated with delirium and mortality in hip-fracture patients. J. Clin. Invest. 133, e163472 (2023).
Tsui, A. et al. Persistent delirium is associated with cerebrospinal fluid markers of neuronal injury. Brain Commun. 6, fcae319 (2024).
Krogseth, M. et al. Delirium, neurofilament light chain, and progressive cognitive impairment: analysis of a prospective Norwegian population-based cohort. Lancet Healthy Longev. 4, e399–e408 (2023).
Heneka, M. T. et al. Neuroinflammation in Alzheimer disease. Nat. Rev. Immunol. https://doi.org/10.1038/s41577-024-01104-7 (2024).
Leslie, D. L. & Inouye, S. K. The importance of delirium: economic and societal costs. J. Am. Geriat. Soc. https://doi.org/10.1111/j.1532-5415.2011.03671.x (2011).
Sepulveda, E. et al. The complex interaction of genetics and delirium: a systematic review and meta-analysis. Eur. Arch. Psychiatry Clin. Neurosci. 271, 929–939 (2021).
Massimo, L. et al. Genetic and environmental factors associated with delirium severity in older adults with dementia. Int. J. Geriat. Psychiatry 32, 574–581 (2017).
Van Munster, B. C. et al. Genetic polymorphisms in the DRD2, DRD3, and SLC6A3 gene in elderly patients with delirium. Am. J. Med Genet. B 153B, 38–45 (2010).
Ely, W. E. et al. Apolipoprotein E4 polymorphism as a genetic predisposition to delirium in critically ill patients. Crit. Care Med. 35, 112–117 (2007).
Kim, J. et al. Antipsychotics and dopamine transporter gene polymorphisms in delirium patients. Psychiatry Clin. Neurosci. 59, 183–188 (2005).
Van Munster, B. C., Korevaar, J. C., De Rooij, S. E., Levi, M. & Zwinderman, A. H. The association between delirium and the apolipoprotein E ε4 allele in the elderly. Psychiatr. Genet. 17, 261–266 (2007).
Van Munster, B. C., Zwinderman, A. H. & De Rooij, S. E. Genetic variations in the interleukin-6 and interleukin-8 genes and the interleukin-6 receptor gene in delirium. Rejuvenation Res. 14, 425–428 (2011).
Leung, J. M. et al. Apolipoprotein E e4 allele increases the risk of early postoperative delirium in older patients undergoing noncardiac surgery. Anesthesiology 107, 406–411 (2007).
Cunningham, E. L. et al. Observational cohort study examining apolipoprotein E status and preoperative neuropsychological performance as predictors of post-operative delirium in an older elective arthroplasty population. Age Ageing 46, 779–786 (2017).
Van Munster, B. C., Korevaar, J. C., Zwinderman, A. H., Leeflang, M. M. & De Rooij, S. E. J. A. The association between delirium and the apolipoprotein e epsilon 4 allele: new study results and a meta-analysis. Am. J. Geriatr. Psychiatry 17, 856–862 (2009).
Terrelonge, M. et al. KIBRA, MTNR1B, and FKBP5 genotypes are associated with decreased odds of incident delirium in elderly post-surgical patients. Sci. Rep. 12, 556 (2022).
Adamis, D., Meagher, D., Williams, J., Mulligan, O. & McCarthy, G. A systematic review and meta-analysis of the association between the apolipoprotein E genotype and delirium. Psychiatr. Genet. 26, 53–59 (2016).
Visscher, P. M. et al. 10 years of GWAS discovery: biology, function, and translation. Am. J. Hum. Genet. 101, 5–22 (2017).
Blauwendraat, C., Nalls, M. A. & Singleton, A. B. The genetic architecture of Parkinson’s disease. Lancet Neurol. 19, 170–178 (2020).
Orme, T., Guerreiro, R. & Bras, J. The genetics of dementia with Lewy bodies: current understanding and future directions. Curr. Neurol. Neurosci. Rep. 18, 67 (2018).
Andrews, S. J. et al. The complex genetic architecture of Alzheimer’s disease: novel insights and future directions. eBioMedicine 90, 104511 (2023).
McCoy, T. H., Hart, K., Pellegrini, A. & Perlis, R. H. Genome-wide association identifies a novel locus for delirium risk. Neurobiol. Aging 68, 160.e9–160.e14 (2018).
Heinrich, M. et al. Association between genetic variants of the cholinergic system and postoperative delirium and cognitive dysfunction in elderly patients. BMC Med Genomics 14, 248 (2021).
Westphal, S. et al. Genome-wide association study of myocardial infarction, atrial fibrillation, acute stroke, acute kidney injury and delirium after cardiac surgery – a sub-analysis of the RIPHeart-Study. BMC Cardiovasc. Disord. 19, 26 (2019).
Wiredu, K., Aduse-Poku, E., Shaefi, S. & Gerber, S. A. Proteomics for the discovery of clinical delirium biomarkers: a systematic review of major studies. Anesthesia Analgesia 136, 422–432 (2023).
Mosharaf, M. P., Alam, K., Gow, J. & Mahumud, R. A. Cytokines and inflammatory biomarkers and their association with post-operative delirium: a meta-analysis and systematic review. Sci. Rep. 15, 7830 (2025).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Turley, P. et al. Multi-trait analysis of genome-wide association summary statistics using MTAG. Nat. Genet. 50, 229–237 (2018).
Lumsden, A. L., Mulugeta, A., Zhou, A. & Hyppönen, E. Apolipoprotein E (APOE) genotype-associated disease risks: a phenome-wide, registry-based, case-control study utilising the UK Biobank. eBioMedicine 59, 102954 (2020).
Smith, L. H. & VanderWeele, T. J. Mediational E-values: approximate sensitivity analysis for unmeasured mediator-outcome confounding. Epidemiology 30, 835–837 (2019).
Tibshirani, R. Regression shrinkage and selection via the lasso. J. R. Stat. Soc. B 58, 267–288 (1996).
Meinshausen, N. & Bühlmann, P. Stability selection. J. R. Stat. Soc. B 72, 417–473 (2010).
Giambartolomei, C. et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet. 10, e1004383 (2014).
Zuber, V. et al. Combining evidence from Mendelian randomization and colocalization: review and comparison of approaches. Am. J. Hum. Genet. 109, 767–782 (2022).
Finan, C. et al. The druggable genome and support for target identification and validation in drug development. Sci. Transl. Med. 9, eaag1166 (2017).
Huang, K. et al. Small-cohort GWAS discovery with AI over massive functional genomics knowledge graph. Preprint at medRxiv https://doi.org/10.1101/2024.12.03.24318375 (2024).
Raulin, A.-C. et al. ApoE in Alzheimer’s disease: pathophysiology and therapeutic strategies. Mol. Neurodegeneration 17, 72 (2022).
Bowman, K. et al. Vitamin D levels and risk of delirium: a Mendelian randomization study in the UK Biobank. Neurology https://doi.org/10.1212/wnl.0000000000007136 (2019).
Xie, W. et al. CEND1 deficiency induces mitochondrial dysfunction and cognitive impairment in Alzheimer’s disease. Cell Death Differ. 29, 2417–2428 (2022).
Manavalan, A. et al. Brain site-specific proteome changes in aging-related dementia. Exp. Mol. Med 45, e39 (2013).
Schmukler, E. et al. Altered mitochondrial dynamics and function in APOE4-expressing astrocytes. Cell Death Dis. 11, 578 (2020).
Farrer, L. A. Effects of age, sex, and ethnicity on the association between apolipoprotein e genotype and Alzheimer disease: a meta-analysis. JAMA 278, 1349–1356 (1997).
Belloy, M. E. et al. APOE genotype and Alzheimer disease risk across age, sex, and population ancestry. JAMA Neurol. 80, 1284–1294 (2023).
Griswold, A. J. et al. Increased APOE ε4 expression is associated with the difference in Alzheimer’s disease risk from diverse ancestral backgrounds. Alzheimer’s Dement. 17, 1179–1188 (2021).
Bellou, E. et al. Age-dependent effect of APOE and polygenic component on Alzheimer’s disease. Neurobiol. Aging 93, 69–77 (2020).
Bonham, L. W. et al. Age-dependent effects of APOE ε4 in preclinical Alzheimer’s disease. Ann. Clin. Transl. Neurol. 3, 668–677 (2016).
Steen, J., Loeys, T., Moerkerke, B. & Vansteelandt, S. Medflex: an R package for flexible mediation analysis using natural effect models. J. Stat. Soft. https://doi.org/10.18637/jss.v076.i11 (2017).
Leighton, S. P. et al. Delirium and the risk of developing dementia: a cohort study of 12 949 patients. J. Neurol. Neurosurg. Psychiatry 93, 822–827 (2022).
Livingston, G. et al. Dementia prevention, intervention, and care: 2024 report of the Lancet standing Commission. Lancet 404, 572–628 (2024).
Edwards, D., Handsley, M. & Pennington, C. The ADAM metalloproteinases. Mol. Asp. Med. 29, 258–289 (2008).
Lambrecht, B. N., Vanderkerken, M. & Hammad, H. The emerging role of ADAM metalloproteinases in immunity. Nat. Rev. Immunol. 18, 745–758 (2018).
Bellenguez, C. et al. New insights into the genetic etiology of Alzheimer’s disease and related dementias. Nat. Genet. 54, 412–436 (2022).
Mattiola, I. et al. The macrophage tetraspan MS4A4A enhances dectin-1-dependent NK cell–mediated resistance to metastasis. Nat. Immunol. 20, 1012–1022 (2019).
Chen, J., Zhao, X., Huang, C. & Lin, J. Novel insights into molecular signatures and pathogenic cell populations shared by systemic lupus erythematosus and vascular dementia. Funct. Integr. Genomics 23, 337 (2023).
Saha, O. et al. The Alzheimer’s disease risk gene BIN1 regulates activity-dependent gene expression in human-induced glutamatergic neurons. Mol. Psychiatry https://doi.org/10.1038/s41380-024-02502-y (2024).
Foster, E. M., Dangla-Valls, A., Lovestone, S., Ribe, E. M. & Buckley, N. J. Clusterin in Alzheimer’s disease: mechanisms, genetics, and lessons from other pathologies. Front. Neurosci. 13, 164 (2019).
Poljak, A. et al. Quantitative proteomics of delirium cerebrospinal fluid. Transl. Psychiatry 4, e477 (2014).
Zhu, X.-C. et al. CR1 in Alzheimer’s disease. Mol. Neurobiol. 51, 753–765 (2015).
Roses, A. et al. Understanding the genetics of APOE and TOMM40 and role of mitochondrial structure and function in clinical pharmacology of Alzheimer’s disease. Alzheimer’s Dement. 12, 687–694 (2016).
Zhu, Z. et al. TOMM40 and APOE variants synergistically increase the risk of Alzheimer’s disease in a Chinese population. Aging Clin. Exp. Res. 33, 1667–1675 (2021).
Fong, T. G. et al. Biomarkers of neurodegeneration and neural injury as potential predictors for delirium. Int. J. Geriat. Psychiatry 39, e6044 (2024).
Fong, T. G. et al. Association of plasma neurofilament light with postoperative delirium. Ann. Neurol. 88, 984–994 (2020).
Van Munster, B. C. et al. Neuroinflammation in delirium: a postmortem case-control study. Rejuvenation Res. 14, 615–622 (2011).
Miao, Y., Wang, M., Cai, X., Zhu, Q. & Mao, L. Leucine rich α-2-glycoprotein 1 (Lrg1) silencing protects against sepsis-mediated brain injury by inhibiting transforming growth factor β1 (TGFβ1)/SMAD signaling pathway. Bioengineered 13, 7316–7327 (2022).
Oren, R. L. et al. Age-dependent differences and similarities in the plasma proteomic signature of postoperative delirium. Sci. Rep. 13, 7431 (2023).
Vasunilashorn, S. M., Dillon, S. T., Marcantonio, E. R. & Libermann, T. A. Application of multiple omics to understand postoperative delirium pathophysiology in humans. Gerontology 69, 1369–1384 (2023).
Peters Van Ton, A. M., Verbeek, M. M., Alkema, W., Pickkers, P. & Abdo, W. F. Downregulation of synapse-associated protein expression and loss of homeostatic microglial control in cerebrospinal fluid of infectious patients with delirium and patients with Alzheimer’s disease. Brain Behav. Immun. 89, 656–667 (2020).
Jujić, A. et al. Low levels of selenoprotein P are associated with cognitive impairment in patients hospitalized for heart failure. J. Cardiac Fail. https://doi.org/10.1016/j.cardfail.2024.01.010 (2024).
Berasain, C. & Avila, M. A. Amphiregulin. Semin. Cell Dev. Biol. 28, 31–41 (2014).
Hong, Y. et al. Sepsis-associated encephalopathy: from pathophysiology to clinical management. Int. Immunopharmacol. 124, 110800 (2023).
Zaiss, D. M. W., Gause, W. C., Osborne, L. C. & Artis, D. Emerging functions of amphiregulin in orchestrating immunity, inflammation, and tissue repair. Immunity 42, 216–226 (2015).
Hassan, R. et al. Mesothelin-targeting T cell receptor fusion construct cell therapy in refractory solid tumors: phase 1/2 trial interim results. Nat. Med. 29, 2099–2109 (2023).
Lawlor, P. G. & Bush, S. H. Delirium in patients with cancer: assessment, impact, mechanisms and management. Nat. Rev. Clin. Oncol. 12, 77–92 (2015).
Amgarth-Duff, I., Hosie, A., Caplan, G. & Agar, M. A systematic review of the overlap of fluid biomarkers in delirium and advanced cancer-related syndromes. BMC Psychiatry 20, 182 (2020).
Tzioras, M., Davies, C., Newman, A., Jackson, R. & Spires-Jones, T. Invited Review: APOE at the interface of inflammation, neurodegeneration and pathological protein spread in Alzheimer’s disease. Neuropathol. Appl. Neurobiol. 45, 327–346 (2019).
Reas, E. T. et al. APOE ε4-related blood–brain barrier breakdown is associated with microstructural abnormalities. Alzheimer’s Dement. 20, 8615–8624 (2024).
Serrano-Pozo, A., Das, S. & Hyman, B. T. APOE and Alzheimer’s disease: advances in genetics, pathophysiology, and therapeutic approaches. Lancet Neurol. 20, 68–80 (2021).
Yang, S.-T. et al. Accumulation of amyloid in cognitive impairment after mild traumatic brain injury. J. Neurol. Sci. 349, 99–104 (2015).
Koizumi, K. et al. Apoε4 disrupts neurovascular regulation and undermines white matter integrity and cognitive function. Nat. Commun. 9, 3816 (2018).
VanDusen, K. W. et al. The MARBLE study protocol: modulating APOE signaling to reduce brain inflammation, delirium, and postoperative cognitive dysfunction. J. Alzheimer’s Dis. 75, 1319–1328 (2020).
Nelson, M. R. et al. The support of human genetic evidence for approved drug indications. Nat. Genet. 47, 856–860 (2015).
Minikel, E. V., Painter, J. L., Dong, C. C. & Nelson, M. R. Refining the impact of genetic evidence on clinical success. Nature 629, 624–629 (2024).
Reay, W. R. & Cairns, M. J. Advancing the use of genome-wide association studies for drug repurposing. Nat. Rev. Genet. 22, 658–671 (2021).
Draganov, D. I., Stetson, P. L., Watson, C. E., Billecke, S. S. & La Du, B. N. Rabbit serum paraoxonase 3 (PON3) is a high density lipoprotein-associated lactonase and protects low density lipoprotein against oxidation. J. Biol. Chem. 275, 33435–33442 (2000).
Chang, Y.-H. et al. Statin use and delirium risk: an updated systematic review and meta-analysis. Am. J. Therapeutics 30, e326–e335 (2023).
Camps, J., Marsillach, J. & Joven, J. The paraoxonases: role in human diseases and methodological difficulties in measurement. Crit. Rev. Clin. Lab. Sci. 46, 83–106 (2009).
Grdic Rajkovic, M., Rumora, L. & Barisic, K. The paraoxonase 1, 2 and 3 in humans. Biochem. Med. https://doi.org/10.11613/BM.2011.020 (2011).
Schlomann, U. et al. ADAM8 as a drug target in pancreatic cancer. Nat. Commun. 6, 6175 (2015).
Shubbar, E. et al. High levels of γ-glutamyl hydrolase (GGH) are associated with poor prognosis and unfavorable clinical outcomes in invasive breast cancer. BMC Cancer 13, 47 (2013).
Li, Q., Yang, Z., He, X. & Yang, X. Comprehensive analysis of PILRΑ’s association with the prognosis, tumor immune infiltration, and immunotherapy in pan-cancer. Sci. Rep. 13, 14334 (2023).
Monroe, K. et al. PILRA regulates microglial neuroinflammation and lipid metabolism as a candidate therapeutic target for Alzheimer’s disease. Preprint at Research Square https://doi.org/10.21203/rs.3.rs-3954863/v1 (2024).
Ibitoye, T. et al. Delirium is under-reported in discharge summaries and in hospital administrative systems: a systematic review. Delirium https://doi.org/10.56392/001c.74541 (2023).
Sudlow, C. et al. UK Biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
The All of Us Research Program Genomics Investigators et al. Genomic data in the All of Us Research Program. Nature 627, 340–346 (2024).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518 (2023).
Zawistowski, M. et al. The Michigan Genomics Initiative: a biobank linking genotypes and electronic clinical records in Michigan medicine patients. Cell Genomics 3, 100257 (2023).
World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (WHO, 2004).
World Health Organization. International Classification of Diseases: Ninth Revision, Basic Tabulation List with Alphabetic Index (WHO, 1978).
Stuart-Buttle, C. D., Read, J. D., Sanderson, H. F. & Sutton, Y. M. A language of health in action: Read Codes, classifications and groupings. Proc. AMIA Annu. Fall Symp. 1996, 75–79 (1996).
Kuan, V. et al. A chronological map of 308 physical and mental health conditions from 4 million individuals in the English National Health Service. Lancet Digital Health 1, e63–e77 (2019).
Mbatchou, J. et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. 53, 1097–1103 (2021).
Kent, W. J., Baertsch, R., Hinrichs, A., Miller, W. & Haussler, D. Evolution’s cauldron: duplication, deletion, and rearrangement in the mouse and human genomes. Proc. Natl Acad. Sci. USA 100, 11484–11489 (2003).
Willer, C. J., Li, Y. & Abecasis, G. R. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26, 2190–2191 (2010).
Ning, Z., Pawitan, Y. & Shen, X. High-definition likelihood inference of genetic correlations across human complex traits. Nat. Genet. 52, 859–864 (2020).
Falconer, D. S. & Mackay, T. Introduction to Quantitative Genetics (Pearson, Prentice Hall, 2009).
Lee, S. H., Wray, N. R., Goddard, M. E. & Visscher, P. M. Estimating missing heritability for disease from genome-wide association studies. Am. J. Hum. Genet. 88, 294–305 (2011).
He, Y., Koido, M., Shimmori, Y. & Kamatani, Y. GWASLab: a Python package for processing and visualizing GWAS summary statistics. Preprint at Jxiv https://doi.org/10.51094/jxiv.370 (2023).
VanderWeele, T. J. & Ding, P. Sensitivity analysis in observational research: introducing the E-value. Ann. Intern. Med. 167, 268–274 (2017).
Lyall, D. M. et al. Cognitive Test Scores in UK Biobank: data reduction in 480,416 participants and longitudinal stability in 20,346 participants. PLoS ONE 11, e0154222 (2016).
Fawns-Ritchie, C. & Deary, I. J. Reliability and validity of the UK Biobank cognitive tests. PLoS ONE 15, e0231627 (2020).
Townsend, P. Deprivation. J. Soc. Pol. 16, 125–146 (1987).
Quan, H. et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 173, 676–682 (2011).
Quan, H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 43, 1130–1139 (2005).
Sun, B. B. et al. Plasma proteomic associations with genetics and health in the UK Biobank. Nature 622, 329–338 (2023).
Chen, E. Y. et al. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinform. 14, 128 (2013).
Milacic, M. et al. The Reactome Pathway Knowledgebase 2024. Nucleic Acids Res. 52, D672–D678 (2024).
Liberzon, A. et al. The Molecular Signatures Database hallmark gene set collection. Cell Syst. 1, 417–425 (2015).
Kanehisa, M. KEGG: Kyoto Encyclopedia of Genes and Genomes. Nucleic Acids Res. 28, 27–30 (2000).
Friedman, J., Hastie, T. & Tibshirani, R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Soft. 33, 1–22 (2010).
Lever, J., Krzywinski, M. & Altman, N. Classification evaluation. Nat. Methods 13, 603–604 (2016).
DeLong, E. R., DeLong, D. M. & Clarke-Pearson, D. L. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44, 837–845 (1988).
Purcell, S. M. & Chang, C. C. PLINK v.1.9 (11 Dec 2023); www.cog-genomics.org/plink/1.9/
Sanderson, E. et al. Mendelian randomization. Nat. Rev. Methods Prim. 2, 6 (2022).
Skrivankova, V. W. et al. Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization: the STROBE-MR statement. JAMA 326, 1614–1621 (2021).
Hartwig, F. P., Davies, N. M., Hemani, G. & Davey Smith, G. Two-sample Mendelian randomization: avoiding the downsides of a powerful, widely applicable but potentially fallible technique. Int. J. Epidemiol. 45, 1717–1726 (2016).
Bowden, J. et al. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: the role of the I2 statistic. Int. J. Epidemiol. https://doi.org/10.1093/ije/dyw220 (2016).
Burgess, S., Butterworth, A. & Thompson, S. G. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 37, 658–665 (2013).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife 7, e34408 (2018).
Bowden, J., Davey Smith, G. & Burgess, S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44, 512–525 (2015).
Greco M, F. D., Minelli, C., Sheehan, N. A. & Thompson, J. R. Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat. Med. 34, 2926–2940 (2015).
Bowden, J. et al. Improving the accuracy of two-sample summary-data Mendelian randomization: moving beyond the NOME assumption. Int. J. Epidemiol. 48, 728–742 (2019).
Berisa, T. & Pickrell, J. K. Approximately independent linkage disequilibrium blocks in human populations. Bioinformatics 32, 283–285 (2016).
De Leeuw, C. A., Mooij, J. M., Heskes, T. & Posthuma, D. MAGMA: generalized gene-set analysis of GWAS data. PLoS Comput. Biol. 11, e1004219 (2015).
Acknowledgements
This work used the Edinburgh Compute and Data Facility (http://www.ecdf.ed.ac.uk/). This research has been conducted using the UKB Resource projects 788 and 44986. This work uses data provided by patients and collected by the UK NHS as part of their care and support. UKB has approval from the North West Multicentre Research Ethics Committee as a Research Tissue Bank approval. We gratefully acknowledge AoU participants for their contributions, without whom this research would not have been possible. We also thank the NIH’s AoU Research Program for making available the participant data examined in this study. We acknowledge the participants and investigators of the FinnGen study. We acknowledge the MGI participants, Precision Health at the University of Michigan, the University of Michigan Medical School Central Biorepository and the University of Michigan Advanced Genomics Core for providing data and specimen storage, management, processing and distribution services, and the Center for Statistical Genetics in the Department of Biostatistics at the School of Public Health for genotype data curation, imputation and management in support of the research reported in this publication. This research was funded by the Legal & General Group (research grant to establish the independent Advanced Care Research Centre at University of Edinburgh). The funder had no role in the conduct of the study, interpretation or the decision to submit for publication. The views expressed are those of the authors and not necessarily those of Legal & General. This work was supported by Vivensa Foundation (grant number PDM2202\40). For the purpose of open access, the author has applied a CC-BY public copyright licence to any author-accepted manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
V.R., A.T. and T.I.C. conceived and designed the study. V.R. and Y.B. performed the analyses. V.R and A.M.J.M. wrote the paper. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks Qile Dai, Elisabet Vilella and the other, anonymous, reviewer(s) for their contribution to the peer review of this work
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Age distribution of participants in UKB and AoU.
Age of all samples used in the GWAS (n_UKB = 407,827; n_AoU = 240,158) grouped by delirium status are shown in histograms (a) and (c) for UKB and AoU respectively. Prevalence of delirium first event (blue) and all-cause dementia (brown) by age bracket is shown in (b) and (d) for UKB and AoU respectively. Numbers above bars denote total number of delirium and all-cause dementia diagnosed individuals within each age bracket respectively. UKB: UK Biobank; AoU: All of Us Research Programme.
Extended Data Fig. 2 Manhattan plot of delirium GWAS in UKB EUR, conditional on APOE-ε4 haplotype count.
(Left) Each point represents a genetic variant. The x-axis denotes the variant’s genomic position and the y-axis the GWAS association p value. The gray dashed line denotes the genome-wide significance p value threshold 5×10−8. The closest gene in which the lead significant variant is located is annotated. Orange color highlights loci ±1,000 kb around lead variants. n_cases = 7,176; n_controls = 385,096. (Right) QQ-pot of GWAS observed vs. expected p values. ADAM32: ADAM metallopeptidase domain 32; λgc: genomic inflation factor. The plot was created using the GWASLab python package.
Extended Data Fig. 3 Manhattan plot of delirium GWAS in UKB EUR, conditional on all-cause dementia status.
(Left) Each point represents a genetic variant. The x-axis denotes the variant’s genomic position and the y-axis the GWAS association p value. The gray dashed line denotes the genome-wide significance p value threshold 5×10−8. The closest gene in which the lead significant variant is located is annotated. Orange color highlights loci ±1,000 kb around lead variants. n_cases = 7,176; n_controls = 385,096. (Right) QQ-pot of GWAS observed vs. expected p values. APOC1: apolipoprotein C1; SEC14L1: SEC14 like lipid binding 1; λgc: genomic inflation factor. The plot was created using the GWASLab python package.
Extended Data Fig. 4 Manhattan plot of delirium GWAS in UKB EUR, stratified by all-cause dementia status.
Results for the dementia (n_cases = 2,561; n_controls = 5,374) (left) and non-dementia (n_cases = 4,614; n_controls = 379,642) (right) sub-cohorts. Each point represents a genetic variant. The x-axis denotes the variant’s genomic position and the y-axis the GWAS association p value. The red dashed line denotes the genome-wide significance p value threshold 5×10−8. The plot was created using the qqman R package.
Extended Data Fig. 5 Manhattan plots of delirium GWAS in UKB EUR, stratified by Alzheimer disease status.
Results for the AD (n_cases = 1,142; n_controls = 2,424) (left) and non-AD (n_cases = 6,033; n_controls = 382,592) (right) sub-cohorts. Each point represents a genetic variant. The x-axis denotes the variant’s genomic position and the y-axis the GWAS association p value. The red dashed line denotes the genome-wide significance p value threshold 5×10−8. The plot was created using the qqman R package. AD: Alzheimer disease.
Extended Data Fig. 6 Manhattan plot of delirium GWAS in UKB EUR, on participants aged 60 years or older.
(n_cases = 6,955; n_controls = 335,567). Each point represents a genetic variant. The x-axis denotes the variant’s genomic position and the y-axis the GWAS association p value. The red dashed line denotes the genome-wide significance p value threshold 5×10−8. The plot was created using the qqman R package.
Extended Data Fig. 7 Mediation analysis of APOE-ε4 on delirium, mediated by all-cause dementia, with additional covariates.
(a) Hypothesized directed acyclic graph, showing all-cause dementia as mediator of APOE-e4 genetic effect on delirium (black arrows), adjusted for baseline covariates: age, sex, Charlson comorbidity index, general cognitive ability and Townsend deprivation index (gray arrows). (b,c) Effect decomposition of the total APOE-ε4 effect, into natural direct (independent of dementia) and natural indirect (mediated through dementia) effects ± 95% confidence intervals (n = 141,864 individuals in UK Biobank). (b) shows the effect of having one APOE-ε4 haplotype, and (c) the effect of having two APOE-ε4 haplotypes, compared to having none. OR: odds ratio. NDE: natural direct effect; NIE: natural indirect effect.
Extended Data Fig. 8 Proteomic predictive performance on the dementia-free test set.
Receiver Operating Characteristic (ROC) (a) and Precision–Recall (PR) curves (b) showing performance metrics of different models for predicting incident delirium on the held-out test set (n_cases = 105; n_controls = 6,378). The ‘proteomic’ logistic regression model is fit with the 14 stability-selected proteins, the ‘basic’ model is fit using only age at protein collection, sex and BMI and the ‘proteomic+basic’ includes both. The ‘APOE+proteomic+basic’ model additionally includes APOE-ε4 haplotype count as predictor. The dotted black lines indicate the performance of a randomly classifying model, that is the diagonal of the ROC curve (a) and the disease prevalence horizontal line in the PR curve (b). AUC: Area Under the Curve. ROC and PR plots and AUC calculations are made using the yardstick R package (v1.3.0).
Supplementary information
Supplementary Information
Supplementary Table 18.
Supplementary Tables
Supplementary Tables 1–17.
Supplementary Data 1
Table 1 summary statistics.
Supplementary Data 2
Full colocalization results.
Supplementary Data 3
cis-pQTLs summary statistics.
Source data
Source Data Figs. 2 and 4–7 and Extended Data Figs. 7 and 8
Statistical source data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Raptis, V., Bhak, Y., Cannings, T.I. et al. Dissecting the genetic and proteomic risk factors for delirium. Nat Aging 6, 235–251 (2026). https://doi.org/10.1038/s43587-025-01018-6
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s43587-025-01018-6